COVID-19 patients who require intensive care are likely to have delirium and other neurological symptoms, a new study finds.
Researchers at the University of Michigan identified delirium in 73 percent of patients admitted to the Michigan Medicine intensive care unit (ICU) between March 2020 and May 2020.
The patients had the condition for at least four days with some experiencing the symptom for as long as 17 days.
Some of the patients also reported delirium, dementia, depression, and other cognitive issues in the months after they returned home from the hospital.
The findings adds additional evidence to past studies and experiences from long Covid patients, who say that neurological issues are a common – yet under-studied – facet of the disease.

Covid patients hospitalized in an ICU are very likely to have delirium and other neurological symptoms, a recent study shows. Pictured: Nurses care for a Covid patient at an ICU at Sharp Grossmont Hospital in La Mesa, California, May 2020
Covid is commonly seen as a respiratory disease, but in the past year and a half, researchers have catalogued its potential to impact many other parts of the body.
The disease can cause long-term loss of smell and taste, cardiovascular issues, gastrointestinal complications, neurological symptoms, autoimmune issues and more.
Neurological symptoms may be one of the most concerning categories.
Covid has been documented as a cause of prolonged fatigue, ‘brain fog’ and other related challenges for long Covid patients, who suffer from symptoms for weeks or months after their initial infection.
And in patients hospitalized with severe Covid cases, clinicians have found that delirium may be a common symptom.
Delirium is a confused mental state, in which patients have a limited ability to navigate their environment.
A recent study further demonstrates that delirium is common in patients who require intensive care in the hospital.
Clinicians at Michigan Medicine, a hospital in the University of Michigan system, followed Covid patients who were admitted to the intensive care unit (ICU) with dementia early in the pandemic.
Their study was published on September 17 in the journal BMJ Open.
In total, Michigan Medicine saw 148 Covid patients in its ICU between March 1 and May 31, 2020.
Of those 148 patients, 108 experienced delirium during their ICU stay.
That’s 73 percent – almost three-quarters – of all ICU patients.
These patients experienced delirium for at least four days – some as long as 17 days – and the median symptom duration was 10 days.
Half of the patients who experienced delirium were black, following a trend – the majority of ICU patients at the hospital were black.
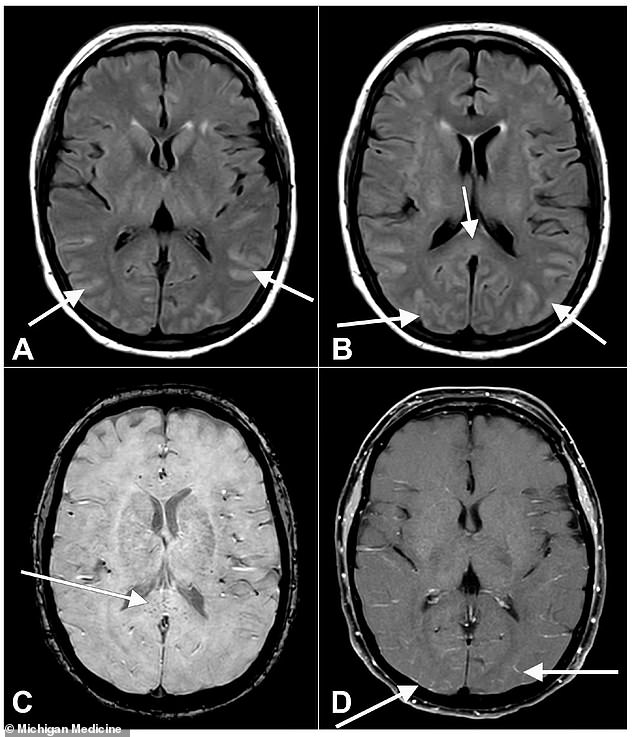
Scientists are still working to understand how Covid causes delirium, but it may be linked to inflammation in the brain – shown in patient D’s brain scan here
The researchers noted, however, that this number of black patients was ‘disproportionately high’ compared with overall demographics at the hospital.
‘COVID is also associated with a number of other adverse outcomes that tend to prolong hospitalization and make recovery difficult,’ said study author Dr Phillip Vliside in a statement.
The delirium patients also tended to have other comorbidities such as hypertension and diabetes.
In a further signal that delirium was associated with more severe Covid disease, the delirium patients had longer hospital stays – and longer stays in the ICU – than those patients who didn’t experience this symptom.
Upon leaving the hospital, about one-third of the delirium patients had not recovered from this symptom.
Many patients – 40 percent – needed assistance from a skilled nurse after leaving the hospital.
Along with recording the patients’ experiences with delirium in the hospital, the researchers also surveyed them after they returned home from the hospital.
The researchers were able to survey about 20 patients and their families, two to three months after they returned home.
About a quarter of those patients still had delirium symptoms, two to three months later.
Some of the delirium patients also reported dementia, depression, and other cognitive issues that were not resolved, months after they returned home from the hospital.
‘A family member who is confused has limited ability to care for themselves and will require additional caretaking support, which is certainly a big challenge,’ Vlisides said.
Scientists have not yet determined how a coronavirus infection may lead to delirium, but the Michigan Medicine researchers say that multiple factors may play a role.
The coronavirus might infect nervous system cells, and might also lead to an inflammatory response that causes the immune system to attack itself.
The researchers performed brain scans for some patients – and noted that a couple of the delirium patients had abnormal fluid or signs of inflammation in their brains.
The Michigan Medicine findings aligned with other research on delirium in Covid patients, showing that between 65 and 80 percent of ICU patients may have this symptom.
However, Vlisides noted that the study’s timeframe – during the pandemic’s first wave – may have made it possible that some patients experienced delirium due to the conditions of their hospital stays, rather than thanks to the virus itself.
‘Early on in the pandemic, we weren’t performing standard delirium prevention protocols like we usually do,’ he said.
Patients with delirium were also more likely to have sedatives prescribed to them.
Still, Vlisides said that this study presents a warning about Covid’s long-term impacts.
‘Overall, this study highlights another reason why getting vaccinated and preventing severe illness is so important,’ he said.
‘There can be long term neurological complications that perhaps we don’t talk about as much as we should.’
Source link : https://www.dailymail.co.uk/health/article-10022417/Nearly-three-quarters-COVID-19-patients-admitted-Michigan-hospitals-ICU-delirium.html











