Three Covid patients at London’s NHS Nightingale Hospital died after being treated by ‘inexperienced’ staff using the wrong ventilator equipment during the first wave of the pandemic.
A total of ten patients were affected at the hospital in the ExCel Centre, Newham, East London, after staff left their intensive care ventilators without heat and moisture exchange (HME) filters.
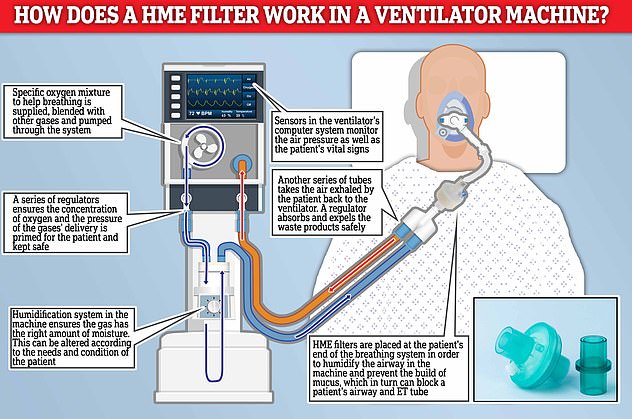
HME filters are placed at the patient’s end of the breathing system in order to humidify the airway in the machine and prevent the build of mucus, which in turn can block a patient’s airways and endotracheal (ET) tube.
But the staff error, which saw them use the wrong filter in the ventilation circuits instead, led to the breathing tubes in three patients becoming blocked and saw all of them ‘suffer harm’ and require re-intubation.
All three patients died after the incident occurred.
The findings are among a catalogue of issues that have emerged since the Nightingale, which was hailed as a solution to the growing crisis in hospital capacity amid the coronavirus crisis, was shut down last year after treating just 54 patients.
While it has not been determined whether the filter incidents contributed to the deaths, the same staff error occurred in all ten cases.
Key findings from the report:
Staff were unclear on the correct use of filters and their position in the ventilators – leading to the build up of mucus and blocked airways;Inexperienced staff were using anaesthetic machines, meant for operating theatres, and removing mucus from patients with limited training; Hospital had multiple filters available and it was not immediately obvious on sight which were the correct filters for the ventilator.
Among the patients to have been affected by the incident was Kishorkumar Patel, 58, a London bus driver, who was initially admitted to Northwick Park Hospital on April 4, 2020, after experiencing shortness of breath, coughing and fatigue.

Kishorkumar Patel, 58, from Sudbury, north west London, was initially admitted to Northwick Park Hospital on April 4, 2020, before he was transferred to the Nightingale Hospital in London

Mr Patel’s sister Ursha Lee (pictured), 55, from Wembley, was told there had been an error with the filter in her brother’s ventilator machine and this had caused his breathing tube to become blocked
The father-of-six, from Sudbury, north west London, who achieved a first-degree black belt in Kung Fu at the age of 55, was one of the first patients to be transferred to the ExCel centre for coronavirus treatment on April 7.
Mr Patel, who had no underlying health conditions, spent 19 days at the hospital before he died on April 26.
Seven days before his death, Mr Patel’s family were told an engineer at the hospital had discovered that the ET tube in his windpipe, which provides oxygen to a patient, was blocked as a result of an ‘incorrect filter’ in his ventilator.
A Serious Incident Report (SIR) sent to the family later described how medical staff discovered heat and moisture exchange filters had not been used in his intensive care ventilator – resulting in a lack of any humidification in the machine.
The incident would have ‘reduced effectiveness’ of the ventilator and ‘contributed to Mr Patel’s deterioration on April 19’, a letter to the family from Barts Health NHS Trust also added.
The health trust said an antiviral filter was used in place of the HME but have not been able to tell the family on what type of ventilator machine – a Penlon anaesthetic machine or a Draeger ICU ventilator – it was used on.
The SIR report also described how the blocked breathing tube was discovered just four days after Mr Patel suffered pulseless electrical activity (PEA) – a form of cardiac arrest – however it is still not clear if the blocked tube contributed to this.
A Barts Health spokesman claimed that despite ‘investigating the circumstances and changing their practices’ they ‘did not believe the filter was a direct cause of Mr Patel’s death’.
But the spokesman did not comment on whether it was a contributing factor in the death, and instead pointed to the upcoming inquest, which will be held on October 4.
Describing the day her brother was admitted to hospital, Mr Patel’s sister Ursha Lee, 55, from Wembley, said: ‘It all started with a WhatsApp message to my brother’s daughter. I had just asked her if she was well but all of a sudden I received a reply from her which read: ”Ambulance just took dad.”
‘Suddenly a barrage of feelings consumed me all at the same time. I just felt sheer panic, shock and worry.
‘My brother was not the type of person to seek help, so deep inside I knew he must have been in a serious condition to have accepted being taken to hospital.’
A day after he was admitted to hospital, Ms Lee and her family briefly spoke with Mr Patel over FaceTime and tried to provide him with some form of comfort.
Ms Lee continued: ‘It was a short call, only around 2-3 minutes, as he couldn’t talk due to having a shortness of breath and we didn’t want to tire him out.
‘We asked if he was ok and he simply gave us a thumbs up. This was undoubtedly a very frightening and daunting time for him to be alone in hospital without family.
‘There was a look he gave me that I remember to this day, something I had not seen from my brother’s eyes ever before. Something was just not right.
‘This phone call to him was to give some form of comfort. I wanted him to know that we were there for him and that he was not alone. I hope we provided that to him, even for a little while.’
On April 6, Ms Lee and her family received a call informing them her brother would be transferred to the Nightingale Hospital in London the following day.
She said: ‘We were told he was going to be transferred to the Nightingale Hospital on April 7. We felt like we had been thrown into that decision.
‘My family’s initially questioned this, especially as just the night before we had been told he was put on a ventilator. But it looked like there was no alternative to us. We at the time were just walking with what could have been a blindfold over our eyes. We couldn’t see him.

The father-of-six, who achieved a first-degree black belt in Kung Fu at the age of 55, was one of the first patients to be transferred to the ExCel centre on April 7


Mr Patel, who was a London bus driver, spent 19 days at the ExCel Centre before he died on April 26 of Covid. Pictured: Mr Patel on the N18 bus (left) and achieving his first-degree black belt in Kung Fu in 2017 (right)

The father was among the first patients to have been transferred to the Nightingale for coronavirus treatment in April last year. Pictured: Mr Patel with his children Sarita, Kiran, Zoe, Aakash, Shane and Anish
‘There was slight apprehension with him being sent to the Nightingale as it was a new hospital that we knew very little about and to add to that it was quite a distance from us.
‘But we just clung onto the positives because that is all we had to keep us going at the time – hope.’
Over the following the days Mr Patel was put on a ventilator and his family would receive daily calls from a telephone operator at the Nightingale about his health.
But they were not able to speak with members of staff directly involved in his care.
Ms Lee said: ‘I was filled with worry as I waited every day for a bit of news about my brother. Our only line of communication was to hear what was being conveyed to us over a phone line by an operator who was put in charge of transfers.
‘I remember watching the news on the day my brother was transferred, seeing patients being taken to the Nightingale by ambulance and just thinking ”I wonder if my brother is inside this ambulance and is he safe and well?”’
However on the evening of April 18, an engineer at the hospital discovered Mr Patel’s ET tube had become blocked with secretions due to an incorrect filter in his ventilator circuit.
Ms Lee and her family were called by the engineer the following day who told them the wrong filter had been used in Mr Patel’s breathing machine. They apologised for the incident and said a letter would be issued.
She said: ‘It was early morning on a Sunday when my nephew received a call from an engineer at the Nightingale telling him that wrong filters had been used on a series of ventilators – including my brother’s – and this had led to his breathing tube being blocked.
‘I remember that day quite clearly. I just thought this has got to quite serious for someone like an engineer to be calling us on a Sunday morning.
Ms Lee described her brother (pictured with his son Anish in 2004) as a simple and gentle man who had a humble soul
Key findings and critical actions required from the report
Key findings:
Anaesthetic machines were being used to provide ventilation to patients for long periods of time. The machines were being used for a function that they were not designed for.There was a lack of expertise within the clinical team working in the ICU – it was noted that non-anaesthetic ICU consultants were not familiar with the anaesthetic machines being used.The correct use of filters and their position within the circuit was complicated and may not have been clear to all ICU staff.There were multiple filers available for use with the machines and it was not immediately obvious on sight which filters were HME. Suctioning was undertaken by staff with limited expertise and the machines in use may not be as effective as standard ICU suction machines.There were different types of ventilators in place which may have contributed to potential confusion regarding what each patient needs.
Recommendations:
A checklist of the ventilator circuit is written and implemented at the start of every shift, to be completed by the anaesthetist and ODP to ensure correct circuit set up and humidification. Gain assurance that bedside nursing staff are clear on the mechanism for checking suction machines. Swap out anaesthetic machines for ICU ventilators with appropriate humidifiers within the circuit – nullifying the need for HME filters.There needs to be further discussion with NHSI/Supply chain regarding equipment for patient ventilation at NHL.The risk associated with using anaesthetic machines as ventilators at NHL is escalated to the hospital risk register. Advertisement
‘The engineer apologised for the incident and said a letter would be issued to the family about the incident.
‘My family and I were absolutely devastated to learn this had happened while my brother was under the care of professionals. He was supposed to be having one-to-one care surely. I was equally saddened to hear that nine other patients had also been affected by this.
‘My brother was already in a bad state and I just felt this incident would only exacerbate the situation.
‘I was just in shock. I just thought what are the implications to this? That question just kept on going through my head. We asked the engineer to provide us with some form of report and explanation. We wanted to know how the filter error would affect my brother’s life.
‘I just kept on thinking of what my brother may have felt or how he may have suffered as a result of the incident.
‘I was up all night filled with worry and panic. I just didn’t understand how this had occurred and what would happen now.’
Just two days later, on April 21, Ms Lee and her family received a call from the Labs and Research department at the hospital seeking permission to enroll her brother into a drugs trial.
She said: ‘We were initially hesitant and did not feel he was fit enough to undergo any trials. He was on dialysis, he had suffered a cardiac arrest, he was on antibiotics, he was taking drugs for the heart. This is excluding what we learnt later, that he had undergone two intubations on the 17th and another on the 19th.’
However on April 23, Mr Patel’s health continued to deteriorate and his family received a call to say that doctors had determined he was now a DNAR patient, this in turn led the family to agree to the drug trials in an effort to save his life.
Ms Lee said: ‘They called to inform us that they had taken the decision to class my brother as a DNAR patient. They told us we had no say in the matter and that the doctors had confirmed that decision. It was heartbreaking. At this point we agreed to the drug trials. We were ready to do whatever we could to keep him alive.
‘It was a living nightmare. A waiting game where we had no idea what cards were going to be shown to us next.’
However on April 26, Mr Patel’s 22-year-old son Anish received a call telling him his father was dying and that he should go to the Nightingale as soon as he could to say his goodbye.
Ms Lee said: ‘I will never forget that day. I will never forget the sound of my nephew on the phone to me saying he needed to get to the hospital and hearing my brother’s wife crying.
‘Just hours later I received a call telling me my brother had passed away. I felt totally alone. I had lost my best friend, my warrior and my strength.
‘I wanted to cry out but I couldn’t. I didn’t know how I would tell my 83-year-old mother who I care for. How do you tell a mother her son is no longer alive?
‘I also thought about my brother’s six beautiful children. Their hurt and their pain.’
A month later, Barts Health Trust sent the family a Serious Incident Report that confirmed that ten ventilated patients had been identified as not having heat & moisture exchange (HME) filters within their ventilator circuits – with harm recorded for three of these patients.
The report said Mr Patel required re-intubation after his ET tube was found to be blocked.
It went on to suggest a number of reasons that could have led to the error, including a ‘lack of expertise within the clinical team working in the ICU’ and ‘potential confusion regarding what each patient needs’ due to the different types of ventilators in place.
The report said there were ‘multiple, potentially confusing disposable filters’ available for staff and it would not have been ‘immediately obvious on sight which filters are HME’.
It added the correct use of filters and their position within the circuit was ‘complicated’ and may not have been clear to all ICU employees before going on to state that suctioning was undertaken by staff with ‘limited expertise’.
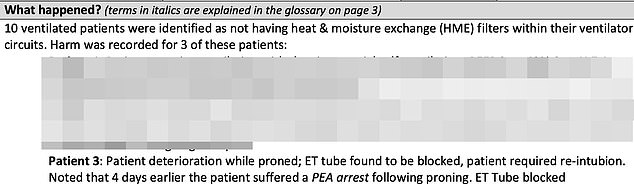
The Serious Incident Report said ten ventilated patients were identified as not having HME filters within their circuits. It went on to say the ET tube of Mr Patel (identified as patient 3) was found to be blocked and that he required re-intubation

The report sent from the health trust to Mr Patel’s family said there was a lack of expertise within the clinical team working in the ICU and the correct use of filer and their positions within the circuit was ‘complicated’ and may not have been clear to all staff
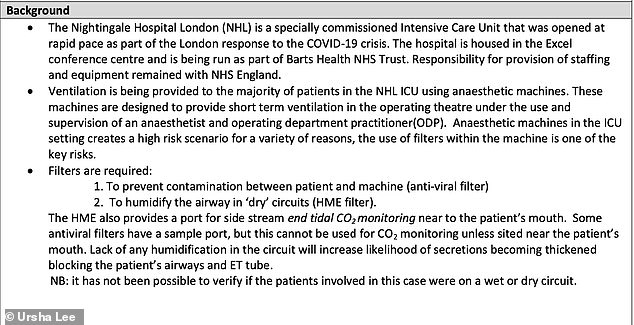
The report also said that ventilation was being provided to the majority of patients using anaesthetic machines – which are designed to provide short term ventilation in the operating theatre under the use and supervision of an anaesthetist
The report also said that ventilation was being provided to the majority of patients using anaesthetic machines, which are designed to provide short term ventilation in the operating theatre under the use and supervision of an anaesthetist and operating department practitioner (ODP).
What are Heat and Moisture Exchange (HME) filters? 
Heat and moisture exchangers (HME) can be placed at the patient’s end of the breathing system
In normal breathing, air is filtered, warmed and moistened by the nose and the upper airway.
However when endotracheal intubation – a procedure in which a tube is inserted through the mouth into the trachea – is performed on a patient this can result in an increased build up of mucus secretions.
This can increase the risk of infections and cause blockages in the breathing tube.
In order to combat this a heat and moisture exchangers (HME) can be placed at the patient’s end of the breathing system.
The filters humidify the airway in circuits.
Lack of any humidification in the circuit will increase likelihood of secretions becoming thickened – blocking the patient’s airways and ET tube.
Anti-viral filters will also be used to prevent contamination between patient and the ventilator machine.
Advertisement
When used in the ICU setting these machines can create a ‘high risk scenario’, with the use of filters within the machines being one of them, according to the report.
Despite questions from the family as to what ventilator Mr Patel had been on during his treatment at the hospital – a Penlon anaesthetic machine or a Draegar ICU ventilator- staff have not been unable to find this information.
The report also added: ‘It has not possible to verify if the patients involved in this case were on a wet or dry circuit.’
A ‘wet circuit’ is a breathing machine with active humidification while a ‘dry circuit’ requires a heat and moisture exchange (HME) filter to provide adequate humidification.
Ms Lee continued: ‘The report provided two sentences on my brother’s condition. It said the ET Tube had been blocked and mentioned and that four days earlier he had suffered a PEA arrest following proning.
‘There were no time references, especially regarding the event of the 18th, and one page was fully dedicated to a Glossary of Terms. I was devastated by the report. Both in terms of its content and its explanation of events.’
Mr Patel’s son Anish was also sent a letter of apology from Barts Health Trust which said the filter error had ‘reduced effectiveness of the circuit’ and ‘contributed to his father’s deterioration on 19th April’.
A section of the letter read: ‘We discovered that an issue had occurred with the filter in the breathing circuit that was providing ventilation to your father. The wrong filter had been placed in the circuit and as a result the circuit was not functioning as effectively as it could be.
‘We feel that the reduced effectiveness of the circuit and contributed to his deterioration on 19th April; it is very difficult to say if this event contributed to his sad death.’
Now, more than a year after her brother’s death, Ms Lee believes the temporary hospital, which was the first of the Nightingale hospitals to open, was not equipped to meet the demands of the pandemic.
She continued: ‘It was a fast train going at high speed, but it didn’t have a driver.
‘It wasn’t equipped with sufficient equipment and staff lacked expertise. It was a catastrophe.
‘I also don’t feel my brother should have been transferred there in the first place.
‘Months after his death we discovered that he had been attended to by a medical crash team soon after he was discharged from Northwick Park.
‘We didn’t know that until we received our first bundle of documents from the courts. We weren’t told.’
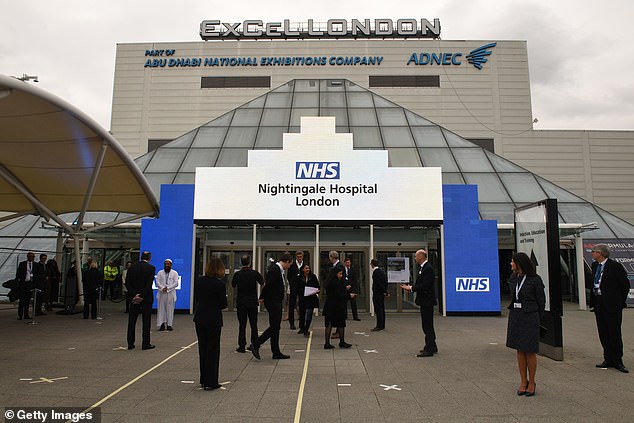
The Nightingale Hospital in London was one of seven temporary hospitals opened on April 3 last year

Prior to its opening, images from inside the hospital showed military personnel erecting cubicles and carrying equipment

The field hospital, which shut its doors on May 15, was set to hold up to 4,000 Covid-19 patients

Barts Health trust said the incident would have ‘reduced effectiveness’ of the ventilator and ‘contributed to Mr Patel’s deterioration on April 19’

Following her brother’s death, Ms Lee has also been in contact with Northwick Park to try and locate her brother’s phone – which remains the only possession he had on him when he was taken to the hospital.
She added: ‘We contacted Northwick Park Hospital in order to obtain his phone as we had been told by a nurse prior to his transfer that his possessions would be placed in a secure location. But we were absolutely stunned to hear they did not have his mobile phone.
‘His phone contained an array of family photographs and memories and our last moments with him were on that phone call to him. I don’t understand how it just went missing.’
Mr Patel’s family are now preparing for a coroner’s inquest into his death which is due to take place on October 4.
Ms Lee added: ‘It has been incredibly stressful but I keep on going for my brother.
‘There are so many key elements that made my brother who he was. The foremost was his humility, his mental strength and his devotion to his six children whom he loved unconditionally.
‘He was well known within the neighbourhood and even after completing a full nightshift on the N18 bus he would avidly run around his local park around 10 times before going home to sleep.
‘He lived his life as a simple and gentle man and was a prime example of a humble soul.’
Last month it emerged that a second patient, Kofi Aning, 66, from Enfield, north London, who worked as a carer, was also among the patients to have been affected by a wrong filter in his breathing system.
A TIMELINE OF THE NIGHTINGALE HOSPITALS
NHS Nightingale Hospital London
Announced: March 24, 2020Opened: April 3 (by Prince Charles)Closed: May 15, 2020What now? Open for vaccinations
NHS Nightingale Hospital Birmingham
Announced: March 27, 2020Opened: April 16 (by Prince William)Down to standby: May 5, 2020What now? Closed for good on April 1, 2021
NHS Nightingale Hospital North West
Announced: March 27, 2020Opened: April 17 (by Duchess of Cornwall)Down to standby: June 5, 2020What now? Closing for good
NHS Nightingale Hospital Yorkshire and the Humber
Announced: April 3, 2020Opened: April 21 (by Captain Tom Moore)Radiology outpatient clinic: June 4, 2020What now? Closing for good
NHS Nightingale Hospital North East
Announced: April 10, 2020Opened: May 5 (by Matt Hancock)What now? Open for vaccines
NHS Nightingale Hospital Bristol
Announced: April 3, 2020Opened: April 27 (by Matt Hancock & Prince Edward)Down to standby: July 6, 2020What next? Closing for good on March 31, 2021
NHS Nightingale Hospital Exeter
Announced: April 10, 2020Opened in standby: July 8, 2020First Covid patients: November 26What next? Hospital announced the focus on Covid-19 care would be cut from 1 April and it will be open for local NHS Advertisement
He sadly passed away on April 23.
A Barts Health spokesperson said: ‘We offer our deepest sympathies to Mr Patel’s family.
‘We have fully investigated the circumstances, changed our practice accordingly and do not believe that the incident with the filter was a direct cause of Mr Patel’s death.
‘This will be further considered by the coroner at the inquest.’
The Nightingale Hospital in London, which was opened by Prince Charles on April 3, was one of seven temporary hospitals opened to great fanfare at the start of the pandemic last year, along with centres in Birmingham, Manchester, Exeter, Harrogate in North Yorkshire, Bristol and Washington in Tyne and Wear.
Prior to its opening, images from inside the field hospital showed military personnel erecting cubicles and carrying equipment into the transformed centre- which was set to hold up to 4,000 Covid-19 patients.
The centre was hastily put up in less than two weeks in March, amid fears the capital’s hospitals could be overwhelmed by spiralling Covid-19 admissions.
However by May 6, 2020, the Government dashboard showed only five patients remained at the facility and just six weeks later the hospital was moved to ‘standby’ and closed its doors on May 15.
Figures later showed the temporary hospital only treated a total of 54 patients.
Efforts were then launched to re-construct a ‘scaled-down’ version of the mothballed hospital and the facility was reopened in January this year to admit non-Covid patients in order to ease the pressure in the critical care wards across the capital.
In March, medical staff at the Nightingale Hospital defended the creation of facility but admitted the complexity of coronavirus led to issues.
In a paper in the medical journal Intensive Care Medicine, the doctors disclosed 54 patients were treated for Covid between April 7 and May 7 and all those admitted were invasively ventilated at the time of admission.
In their paper the staff said that it ‘remains moot’ whether the facility was the best way of treating patients.
They wrote: ‘Whether the NHL blueprint was the optimal model of care or represented appropriate resource allocation remains moot but it was deemed necessary at a time of crisis.’
The doctors went on to say: ‘The operating model as originally conceived was based on previous (influenza) pandemics. Subsequent clinical experience highlights that the clinical syndrome of Covid-19 and the spectrum and duration of multi-organ support requires comprehensive critical care capacity. Future planning should account for this.’
Earlier this year NHS England announced four out of the seven Nightingale Hospitals across the country would close permanently.
The facilities in Birmingham, Manchester, Bristol and Harrogate shut their doors permanently in April while the three remaining Nightingales, in Exeter, London and Sunderland, will be kept either as extra NHS capacity for routine work or as Covid vaccine centres.
Source link : https://www.dailymail.co.uk/news/article-9843189/London-bus-driver-three-Covid-patients-die-capitals-NHS-Nightingale-staff-error.html











