More than 35million GP appointments have been ‘lost’ during the Covid pandemic, fuelling fears of a ticking time-bomb of late diagnoses.
NHS Digital data shows there were 12 per cent per cent fewer visits in England between March 2020 and January 2021 compared to the same period a year prior — down from 287.2m to 251.4m.
Experts fear missed appointments have led to a significant deterioration in patients’ health, missed cancers and the worsening of other conditions such as asthma and diabetes.
Cancer charities have warned the current ‘Covid-induced’ backlog could lead to at least 35,000 excess deaths.
The figures, published today, show that GP surgeries have fared better during the second wave than last spring.
For example, there were 8m fewer appointments year-on-year last April, during the first lockdown, compared to 2m missed during the second shutdown in November.
The NHS cancelled almost every service when the pandemic first took off last March, when scientists did not fully understand the threat of the disease and Brits were told not to visit their GP unless it was an emergency.
But officials came under criticism for the knock-on effect of delayed care on the nation’s health, and there was a concerted effort going forward to keep vital services up and running despite restrictions.
Today’s figures also show there were more than 3m ‘lost’ appointments this January, as GPs juggled routine care with the Covid vaccine roll-out and the NHS grappled with levels of the virus that surpassed the spring peak.
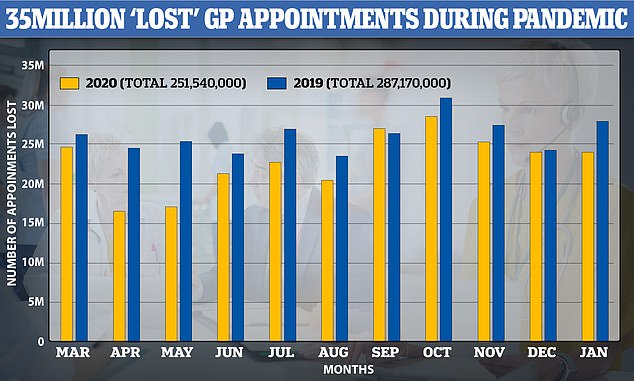
NHS Digital data shows there were 12 per cent per cent fewer visits in England between March 2020 and January 2021 compared to the same period a year prior — down from 287.2m to 251.4m

People have struggled to see a GP because of Covid-19 precautions that have moved a huge chunk of appointments online (file)
Professor Karol Sikora, a medical expert at the University of Buckinghamshire, told MailOnline: ‘Whist there may be a drop in trivial problems being brought to primary care there are two worrying gaps – cancer and heart disease.
‘Delays and failure to act on tests after hospital referral will only reduce the outcome for those patients. For cancer it will treatment more complicated and possibly increase significantly its side effects.
‘The politicians and their advisors have deliberately created a brainwashing strategy using fear as a weapon. This needs to rapidly reversed otherwise unnecessary lives will be lost.’
HOW THE NHS HAS STRUGGLED DURING THE PANDEMIC
Operation waiting lists are at an all-time high and cancer treatment is at a record-low as a result of the savage toll of the coronavirus pandemic on the NHS.
Experts have warned the country faces a future wave of health crises because so many people have had their care delayed.
WAITING LISTS FOR OPERATIONS
Some 4.5 million people in England are waiting for non-emergency surgery, the highest figure since records began in 2007.
And a total of 192,000 have been waiting more than a year for life-changing operations such as hip and knee replacements.
This is around a 160-fold increase since before the pandemic began in February, when just 1,163 had been waiting for a year.
The NHS waiting list data goes up only until the end of November – and doctors say the total will keep rising.
NHS England figures also show that at least 12,000 fewer heart operations than expected took place in England in the year to November 2020 – around one third lower than usual.
MISSED CANCER CARE
Separate figures show that during the first wave of the pandemic around 35,000 fewer people were diagnosed with cancer than would be expected.
Experts said the delays will cost lives, allowing tumours to grow and cancers to worsen.
The data from Public Health England’s National Cancer Registration and Analysis Service reveals 106,732 cases were diagnosed between April and September 2020, down from 142,324 the previous year.
STILLBIRTHS AND MISSED SMEARS
Other harrowing figures show the number of stillbirths in England almost doubled last spring, according to the Healthcare Safety Investigation Branch (HSIB), and at least 250,000 women are overdue their cervical smear tests as a result of the coronavirus pandemic, NHS figures show.
Advertisement
People have struggled to see a GP because of Covid-19 precautions that have moved a huge chunk of appointments online — face-to-face visits have plunged 40 per cent during the pandemic.
Social distancing and strict cleaning rules also mean family doctors can only see a fraction of the normal volume of patients in their practices.
Others have been scared off seeing their GP for fear of being a burden on the health service or catching Covid.
Professor Martin Marshall, chairman of the Royal College of GPs, said: ‘When the Covid-19 pandemic hit the UK, GPs and our teams swiftly transformed the way we delivered many of our services in order to keep staff and patients safe, and maintain infection control in surgeries, so it isn’t surprising to see this reflected in consultation data from the start of this year, compared to pre-pandemic.
‘When patients have needed face-to-face appointments, these have been facilitated in as safe a way as possible, and as this data shows, more than half of consultations in general practice are currently being conducted face-to-face.
‘One thing we are finding is much lower prevalence of common winter illnesses, such as colds and flu, which often makes up a high number of GP consultations at this time of year.
‘This is likely to be due to a combination of social distancing measures and lockdown restrictions, and a very high take-up of the flu vaccine, particularly amongst over-65s, which is our best protection against influenza.’
Today’s figures are the latest example of the damaging effects of brutal lockdown curbs on non-Covid care.
Separate data has shown operation waiting lists are at an all-time high and cancer treatment is at a record-low.
Some 4.5million people in England are waiting for non-emergency surgery, the highest figure since records began in 2007.
And a total of 192,000 have been waiting over a year for life-changing operations such as hip and knee replacements.
This is around a 160-fold increase since before the pandemic began in February, when just 1,163 had been waiting at least 52 weeks.
The NHS waiting list data only goes up until the end of December – and doctors say the total could reach 10million by the time the pandemic is over.
NHS England figures also show that at least 12,000 fewer heart operations than expected took place in England in the year to November 2020 – around one third lower than usual.
Other figures show that during the first wave of the pandemic around 35,000 fewer people were diagnosed with cancer than would be expected.
Experts said the delays will cost lives, allowing tumours to grow and cancers to worsen.
The data from Public Health England’s National Cancer Registration and Analysis Service reveals 106,732 cases were diagnosed between April and September 2020, down from 142,324 the previous year.
Different harrowing figures show the number of stillbirths in England almost doubled last spring, according to the Healthcare Safety Investigation Branch (HSIB), and at least 250,000 women are overdue their cervical smear tests as a result of the coronavirus pandemic, NHS figures show.
Source link : https://www.dailymail.co.uk/news/article-9299021/More-35MILLION-GP-appointments-England-lost-pandemic.html











