Family doctors are seeing fewer patients in person than they did last year, despite the hugely successful vaccine rollout, better Covid treatments and a more stable supply of PPE.
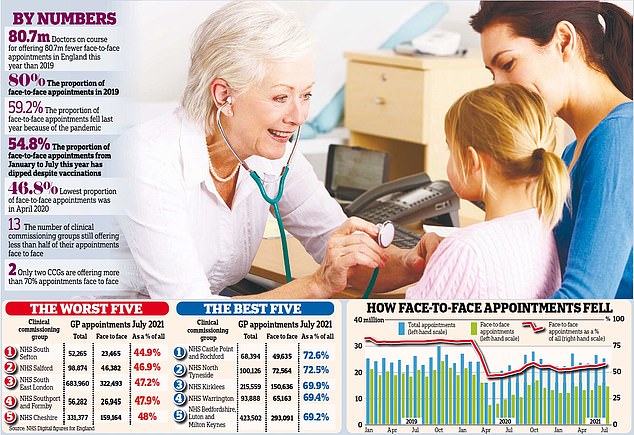
Shocking NHS figures reveal that patients were in the same room as their medic for just 54.8 per cent of consultations between January and July. That compares with 59.2 per cent last year, 80 per cent in 2019 and 82 per cent in 2018.
The rest are conducted by telephone or video. However, this category also includes consultations at a patient’s home, which are extremely rare.
The figures also reveal that the figure for face-to-face appointments fell below 50 per cent during the lockdowns. GPs are on course to see 80 million fewer people face-to-face this year than in 2019, raising fears that more life-threatening conditions will be missed.
NHS England told surgeries in May to ensure they were offering face-to-face appointments to any patient who requests one.
Stats show GPs are seeing even fewer patients face-to-face this year than they did in 2020
But rates have crept up only marginally since, from 55.6 per cent that month to 57.2 per cent in July – still almost a third lower than pre-pandemic levels.
And the figures expose a postcode lottery of care, with just two local health areas – known as clinical commissioning groups – offering more than seven in ten appointments face to face.
NHS Castle Point and Rochford CCG topped the list with a rate of 72.6 per cent in July. But 13 CCGs are failing to offer even half of their appointments in person, with NHS South Sefton at the bottom of the league table on 44.9 per cent.
Dennis Reed, the director of Silver Voices, a campaign group for the over-60s, is leading calls for patients to be given a legal right to ‘timely face-to-face GP appointments’. His petition on the official Government website has more than 16,000 signatures and will be considered for a debate in Parliament if it reaches 100,000. A survey of more than 500 elderly people by the campaign group in May found 71 per cent had struggled to obtain a face-to-face appointment.

And the figures expose a postcode lottery of care, with just two local health areas – known as clinical commissioning groups – offering more than seven in ten appointments face to face [File photo]
Mr Reed said: ‘If you can get through to your GP surgery on the phone you’ll be interrogated by a receptionist and have to jump through so many hoops to get an appointment. Many elderly people find this so daunting that they have just given up trying and are suffering at home. It’s very worrying and stressful for them.’
Mr Reed added: ‘We are worried that serious conditions are going undiagnosed, people are getting sicker and dying as a result. Ministers must get a grip on this now.’
Face-to-face GP appointments hit a low of 46.8 per cent in April 2020, the first full month after the first lockdown.
They remained below 50 per cent until August that year and have been above that level ever since.
But they are yet to return above 60 per cent in any month.
Lucy Watson, chairman of the Patients Association, said its helpline received regular calls from ‘frustrated’ and ‘distressed’ patients who can not see their GP face to face, and numerous health charities have warned of the harms of remote consultations.
Diabetes UK said it was ‘vital that those who weren’t able to access remote appointments were able to request face-to-face support’. Asthma UK said: ‘While some people with asthma may prefer phone and video doctors’ appointments because they can be more convenient, the majority have told us that they prefer face-to-face care. Some aspects of asthma care are currently more effective if delivered in person – for example, checking that someone is using their inhaler properly.’
And the Stroke Association said: ‘Some stroke survivors, particularly those with speech and communication difficulties like aphasia, have found online appointments challenging and felt it negatively affected the care they received. It is vital that stroke survivors have choices about how they access services in future, so they can receive the personalised support that best suits them.’ Professor Martin Marshall, chairman of the Royal College of GPs, said family doctors shared patients’ ‘frustrations’ with primary care.

Many patients are still being given Zoom consultations despite NHS England sayin in May that anyone who wants to be seen face-to-face should be
He insists GPs have offered face-to-face appointments when needed but admits some have at times felt like they were working in a call centre, ‘which isn’t the job they signed up for’. He added that the real problem was a chronic shortage of GPs, which limited the total number of appointments available.
Professor Marshall said the move to ‘mainly’ remote consultations was in line with government guidelines, adding: ‘This was necessary for infection control and to keep patients – and GP teams – as safe as possible. Face-to-face appointments and physical examinations have continued throughout, wherever clinically appropriate and safe to do so.’
Dr Richard Vautrey, chairman of the BMA’s GP committee, said patients were seen in person when it is safe and clinically appropriate. He added that it had been necessary to cut back numbers to protect the public during the pandemic and the need to limit the spread of coronavirus remained.
‘Patients don’t want to come into the surgery with one illness, only to leave having caught Covid-19 as well. To protect our patients, we had to limit the number of people coming through our doors.’
Source link : https://www.dailymail.co.uk/news/article-10007765/Pandemic-caused-plunge-numbers-saw-GP-year-set-worse-last.html











