Telling GPs to ‘think twice’ about prescribing opioids may prevent tens of thousands of patients from getting hooked on them, research suggests.
Experts have for years warned Britain is on track for a US-style opioid crisis, with the number of strong painkiller prescriptions dished out having doubled over the past two decades.
Officials have tried cracking down on the prescription of the drugs – such as codeine and Tramadol – among concerns about addition and dependence.
But a simple messaging campaign tailored specifically at GPs could help tackle the problem, according to academics at the University of Leeds.
It was trialled in West Yorkshire and led to 15,000 fewer patients prescribed opioids over the course of a year. And the campaign saved the NHS £700,000, calculations suggested.
If rolled out nationally, the experts estimated it could lead to 406,000 fewer people getting prescribed the powerful drugs. And it would save the health service around £18.5million.
The ‘feedback’ intervention gave GPs updates every other month on the number of people at their practice being prescribed opioids.
Family doctors enrolled in the trial were reminded of the need to be cautious about starting people on opioids.
And they were sent ‘persuasive messaging’ and asked to review whether to take people off the drugs when they provided no benefit.
From 1998 to 2018, the number of opioids prescriptions issued by GPs in England more than doubled. The NHS now spends more than £260million per year on the drugs.
Meanwhile, rates have only fallen slightly in America over the past decade ‘despite increased awareness of the risks and opioid abuse’, researchers said.

Opioids – such as morphine, fentanyl and codeine – are morphine-based medicines that can result in addiction, dependency and overdose. From 1998 to 2018, the number of opioids prescriptions issued by GPs in England more than doubled, prompting concerns the UK is in an ‘opioid epidemic’
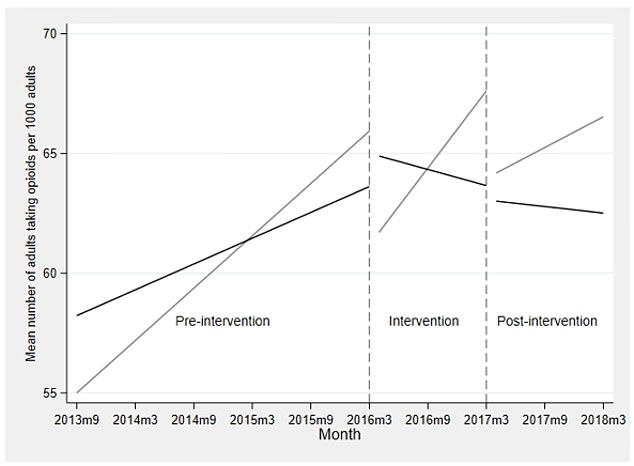
The graph shows the average number of adults prescribed opioid per 1,000 adults from 2013 to 2018. The grey line represents the GP practices that did not engage with the ‘think twice’ campaign, while the black line represents those who did, which were in West Yorkshire. These practices received updates every two months on their opioid prescribing rates. The graph shows the opioid use rate was rising from 2013 to 2016. But when the campaign was put in place in 2016, rates fell among participating practices, while they continued to rise in non-participating surgeries. And after the year-long study, rates continued to drop in the West Yorkshire practices, but at a slower rate
Opioids are often given as painkillers, but the Royal College of Anaesthetists warns there is ‘little evidence’ they help with long-term chronic pain.
And guidance from the National Institute for Health and Care Excellence (NICE), which issues information for healthcare professionals, states patients with long-term pain should not be started on opioids.
Researchers said doctor’s prescribing patterns are to blame for the hike, rather than patients’ needs.
HOW AMERICA GOT HOOKED ON OPIOIDS
Prescription opioids and illicit drugs have become incredibly pervasive throughout the US, and things are only getting worse.
In the early 2000s, the FDA and CDC started to notice a steady increase in cases of opioid addiction and overdose. In 2013, they issued guidelines to curb addiction.
However, that same year – now regarded as the year the epidemic took hold – a CDC report revealed an unprecedented surge in rates of opioid addiction.
Overdose deaths are now the leading cause of death among young Americans – killing more in a year than were ever killed annually by HIV, gun violence or car crashes.
In 2019, the CDC revealed that nearly 71,000 Americans died from drug overdoses.
This is up from about 59,000 just three years prior, in 2016, and more than double the death rate from a decade ago.
It means that drug overdoses are currently the leading cause of death for Americans under 50 years old.
The data lays bare the bleak state of America’s opioid addiction crisis fueled by deadly manufactured drugs like fentanyl.
Advertisement
They said patients have a ‘strong expectation’ that GPs can dish out pain relief, which adds to pressure to prescribe them.
There are also ‘large differences’ in opioid prescribing between different practices, suggesting it is driven by clinician habits.
The longer people take the drugs for, the more their body learns to tolerate them and the higher doses they have to take the produce the right effect.
It also becomes harder and harder to stop taking them and, once the body becomes addicted, suddenly stopping them can have deadly effects.
Researchers trialled the Campaign to Reduce Opioid Prescribing in 2016 at 316 GP surgeries in the West Yorkshire region, which serve 2.2million people. The medics compared the practice to 130 unnamed GP surgeries.
In the months leading up to the trial, the number of patients prescribed opioids at the West Yorkshire surgeries was 58.1 per 1,000 adult patients and rising by 0.18 per 1,000 each month.
And the rate was 62.2 per 1,000 patients among the other group and increasing by 0.36 per 1,000 patients every month.
Patients with cancer – who use the drugs to relieve pain – or drug dependency were not included in the figures.
The study, published in PLOS Medicine, found after the trial was implemented, rates fell in West Yorkshire.
Some 0.11 fewer patients per 1,000 were being prescribed opioids each month, they calculated. Experts argued the drop was ‘modest’ but insisted it was ‘substantial’ at a population level.
Meanwhile, the rate of prescribing increased among the non-participating practices by 0.54 per 1,000 patients.
Dr Sarah Alderson, a GP in Holmfirth, West Yorkshire, who led the study, said: ‘Our analysis shows the intervention was particularly effective at getting GPs to stop or reduce their prescribing for those groups at high risk such as older patients or those who also had a mental health condition.
‘The study shows GPs can be highly effective in identifying other ways of supporting patients who experience chronic pain.
‘The feedback intervention could easily be adapted and delivered elsewhere at relatively low cost.’
But the experts noted the declining rates opioid prescription rates among participating practices started to slow once they stopped received updates from the researchers.
So Dr Alderson said the campaign needs to be sustained over a longer time period.
Dr Tracey Farragher, epidemiologist at the University of Manchester and analyst on the study, said: ‘This study is a great example of how health records can improve patient care by providing up to date information to doctors about how many of their patients are being prescribed opioids.’
Source link : https://www.dailymail.co.uk/health/article-10056617/GPs-told-think-twice-dishing-powerful-opioid-drugs.html











