Diagnoses of chronic illnesses in England fell by up to half last year in a trend that was partly fuelled by fewer GP appointments during the pandemic, stark official figures revealed today.
Incidence of chronic pulmonary disease (COPD) — a group of lung diseases that can cause breathing difficulties — was down 51 per cent in 2020 compared to 2019.
The number of patients diagnosed with atrial fibrillation, an irregular heart rate which raises the risk of strokes and heart attacks, fell by 26 per cent, followed by heart failure and diabetes, which both dropped by a fifth. Coronary heart disease cases were also down 17 per cent, the report found, and strokes fell by 16 per cent.
The Department of Health and Office for National Statistics report suggests tens of thousands fewer people got a delayed diagnosis, risking their condition worsening. It claimed ‘reduced general practice activity’ was likely partly behind the trend.
The figures came as the chair of the doctors’ union the British Medical Association (BMA) said patients were wrong to think they received ‘worse care’ as a result of a lack of in-person consultations during the pandemic.
Dr Richard Vautrey, head of the BMA’s General Practitioners committee, claimed GP surgeries needed more money to get face-to-face GP appointments back to pre-pandemic levels.
The timing of his comments were slammed as being ‘tone deaf’ by the Adam Smith Institute thinktank, which said: ‘It shows the BMA does not want to see the problem and doesn’t want to see the real solution.’
NHS figures suggest around 23million fewer face-to-face GP consultations were carried out in the first wave of the Covid pandemic alone, as NHS services and practices were encouraged to move to virtual settings and Brits were more reluctant to come forward due to virus fears.
As well as missed diagnoses, the shut down of NHS services during the pandemic allowed waiting lists to spiral to record highs, with 5.6million people now waiting for routine operations.
Boris Johnson’s has pledged a manifesto-busting £30billion to the NHS over the next two years to help clear the mammoth backlog. But Dr Vautrey said ministers weren’t ‘investing in general practice as seriously as they need to’.
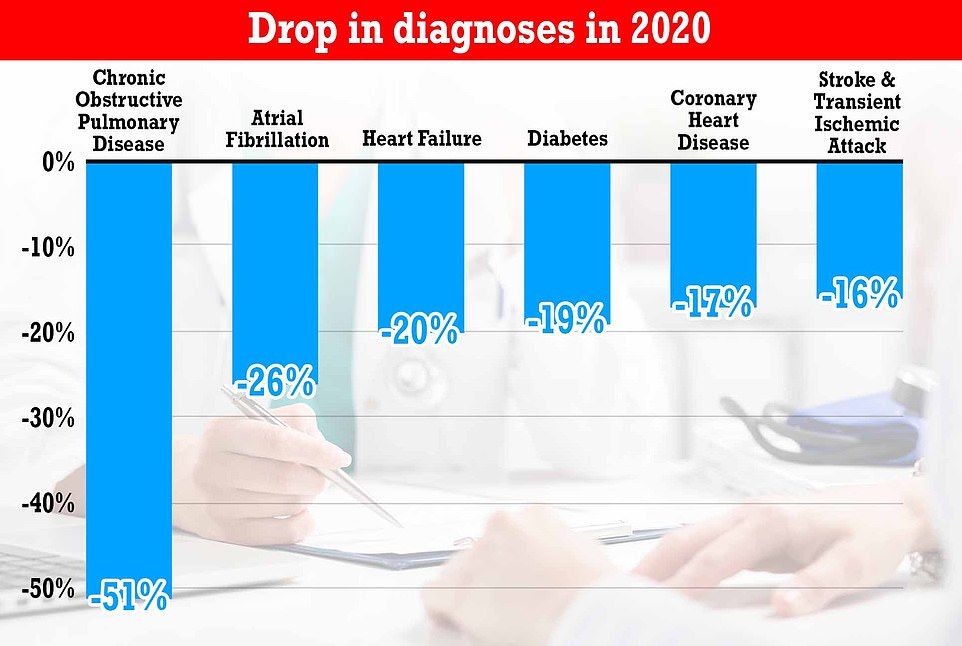
Diagnoses of chronic illnesses fell by up to half last year fuelled by a lack of GP appointments during the pandemic. Incidence of chronic pulmonary disease (COPD) — a group of lung conditions that cause breathing difficulties — was down 51 per cent in 2020 compared to 2019, a damning Department of Health report found. The number of patients diagnosed with atrial fibrillation, an irregular heart rate which raises the risk of strokes and heart attacks, was down by 26 per cent, followed by heart failure and diabetes, which both dropped by a fifth. Coronary heart disease cases were also down 17 per cent, the report found, and strokes fell by 16 per cent
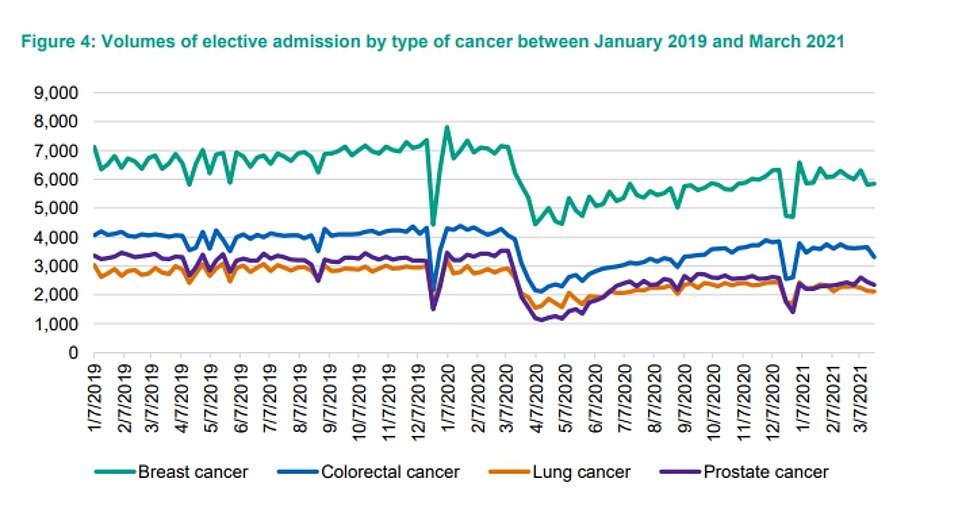
The report also found that thousands fewer people were admitted for cancers during 2020, which it warned ‘these treatment delays are likely to lead to poorer health outcomes for patients’
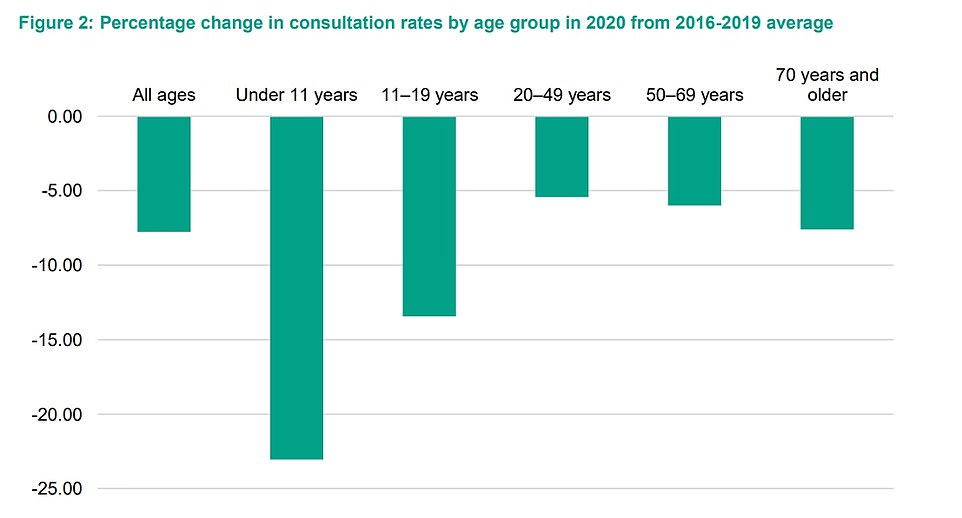
It found that GP appointments for children under the age of 11 had the most sustained fall (23 per cent below four-year average). The 11 to 19 age group also seen sharp falls (13.4 per cent), which were most pronounced when lockdown restrictions were in place. Amongst older people, the impact was less significant, with a 7.6 per cent drop in consultations in 2020 relative to the four-year average. But this still translates to millions of missed consults
Today’s report on missed diagnoses was submitted to Government on September 9 but made public today as part of a batch of scientific and public health reports used to guide ministers through the pandemic.
It found that GP appointments for children under the age of 11 had the most sustained fall (23 per cent below four-year average). The 11-19 age group also saw sharp falls (13.4 per cent), which were most pronounced when Covid lockdown restrictions were in place.
Amongst older people, the impact was less significant, with a 7.6 per cent drop in consultations in 2020 relative to the four-year average. But this still translates to millions of missed appointments.
The report also found that thousands fewer people were admitted for cancers during 2020, which it warned ‘these treatment delays are likely to lead to poorer health outcomes for patients’.
Meanwhile, MailOnline’s analysis of NHS data yesterday found, as well as elective treatment and GP appointments, more than a million emergency hospital admissions were ‘lost’ to the coronavirus pandemic.
There were approximately 5.45million emergency procedures carried out across all NHS England services in the 12 months to March, down 16 per cent on the 6.5m the previous year.
The NHS Digital figures included admissions for A&E, mental health, maternity and even dental patients, showing how the pandemic impacted every corner of the health service.
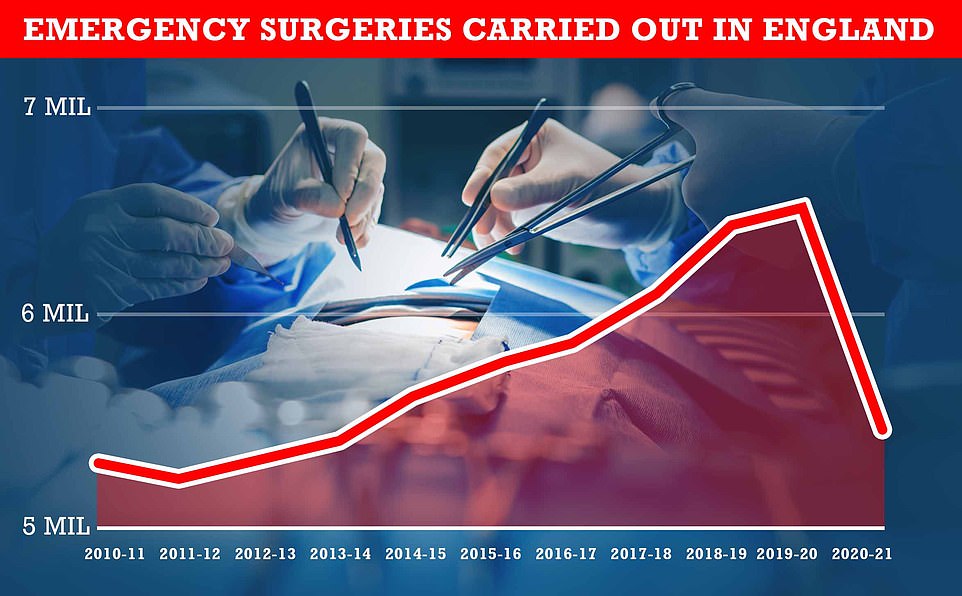
There were 5.45million emergency procedures carried out across all NHS England services in the 12 months to March, down 16 per cent on the 6.5m the previous year
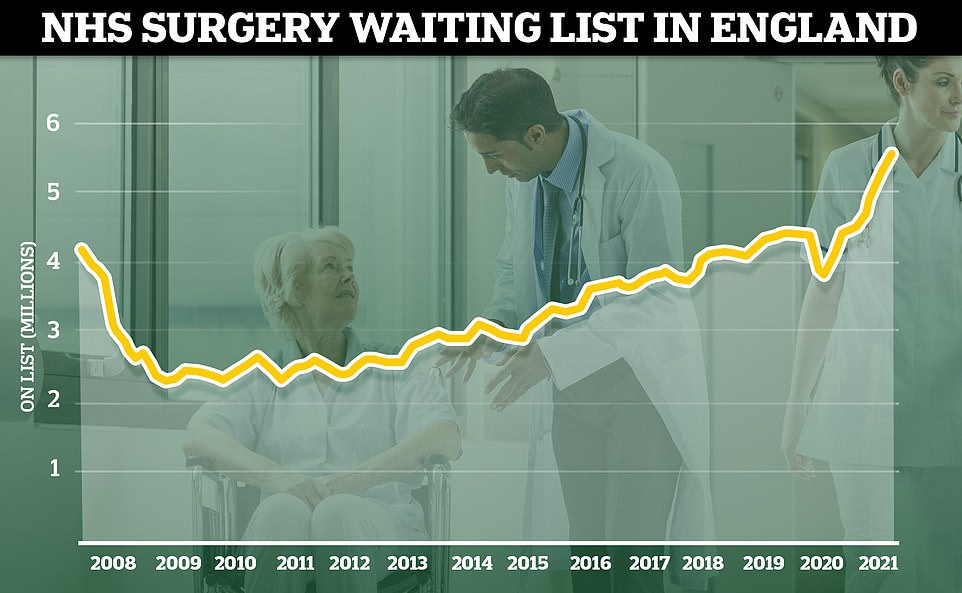
The number of patients waiting for routine hospital treatment hit 5.6million in July, the highest figure since records began in 2007. And health chiefs have warned the backlog is going to get much worse before it gets better, with projections that it could soar up to 13million by the end of the year if no action is taken
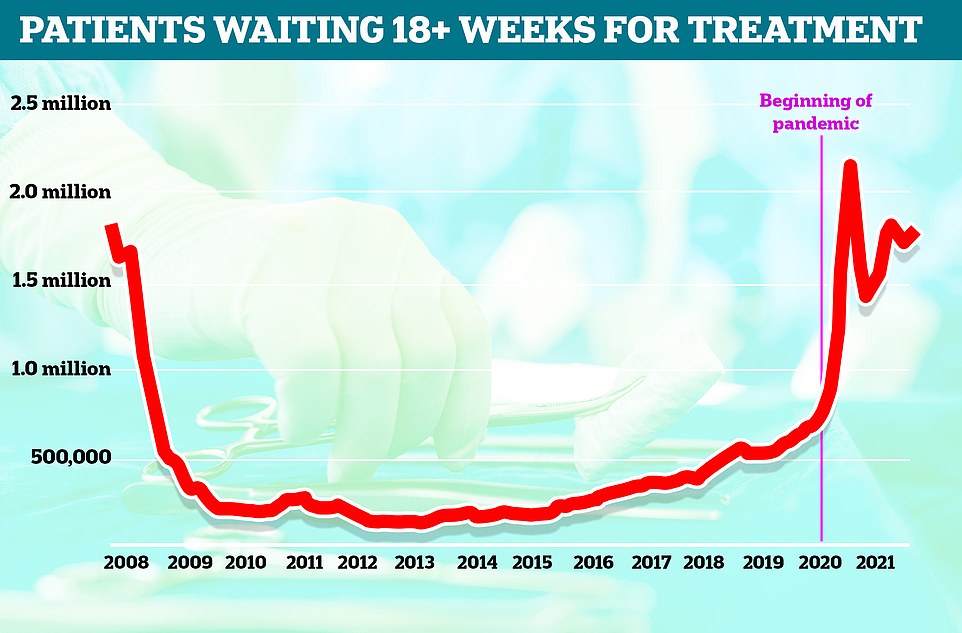
Patients forced to wait more than 18 weeks for routine surgery – the maximum time someone should wait under the NHS’s own rules – reached 1.7million in July, the highest level in four months
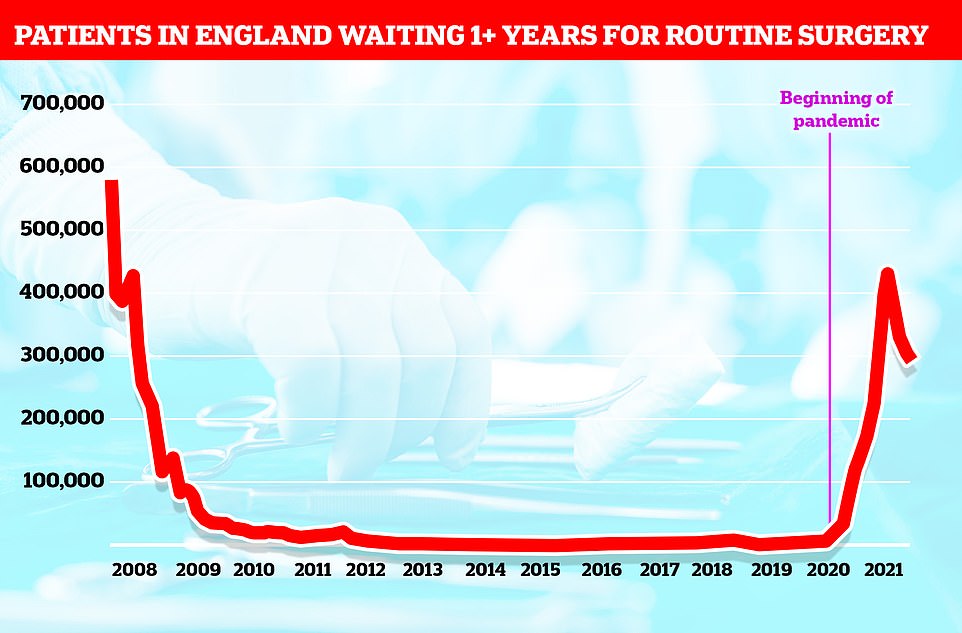
Some 293,000 people had been waiting more than a year for treatment on the NHS by July this year, figures showed. This was down slightly on last month when there were 304,803 people on the list, but still almost three times the same levels last year. The list has surged after the pandemic forced hospitals to turn over whole wards to fighting the virus
‘Eye-watering’ one in 10 people in England are now waiting for routine operations on the NHS
One in ten people in England are stuck on the NHS waiting list for routine operations, extraordinary figures revealed today as queues hit another record high.
Latest NHS data showed that 5.6million people across the country were waiting for elective surgery in July — the most since records began in 2007 — after the number rose continuously during the pandemic.
Waiting lists spiralled after Covid forced hospitals to cancel routine operations and turn over whole wards to patients suffering from the disease. Social distancing and extra Covid precautions have made it even harder to start chipping away at the record waiting lists.
Record numbers of patients are now turning to private health rather than waiting for help from the NHS, figures show, with one private provider seeing patient numbers rise by 80 per cent on the back of the pandemic.
The waiting list includes people waiting for operations like knee, hip and joint replacements, as well as cataracts surgery.
The number who’ve waited more than a year to start treatment stood at 293,000 last month, almost three times as high as the same time last year when 83,000 had been on the list for this long.
And more than 1.7million people have been waiting more than 18 weeks for surgery, outside the period in which the NHS aims to see every patient.
The Royal College of Surgeons said today that behind these ‘eye-watering’ statistics were patients ‘waiting in pain’ that was leaving them unable to work or carry on with their daily lives. Top medics said the NHS was already ‘running on empty’ as it heads into winter which is its busiest period.
Advertisement
Figures also show there were 3.2million fewer elective surgeries in the same period, with 5.6million coming in for care during the pandemic compared to 8.8million pre-Covid.
Addressing the row over the lack of face-to-face GP appointments which has erupted over the past few weeks, Dr Vautrey told BBC Radio 4’s Today programme that the BMA recognises there aren’t enough GPs and nurses.
To rectify this, he said the Government must do what it ‘promised to do which is to recruit 6,000 more GPs, to invest in our premises, to invest in our staff and our service and by doing that we will get a better service for our patients’.
He said ‘we need the number of GPs to increase’ to get back to pre-Covid levels of in-person appointments, and ‘we need the space within our surgeries to increase to be able to do that safely’.
Matt Kilcoyne from the Adam Smith Institute told MailOnline: ‘The BMA’s response is typical of the BMA, it just wants more cash for its members, which never fixes the actual issues.
‘The problem is the BMA is acting in the interest of its members and it is is putting patients’ lives at risk.’
It comes after a senior coroner last week ruled a lack of face-to-face GP consultations contributed to the deaths of five people.
A third fewer people are seeing their GP in-person now compared to before the pandemic and tens of millions of appointments were ‘lost’ during the Covid crisis.
GPs were urged to conduct all consultations remotely and strongly encouraged not to invite patients for an in-person appointment unless they deemed it an emergency.
But trusts have continued to incentivise the practice more than a year after the original lockdown, with doctors being offered bonuses to keep attendances low.
Health Secretary Sajid Javid fired a warning shot at GPs in the Commons earlier this week, telling them: ‘GPs should be offering face-to-face access.’
Meanwhile, a total 5.6million people across the country were waiting for elective surgery in July — the most since records began in 2007 — a number which has risen continuously during the pandemic.
Waiting lists spiralled after Covid forced hospitals to cancel routine operations and turn over whole wards to patients suffering from the disease.
Social distancing and extra Covid precautions have made it even harder to start chipping away at the record waiting lists.
Record numbers of patients are now turning to private health rather than waiting for help from the NHS, figures show, with one private provider seeing patient numbers rise by 80 per cent on the back of the pandemic.
The waiting list includes people waiting for operations like knee, hip and joint replacements, as well as cataracts surgery.
The number who’ve waited more than a year to start treatment stood at 293,000 last month, almost three times as high as the same time last year when 83,000 had been on the list for this long.
And more than 1.7million people have been waiting more than 18 weeks for surgery, outside the period in which the NHS aims to see every patient.
Woman, 27, died from liver cancer after GPs failed to spot tumour for five MONTHS during virtual appointments and refused to see her in-person because of Covid fears 
Jessica Brady, 27, died from stage-four cancer in December after struggling to get an in-person appointment with her GP during the pandemic
The mother of a young woman who died from cancer has told MPs her daughter might still be alive if she was seen by her GP face-to-face.
Jessica Brady, 27, from Stevenage in Hertfordshire, passed away from liver cancer in December after a series of virtual appointments over the course of five months failed to spot her tumour.
Her mother, Andrea, told the Health and Social Care Committee today that Jessica was repeatedly denied an in-person appointment after first complaining of abdominal pain last summer, despite the epidemic being largely under control at that point.
She was diagnosed with a kidney infection ‘in the absence of any diagnostic testing or any physical examination at all’ and prescribed with antibiotics.
When she became extremely fatigued and her symptoms worsened, she was only prescribed more antibiotics, steroids, and an inhaler.
One set of blood tests even revealed Jessica had high D-dimer levels, which can be a signal of solid cancers, the mother told MPs.
And subsequent tests identified concerns regarding her liver function – which her mother said makes sense now as she had liver cancer – but medics decided to wait six weeks to see what happened.
Doctors didn’t put ‘the pieces of the jigsaw together’ that it was cancer until five months later, by which point the cancer had spread around Jessica’s body and become untreatable.
It comes as Health Secretary Sajid Javid demanded ‘more GPs should be offering face-to-face access’ and ‘we intend to do a lot more about it’.
Figures show a third fewer people in England are seeing a GP now than before the pandemic and tens of millions of appointments were ‘lost’ during Covid.

Andrea Brady, Jessica’s mother, told MPs her daughter needed a face-to-face appointment ‘really early on’. She was told to get a gastroscopy after in-person appointments, but if this happened a few months earlier, her cancer ‘wouldn’t have spread so aggressively’, Mrs Brady said
Ms Brady revealed that Jessica was only finally seen in person by a GP when she bombarded her local surgery with more than 20 phone calls.
The family doctor told the family that Jessica ‘probably needs a gastroscopy’, her mother told the committee.
If this procedure – which involves a camera taking pictures inside the stomach – happened a few months earlier, her cancer ‘wouldn’t have spread so aggressively’, Ms Brady said.
‘Jess was a very gentle, sweet person, but she really did attribute her late diagnosis to the slow reaction of her GP surgery,’ her mother added.
Even after seeing a GP in-person, it was not until she sought private health care that she was diagnosed with stage four cancer of the lungs, bones, spine and liver.
She went to hospital on the day of her diagnosis and died three and a half weeks later on December 20.
Asked about Jessica’s challenge in getting a GP appointment, she said: ‘It was incredibly challenging for Jess, just navigating the whole system of consult procedures.
‘I think the most important thing is we feel, and Jess felt that no one listened, no one took it seriously and more than anything, she needed a permitted face-to-face appointment really early on, with people making notes.
‘And also, during all that time, she wasn’t seen by one designated doctor, four different doctors spoke to Jess and prescribed her medication. And we think that was really key.
‘No one person was looking at the whole picture and putting the pieces of the jigsaw together. That didn’t happen until two days before Jess received her diagnosis, when I think there was an element of panic, because she was receiving quite a lot of phone calls at that stage, and saying you probably need a gastroscopy.
‘In fairness, if that had happened three months earlier, obviously her cancer would not have spread – well we think it wouldn’t have spread so aggressively by then – so I think it’s fair to say that Jess was a very gentle, sweet person, but she really did attribute her late diagnosis to the slow reaction of her GP surgery.’
Her parents have launched a petition calling for a cancer specialist in every doctor surgery, a dedicated GP for each patient, frequent courses for GPs and a public health campaign on the warning signs of cancer in young people.
In response to Jessica’s case, Dr Richard Roope, clinical adviser for cancer at the Royal College of General Practitioners, told MPs: ‘In general practice we talk about learning events and this is the mother of all learning events.
‘To state obvious, no GP gets up in morning to miss a diagnosis.
‘We are there to help our patients and to enable access to the best treatment and diagnostics in a timely fashion and I think we can do things better than what has happened.
‘And I think the narrative that we’ve heard is in a way a manifestation of essentially demand outstripping supply.
‘That all GPs could do more if we had more time and if there was more GPs we could give more time to each patient.’
It comes as the Health Secretary said today that ‘everyone can understand’ why GPs ‘couldn’t provide access in the normal way’ during the peak of the coronavirus pandemic.
But he said ‘we are way past that now’ and doctors should be following society in going back to ‘completely normal’ life.
He said that ‘more GPs should be offering face-to-face access’ and ‘we intend to do a lot more about it’.
Virtual appointments were heavily encouraged throughout the Covid crisis in an attempt to keep social mixing low and hospitals virus-free.
But trusts have continued to incentivise the practice, with GPs being offered bonuses to keep in person attendances low.
There are fears that some people, particularly the elderly, are being left behind.
Recent data from NHS Digital showed 57.2 per cent of appointments in July were conducted face-to-face.
That is higher than the low of 46.8 per cent last April, as the first Covid wave swept across the UK, but much lower than the 80 per cent pre-pandemic figure.
Source link : https://www.dailymail.co.uk/news/article-10002077/Lung-heart-disease-diagnoses-fell-HALF-pandemic.html











