Britain’s Kent Covid variant could be more infectious because people stay sicker for longer, scientists now believe.
More than 50 countries have already spotted the mutant B.1.1.7 strain, which evolved to become up to 70 per cent transmissible than the original virus.
But researchers from Harvard University believe it may actually be because it leaves patients infectious for longer.
They found patients infected with the new variant were ill for 13 days, compared with eight days for the original SARS-CoV-2 strain.
The study — not yet published in a medical journal — used data from 65 players and staff in the US National Basketball Association who had contracted Covid.
People normally only get a test when they have symptoms but the NBA test daily and continue to do so after a positive swab, to monitor the full extent of the virus.
The Kent variant was first detected in in September 2020 and its rapid spread across the country spooked No10 into tougher action in December.
As well as being more infectious, studies also suggest the variant is slightly deadlier. But all the evidence suggests current vaccines work against it.
What do we know about the Kent variant?
Name: B.1.1.7, formerly VUI-202012/01
Where did it come from? The variant was first found in Kent and can be traced back to September 2020. Scientists noticed that it was spreading in November and it was revealed to the public in December.
What makes it new? The variant, which is a version of the SARS-CoV-2 coronavirus that causes Covid-19, has a series of mutations that change the shape of the spike protein on its outside. The main one is known as N501Y. This appears to make it better able to stick to the cells inside the body and makes it more likely to cause infection and faster to spread.
How did that happen? Viruses, particularly ones spreading so fast and in such huge numbers, mutate all the time. To reproduce they basically force living cells to copy and paste the viral genetic code, and this can contain errors that lead to slightly different versions of the virus. Often these mutations make no difference but, if they make the virus stronger, they can stick around for further generations and become the norm.
What can we do about it? Nothing much. People who catch the virus won’t know which type they have, and it will still cause the same symptoms and illness. Officials can try to contain it by locking down the areas where it is most prevalent, but if it is stronger than other versions of the virus it will eventually spread everywhere and become dominant as long as people continue to travel.
Will our vaccines still work? Yes, it’s very likely they will. Scientists on SAGE are fairly sure the mutations the Kent variant carries do not significantly affect how well the immune system can handle it. People who have a vaccine modelled on an older version of the virus, or who have been infected with Covid-19 before, are likely to be immune to it. This is because the main mutations are only on one part of the spike protein, whereas the immune system is able to target various other parts of the virus.
Advertisement
Eric Topol, director of the Scripps Research Translational Institute in California, told The Times they first thought the extra infectiousness of the UK variant was because of a ‘higher viral load’.
It’s thought that the amount of virus particles someone has inside them — known as the viral load — determines how sick they will be. Studies also suggest a high viral load makes people more likely to infect others.
However, the new data suggests it is related to ‘longer duration of infections’.
The study of the 65 players and staff found that the seven who were ill with the new variant were ill for 13 days.
In comparison, the 58 who were infected with the old strain were sick for eight days.
Those who tested positive with the old variant took two days from when Covid was detected to reach peak viral load and another six days until it was undetectable.
Meanwhile, those infected with the Kent variant took five days from when the virus was detected to reach peak viral load and then eight days until it could no longer be detected.
Dr Jenny Rohn, a biologist at University College London, told how the findings have ‘serious implications’ given the current quarantine period of 10 days.
It suggests Britons infected with the Kent variant – which is the most dominant strain in the UK – may need to quarantine for longer, if the findings are proven true in further studies.
Professor Sharon Peacock, head of the Covid-19 Genomics UK (Cog-UK) Consortium said the Kent variant ‘is going to sweep the world, in all probability’.
There are fears the variant has started to mutate further to become more like the one that evolved in South Africa, which is better able to resist immunity developed by past infection or from the current vaccines.
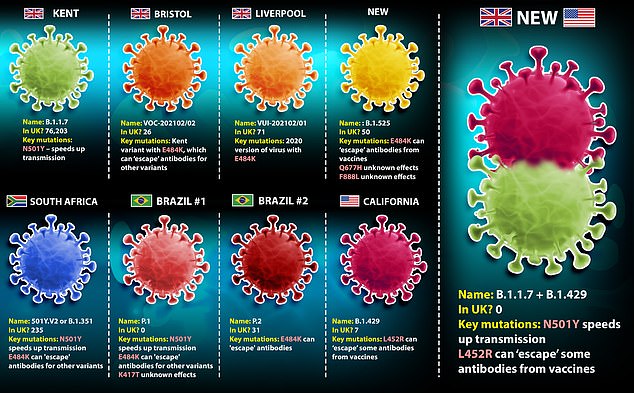
It comes after a hybrid version of coronavirus surfaced in California after the British Kent variant and a strain found in the US merged together inside an infected person.
The variant, not yet named, has only been spotted once but scientists fear there are likely to be more cases.
Experts are worried because it carries mutations which appear to make it able to spread faster and also to slip past some of the immunity made from past infections or vaccines.
It was formed from the Kent Covid variant and a Californian variant called B.1.429.
Scientists in the US claim they merged in a ‘recombination event’, the New Scientist reports. This happens when two different versions of the virus infect the same cell and then swap genes while they are reproducing, giving rise to a new variant.
Researchers have warned in the past that these events are possible but said they are ‘unlikely’ because they require very specific conditions and the coincidence of mostly uncontrollable events. They are more likely to happen during huge outbreaks.
HOW CAN VIRUSES COMBINE?
For a combined variant of the virus to emerge, one person must be infected with two strains of the coronavirus – likely from two separate sources – at the same time, and then the viruses must bump into each other inside the body.
Once the viruses are inside the body, the way they spread is by forcing human cells to make more of them.
The coronavirus is made up of genetic material called RNA and, to reproduce, it must force the body to read this RNA and make exact copies of it.
There are inevitably errors when this happens because it happens so fast and so often and natural processes are imperfect.
If two viruses are in the same place at once, both being duplicated by the same cells, there is a chance the RNA genes could be mixed up, just as there could be a mix-up if someone dropped two packs of cards at once and picked them all up.
Most places have dominant variants of the virus so someone getting infected with two is unlikely to begin with.
And, for healthy people, there is likely only a window of around two weeks before the body starts to develop immunity and successfully clear out the first version of the virus.
This risk window could be cut to days for the majority of people who develop Covid symptoms – which takes an average of five days – and then stay at home sick.
But huge, poorly controlled outbreaks like the ones in the UK and US over the winter, significantly raise the risk of the combination events simply because the number of infections is higher.
Advertisement
Source link : https://www.dailymail.co.uk/news/article-9273561/Kent-Covid-variant-sweeping-world-infectious-original-strain-scientists-say.html











