Ever since I was young, I knew I wanted to have children — a large brood of little ones, with all the squabbles and exhaustion and love that brings. When I started dating my now-wife, Anya, in 2004, we knew we were too old — I was 32, she was 33 — to waste time on a relationship where the other wanted a completely different life.
So we talked early on about the important stuff, and I told her I could happily compromise on everything else but I needed to have children. Then, when we started talking about getting married, she sat me down for a chat.
‘Look,’ she said, ‘I don’t want to put pressure on you, but biology means it’s going to get harder for me. I don’t want to end up on the other side of 40 and you say, “Let’s have kids”, and then I can’t get pregnant and we end up splitting up because of it.’
But I just didn’t take it in.
Anya and I worked together on my BBC travel documentaries, she filming and researching behind the scenes, while I was front of camera. We were travelling the world for up to six months a year.
I always thought the babies would come, but at an appropriate moment. They would be slotted into a schedule. Our schedule. Nature would play ball and fall in with our plans. How wrong I was. In the summer of 2008, after marrying the year before, we began trying for a child. For many months, we tried everything from hypnotherapy to having sex upside down.
Ever since I was young, I knew I wanted to have children — a large brood of little ones, with all the squabbles and exhaustion and love that brings
We even timed lovemaking to coincide with changes in Anya’s body temperature (women’s fertility starts to peak two or three days before ovulation, signposted by a slight change in body temperature), which is not an easy task when you’re on the road filming. It meant being intimate whenever and wherever we were, be it on a ferry, on an abandoned film set or up a mountain.
Eventually, after a year-and-a-half of trying [by then aged 37 and 38 respectively], we sought advice from pricey fertility experts. When Anya’s test results came back all clear, the spotlight turned on me.
I saw a male fertility specialist and filled in long documents detailing my lifestyle and my nutritional intake, or the lack thereof, before giving a sperm sample for testing.
Then I found myself sitting in a private fertility clinic in London, where I heard the worst news I could have imagined.
The fertility specialist bustled in and sat down with my notes. She had a cool manner, like a headmistress, but perhaps she was just unwilling to comfort me with inappropriate warmth.
‘I’ve got your test results,’ she said, ‘and I think you should prepare yourself for some bad news. I won’t make any bones about it,’ she tapped the papers. ‘I’m very sorry to have to tell you, but you are basically infertile.’
I would not be able to have children. It was the starkest of messages: I could hardly take it in.
She told me I had loads of sperm but their morphology was terrible. We’d never heard the term before.

When I started dating my now-wife, Anya, in 2004, we knew we were too old — I was 32, she was 33 — to waste time on a relationship where the other wanted a completely different life
‘Your sperm are deformed,’ said the headmistress, looking over her glasses at me. ‘They will never be able to break into Anya’s eggs.’
She started listing different figures from my sperm test. I had 0 per cent normal sperm. Zero. Nothing. They had also checked sperm motility. My sperm were swimming around in circles, or moving energetically without going anywhere. Ironically enough, considering my day job, they were not good travellers.
‘But surely,’ Anya said, ‘there’s something we could do? He works all hours, eats fairly badly, doesn’t get enough sleep. He could have earlier nights, live more healthily.’
The headmistress shook her head. ‘I’m sorry, but no,’ she said. ‘I don’t want to give you unrealistic levels of hope.’ She was adamant that morphology is one of the hardest things to improve. I was quickly lost to my fears and remember swaying in my seat. It felt I had been deprived at a stroke of my very reason for being.
I’d already had an awareness of what it would mean to miss out on having my own family, and had told Anya that unless I could have children I was very likely to go mad. I didn’t think I would be able to cope with life if I couldn’t become a father.
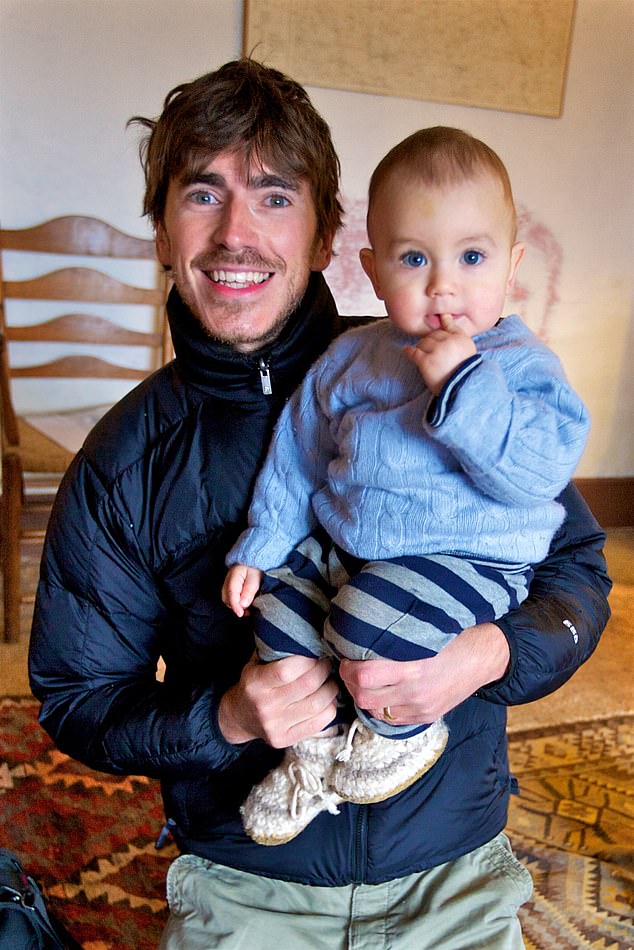
But there seemed to be no way around the specialist’s verdict. Natural conception was impossible. I was told there was no chance that I could have my own baby. My sperm were not viable. They were bloody useless. Yet despite this doomsday prediction, today Anya and I have a son, Jake, who’s now aged ten. He is the centre of our world, beloved beyond all measure.
How did this happen? Well, despite what the specialist told us, I was able to transform my fertility through sensible, practical measures, along the lines that Anya had suggested.
I overhauled my unhealthy diet. I exercised, doing intense British Military Fitness classes run by former Army instructors. I bought new underwear that let everything hang loose, and traded my way-too-tight jeans for combat trousers. I even tried sitting on a rubber ring that was supposed to give my undercarriage some space. Seriously. I wanted to have a child and was happy to do anything.
And it worked. After just a few months following this new regimen, tests showed the headmistress had been wrong. While my results still weren’t amazing, my sperm were completely viable. I had a chance of becoming a father.
I realise this is intimate. I wasn’t sure whether I should write about such a thing, especially as my son will one day read this. But I want to be honest about what we went through because it might help someone else.
Because if you want to have children with a future partner, don’t imagine Mother Nature will be happy to twiddle her thumbs and, when you decide the time is right, dance to your tune.
I had no inkling that there was anything amiss with my fertility. It was only when I started looking at my lifestyle that I realised how much I was doing wrong.

Despite this doomsday prediction, today Anya and I have a son, Jake, who’s now aged ten. He is the centre of our world, beloved beyond all measure
Aside from my age, there were all sorts of things to beat myself up about. Sperm are sensitive and are particularly badly affected by environmental factors such as heat, pollution and chemicals.
The expert had said many men who spend their days sitting at computers or driving taxis or lorries are effectively cooking their sperm.
Had I done the same with my trips to the Tropics and other exotic places for my television documentaries? I kept thinking of the time I had walked into a nuclear waste dump in Kyrgyzstan in Central Asia, wearing a full-face respirator and a biological and chemical warfare suit only a little thicker than a shower curtain.
The sun had roasted me inside the suit to the point where I thought I was going to collapse. I had to sit down, on top of the radioactive nuclear waste dump. Even at the time, I thought the physical proximity of my testicles, my reproductive organs, to the ground was A Very Bad Idea.
Then there were all those journeys where I’d squashed and squeezed myself into tiny vehicles and small planes in tropical corners of the world. I just couldn’t stop thinking that I had boiled or irradiated my own testicles.
It was desperately painful for me to accept that my travelling might have been part of the reason I was going to be unable to have a family, that my journeys made me a prime candidate for infertility all along.
Anya was also deeply upset, of course. But she was a lot calmer than me, and was sceptical about the sheer finality of the verdict. ‘We are not giving up — change is always possible,’ she would say, as I risked sinking into a miasma of depression.
So what was first to change? After that catastrophic verdict from the headmistress, we decided to go to our original fertility specialist, who was sympathetic and calming.
My sperm test results were definitely not good, she agreed. But she did offer a little light, saying that although we would not be able to conceive normally, or even with IVF, there were other options.
Had we thought about a sperm donor? Adoption? Fostering? Or it might be possible to inject my sperm directly into Anya’s eggs in a more complicated form of IVF called ICSI, rather than just ‘introducing’ them to each other in a petri dish.
But before any of that, she thought we should both see a nutritionist — in another oak-panelled room in another expensive private medical practice in the centre of London.
Kathy, the nutritionist, was much more positive and guided me through a total lifestyle reboot. She told me I had to dramatically reduce caffeine, chocolate, wine, sugar, salt and a lot more besides that made life tasty.
She prescribed berries for antioxidants and a healthy new diet. I started necking zinc tablets and other pill-sized treats, and later started taking Wellman fertility supplements.
We both saw acupuncturists and started our intense fitness classes. And as well as my roomier clothing, I was instructed to always sit with my legs apart to keep everything that mattered from overheating.
(Remembering this now, I am struck that it was Anya who also talked with our friends and asked around among other couples about their experiences with fertility. Like a stereotypical bloke, I pretty much clammed up. I’ve since changed. I now know that brooding in silence is the wrong way.)
We thought hard about travelling after my diagnosis. I asked the specialists whether I should give up the adventures, even though they weren’t just my life, they had become my living.

How did this happen? Well, despite what the specialist told us, I was able to transform my fertility through sensible, practical measures, along the lines that Anya had suggested
I was ready to stop travelling if it would seriously improve our chances of having a child. But they pointed out that leaving home behind was also a chance for Anya and I to put our troubles to one side, to clear our minds of stress, which might also be contributing to the problem.
‘Lots of people go somewhere exotic when they’re trying to conceive,’ said one of our fertility specialists with a cheeky smile.
So we restarted filming for our Tropic of Cancer documentary, travelling to southern Egypt, visiting the spectacular ancient ruins of Abu Simbel, built to honour Nefertari by her husband King Ramses II, a lucky blighter who managed to have more than 100 children.
While travelling, I also did three sets of 50 press-ups on my knuckles each morning, followed by three sets of 40 squats. I was an early adopter of resistance loop bands — essentially giant, thick, tough rubber bands that fit in a pocket but help to provide a workout almost anywhere, even, like a complete nutter, while sitting in a car as a passenger.
I also made changes to try to avoid plastic, both at home and when travelling. Keeping food in plastic containers was out. Takeaways in plastic boxes were ditched, too, and organic, unprocessed food was in.
I avoided scented household products and vinyl shower curtains. I swapped my plastic kettle for a metal one and stopped using plastic water bottles.
Why? Well, after doing some research, I found something fundamentally worrying is happening between our thighs.
Some experts believe the sperm counts of Western men have fallen by more than 50 per cent over recent decades, under attack by our modern world.

I had no inkling that there was anything amiss with my fertility. It was only when I started looking at my lifestyle that I realised how much I was doing wrong
Some have even labelled it ‘Spermageddon’. Our collective sperm count is falling, and the number of defective sperm seems to be growing. Like me, men are producing more deformed sperm, sperm with two heads or sperm that are static or listless rather than chasing energetically after a female egg.
It’s not just men: experts believe there is evidence of an increasing number of miscarriages among women of all ages, declining egg quality and more girls experiencing early puberty.
Experts believe this is largely down to endocrine-disrupting chemicals (EDCs), which can mimic and interfere with the hormones that regulate and run our bodies, blocking some hormones or tricking our fine-tuned systems into over- or under-responding in different ways.
EDCs are used in plastic and thousands of products, including cosmetics, toys, clothes, soft furnishings and pesticides. They are even used in the linings of many tinned foods to stop them corroding.
As far back as the year 2000, a Royal Society report pointed out: ‘It is prudent to minimise exposure of humans, especially pregnant women, to endocrine-disrupting chemicals.’ This is because EDCs can make their way into the womb and the foetus, passing the problem down to the next generation.
One senior epidemiologist has even suggested that the reproductive crisis could mean that by 2045 most couples will need assisted conception.
Clearly governments need to act — and they need to act fast. Until they do, my advice for anyone hoping, wanting or trying to have children is, for goodness sake, to take it seriously.
It was now 2010. We had continued trying naturally for a child, endlessly, but with no luck, and I went for more follow-up tests.
I felt a sense of resignation about my own chances but was really starting to enjoy the thought of adopting, perhaps from a country where I had seen the difficulties of life for those children who were orphaned or abandoned.
My tests came back and I remember opening the results while I was eating toast, keeping the letter almost at arm’s length, prepared for the bad news.
But as I glanced across the letter, I could see there were numbers where previously there had only been zeros. There had been a transformation.
My test results were now so good that IVF wasn’t necessary. My sperm had come back to life — and obviously we celebrated in
the only way possible. Then Anya had some tests that showed her fertility levels were dropping. Now she was the issue.
She went to see her GP, who explained that with IVF, at our age, we might have a one in four chance of conception during a monthly cycle — significantly better odds than trying naturally. The longer we left it, the longer the odds would become.
Perhaps if we had waited we might have got pregnant naturally. Or perhaps we would have tried for years more and nothing would have happened. We will never know.
In June that year, we began a cycle of IVF at Hammersmith Hospital, West London. It was definitely not an easy option, and Anya had to endure multiple injections of hormones. Meanwhile, I had to provide my crucial little elements.
Eventually, one Tuesday, our sperm and eggs were put together in a petri dish, and we bit our nails. We knew that the following 24 hours were critical.
On the Wednesday, the clinic called us to say that five eggs had fertilised. We punched the air in delight.
Rather than bunging them back into Anya immediately, the embryologists asked our permission to wait a few more days for them to become a larger bundle of cells called blastocysts.
Waiting a few more days would give them time to grow and strengthen, hopefully increasing the chance they would survive the transfer from dish to body.
But there were, they told us, huge risks. Wait and perhaps they might wither in the clinic. We waited. By Sunday, just one egg was still going strong. That tiny fertilised egg was a survivor, a fighter.
‘That’s our Spartan,’ said Anya.
It takes a while to find out whether an egg has survived the transfer. We knew that the odds were not in our favour. Two weeks later, we went on holiday to Denmark, where Anya’s family are from. One morning, Anya woke me and lifted up a pregnancy test stick and pointed at the line.
She was expecting a baby.
I was flooded with joy and hope to an extent that felt over-whelming. However much I tried to stay calm and keep a bloody lid on it, the elation was intense.
I was so thrilled, so ecstatic, so hopeful. It had seemed so impossible. I’d been told it was impossible. Could I really be this lucky?
In early August, we went for a scan and, like millions of other expectant parents, we heard the extraordinary, elemental, beautiful sound of a pea-sized heart beating loudly through tinny speakers. I wept.
Nine months later, a tiny baby was born.
However much I’d dreamt about that moment, even mythologised it in my head as a transformative rite of passage, I never anticipated the enormity of it. The strength of my love for Jake was unlike anything I had experienced before. I wasn’t remotely prepared for the moment it became a reality.
For all my deep belief in the gifts travel can offer, no experience around the planet, before or since, can match the power or thrill or beauty of having a child and becoming a parent.
It was an eclipse. It put all else into the shade.
It was the culmination of the most exciting, exhausting and bizarre journey of my life.
Extracted from Journeys To Impossible Places by Simon Reeve, published by Hodder on October 14 at £20. © Simon Reeve 2021. To order a copy for £18 (offer valid to October 19, 2021; UK P&P free on orders over £20), visit mailshop.co.uk/books or call 020 3308 9193. Simon will be in conversation at The Barbican on October 12. Visit fane.co.uk/simon-reeve
Source link : https://www.dailymail.co.uk/health/article-10058497/BBC-adventurer-SIMON-REEVE-describes-wife-achieved-miracle-longed-for.html











