A senior doctor at London’s NHS Nightingale Hospital has told an inquest into the death of a Covid patient he had ‘no control’ over equipment or staff and the hospital did not have ‘the systems of care we thought we needed’.
London bus driver Kishorkumar Patel, 58, was one of the first patients to be transferred to the flagship Nightingale, which was opened last year by then health secretary Matt Hancock, for coronavirus treatment on April 7.
Despite being described as ‘physiologically stable’ before he was transferred, the father-of-six, who had no underlying health conditions, died 19 days later on April 26.
He was one of three patients to die at the ExCel Centre in Newham, East London, after staff left his intensive care ventilator without heat and moisture exchange (HME) filters, according to a Serious Incident Report (SIR).
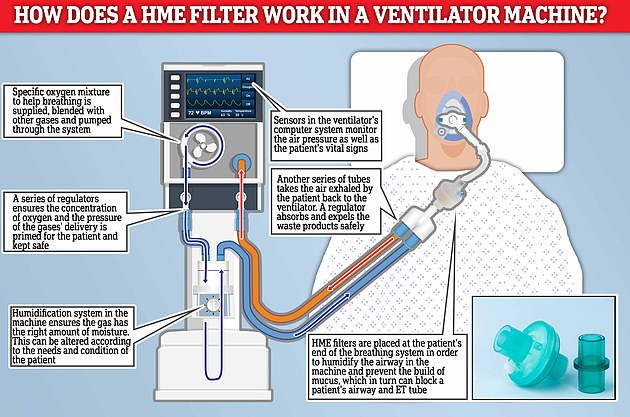
HME filters are placed at the patient’s end of the breathing system in order to humidify the airway in the machine and prevent the build of mucus, which in turn can block a patient’s airways and endotracheal (ET) tube.
But the staff error, which saw them use the wrong filter in the ventilation circuits, led to the breathing tubes in three patients becoming blocked and saw all of them ‘suffer harm’ and require re-intubation.
During today’s inquest Dr Alastair Proudfoot, the clinical lead at London’s Nightingale, told coroner Nadia Persaud the hospital did not have ‘the systems of care we thought we needed’ amid the first wave of the pandemic.

Kishorkumar Patel, 58, was one of three patients to die at the London’s Nightingale Hospital in April last year

The Nightingale Hospital in London was one of seven temporary hospitals opened by then health secretary Matt Hancock at the start of the pandemic last year
Dr Proudfoot said: ‘We didn’t have the systems of care we thought we needed. Two of the very key items that we had no control over were equipment and staffing.
‘Ventilators and ICU nursing staff were two of the most prized commodities across the NHS.
‘Unusually we were not given any ownership or understanding of what equipment we were receiving and why.
‘In terms of the staff, again the people that came either volunteered or were released by their parent trust.
‘That was controlled by NHS London – we did not put out an advert. We invited people to come and but we had no control over who we employed.
‘It was not a homogenous group of people who had worked together before or had even met each other before.’
The hospital used two types of machines for ventilating patients, Penlon anaesthetic machines and the more complex and effective Draeger ICU ventilators, the inquest heard.
But due to a shortage of the ICU grade ventilators, Mr Patel was placed on an anaesthetic machine, which are only designed for short-term use, until April 13.
Dr Proudfoot continued: ‘The anaesthetic unit is not as capable as an ICU ventilator. If I was going to be crude, it is effectively a bag of gas that goes up and down.
‘We were moving patients from an anaesthetic machine to a ventilator when they became available.
‘In an ideal world, we would have been provided with 4,000 ventilators, I didn’t have that, we were provided with anaesthetic machines.
‘All we knew about Covid-19 at the beginning was it was primarily a disease of the lungs and through an inflammatory process it progressed to multiple organ failure.’
Seven days before his death, Mr Patel’s family were told a doctor at the hospital had discovered that his endotracheal (ET) tube in his windpipe, which provides oxygen to a patient, was blocked as a result of an ‘incorrect filter’ in his ventilator.
A Serious Incident Report sent to the family later described how medical staff discovered heat and moisture exchange filters had not been used in his intensive care ventilator – resulting in a lack of any humidification in the machine.
The incident would have ‘reduced effectiveness’ of the ventilator and ‘contributed to Mr Patel’s deterioration on April 19’, a letter to the family from Barts Health NHS Trust also added.
Dr Nikul Patel, who discovered the error inside the bus driver’s ventilation system, told the inquest how he found the ventilators had incorrectly been fitted with bacterial and viral filters, rather than humidity and moisture exchange (HME) filters.
He said had the correct filters been used ‘the secretions would not have built up in such a short space of time.’
Dr Patel said: ‘It was noted the filter at the patient end was a different make and model to what was usually used. The patient should have had a heat and moisture exchanger, or HME, and these come in a variety of shapes and colours.
‘I noted the filter used was a bacterial and viral filter that was also hydrophobic.
‘This raised my suspicion as normally HME filters would absorb water and therefore allow the humidification of the airways.
‘A junior doctor searched the make and model of the filter on the internet and we found the filters that had been used had not been HMEs but as the packaging suggested solely bacterial filters.
‘We then changed the filter on this patient and all the others on the ward for HMEs.’
The doctor noted that the incorrect filters had resulted in ‘excessively thick secretions’ that led to a blockage in Mr Patel’s airways.
When asked if he had spoken to staff about the incident, he said: ‘I think we did talk about it. I asked if anyone had noticed it.
‘It was unclear, people had unclear thoughts and views about whether that filter was in use a week ago or whether it’s just been used.
‘I don’t think anyone was sure whether that filter had been an ongoing issue or whether it had been an issue in the past 24 hours.’


The London bus driver was described as ‘physiologically stable’ when he was transferred to the Nightingale for coronavirus treatment on April 7

Mr Patel, who held a first-degree black belt in Kung Fu, was on an anaesthetic machine until April 13 due to a shortage of purpose-built intensive care ventilators at the field hospital
Mr Patel’s son Anish, who attended the inquest remotely, said the family were given ‘false hope’ the day before his father’s death.
He said: ‘The day before my dad died, we were told that he had started coughing. We did not really understand the situation. It gave my family a sense of false hope.
‘We weren’t told what was meant by this, so is there a log of it anywhere?’
Dr Proudfoot said: ‘I’m desperately sorry but I’m not aware of the specifics. I’m deeply sorry.
‘What I would reassure you is that compassionate care was at the forefront of what we did and I’d like to think that wasn’t a sign of distress. The significance of that, clinically, I don’t know.’
Dr Andrew Wragg, who was an acting deputy director at Nightingale, was asked why staff did not give written statements at the time to determine how and why the wrong filters were used.
He said: ‘There was a huge resource challenge at the time because of the challenges that were asked of us.
‘We put in a reporting system at the time, but when we got to serious incidents the standard approach was not fit for purpose.
‘We got permission from NHS trusts to get permission to use an abridged version that would focus on finding
‘While I’m sure it’s likely you’ll [the Coroner] consider this to be human factors, that people can make mistakes, but this was also related to ongoing pandemic awareness in the NHS, how to cope with increased patient needs, increased capacity, and the timing of lockdowns.
‘The approach was rather than to not peel back on every error, we focused on what we could do to make it safe at that moment
‘This incident was a very good example of something we hadn’t considered before but gave us a fresh look.’
He continued: ‘Different trusts often use different filters.
‘There was a lot of confusion, which one hand is an issue in the manufacturing, but also about the procurement. If the procurement is running centrally, you’ll be given equipment that you are not familiar with.’
Mr Patel was initially admitted to Northwick Park Hospital in north west London, on April 4, 2020, after experiencing shortness of breath, loss of smell, coughing and fatigue.
During the inquest yesterday, Dr Tariq Husain, a consultant in anaesthesiology at Northwick Park Hospital, told coroner Nadia Persaud that Mr Patel was transferred to the Nightingale Hospital due to the onslaught of Covid patients in April 2020.
He said: ‘We had significant challenges. Under normal circumstances we have two intensive care consultants working seven days but at the height of the pandemic we had five or six consultants in intensive care.
‘We also drafted in junior doctors from other hospitals and specialties – even if they had not ever worked in intensive care.
‘We had a cohort of intensive care nurses and we had additional support from the theatre staff.
‘Normally, the nursing ratio in normal circumstance is one for every patient – at its worst we had one intensive care nurse looking after six patients.’
Dr Husain said: ‘There was a group of patients who were physiologically safe. There were also a large group of patients that were unable to be transferred because they were too unsafe and there was a substantial risk they would deteriorate en route.’
Mr Patel’s sister, Ursha Lee, who attended the hearing remotely, said the family were unaware of a consent procedure for transfer and explained they only agreed for their loved one to be moved because they were told Northwick Park had no beds.

Mr Patel’s sister, Ursha Lee, said they only agreed for their loved one to be moved because they were told Northwick Park had no beds

The father was among the first patients to have been transferred to the Nightingale for coronavirus treatment in April last year. Pictured: Mr Patel with his children Sarita, Kiran, Zoe, Aakash, Shane and Anish

Mr Patel’s son Anish said the family were given ‘false hope’ the day before his father’s death
The doctor told the court: ‘We had to create capacity. If we didn’t, people would have been dying in corridors.
‘It wasn’t intentional for us to not pay mind to what families wanted, as I know some families didn’t want their relatives transferred out.’
Key findings and critical actions required from the Serious Incident Report
Key findings:
Anaesthetic machines were being used to provide ventilation to patients for long periods of time. The machines were being used for a function that they were not designed for.There was a lack of expertise within the clinical team working in the ICU – it was noted that non-anaesthetic ICU consultants were not familiar with the anaesthetic machines being used.The correct use of filters and their position within the circuit was complicated and may not have been clear to all ICU staff.There were multiple filers available for use with the machines and it was not immediately obvious on sight which filters were HME. Suctioning was undertaken by staff with limited expertise and the machines in use may not be as effective as standard ICU suction machines.There were different types of ventilators in place which may have contributed to potential confusion regarding what each patient needs.
Recommendations:
A checklist of the ventilator circuit is written and implemented at the start of every shift, to be completed by the anaesthetist and ODP to ensure correct circuit set up and humidification. Gain assurance that bedside nursing staff are clear on the mechanism for checking suction machines. Swap out anaesthetic machines for ICU ventilators with appropriate humidifiers within the circuit – nullifying the need for HME filters.There needs to be further discussion with NHSI/Supply chain regarding equipment for patient ventilation at NHL.The risk associated with using anaesthetic machines as ventilators at NHL is escalated to the hospital risk register. Advertisement
He continued: ‘We were offered beds at the Nightingale Hospital and we chose patients that were physiologically stable to transfer.
‘The Nightingale team over the course it existed had an admission criteria that slightly changed throughout the pandemic.
‘But any of the patients that fulfilled the criteria would be considered for transfer.
‘A form would be emailed centrally which would involve a list of criteria and then it would be emailed to the Nightingale team for them to decide which patients they would take.’
He added: ‘It was entirely appropriate to transfer Mr Patel. He was physiologically stable and our priority was to create critical care capacity.’
Munita Grover, consultant in anaesthesia and critical care at Northwick Park hospital told the court her decision to transfer Mr Patel to the Nightingale was based on the strict criteria set out by the field hospital in London.
She said: ‘My care and involvement commenced on April 5 at Northwick Park Hospital. At the time we were on 12 hour shifts as consultants which deviated from our normal pattern.
‘Mr Patel was brought into the hospital on April 4 and his symptoms were a loss of smell, lethargy a cough with brownish sputum’
On April 7, Dr Grover said she highlighted Mr Patel as a possible patient for transfer but was unaware of equipment issues at the Nightingale.
She continued: ‘We heard that the Nightingale were offering beds to patients and we agreed that according to the criteria set out by the Nightingale Mr Patel met the criteria.
‘I highlighted Mr Patel as a transfer patient.’
She added: ‘We knew they could take patients on ventilators with a low dose of noradrenaline but not anyone with further organ requirements.’
Ms Persaud asked: ‘Were you aware that some patients were being ventilated with anaesthetic machines at the Nightingale?’
Dr Grover said: ‘No I didn’t know of equipment issues at the hospital.’
When asked by Ms Persaud if a clinical diagnosis of Covid by doctors was enough given that Mr Patel did not have a PCR test confirming a coronavirus diagnosis before transfer, Dr Grover added: ‘Yes.’
Ms Persaud went on to ask the consultant: ‘If you didn’t know about the service by the Nightingale how could you determine the optimal care pathway would be provided?’
Dr Grover replied: ‘We were asked to highlight patients based on the physiological criteria by the Nightingale.
‘The patient was ventilated and on a low dose of noradrenaline so the assumption was that would be OK.’
During his stay at the Nightingale, Mr Patel was put on a ventilator and his family would receive daily calls from a telephone operator at the Nightingale about his health.
However on the evening of April 18, a doctor at the hospital discovered Mr Patel’s ET tube had become blocked with secretions due to an incorrect filter in his ventilator circuit.

The report also said that ventilation was being provided to the majority of patients using anaesthetic machines – which are designed to provide short term ventilation in the operating theatre under the use and supervision of an anaesthetist

The report sent from the health trust to Mr Patel’s family said there was a lack of expertise within the clinical team working in the ICU and the correct use of filer and their positions within the circuit was ‘complicated’ and may not have been clear to all staff

The report also said that ventilation was being provided to the majority of patients using anaesthetic machines – which are designed to provide short term ventilation in the operating theatre under the use and supervision of an anaesthetist
Ms Lee and her family were called the following day and told the wrong filter had been used in Mr Patel’s breathing machine. The member of staff apologised for the incident and said a letter would be issued.
What are Heat and Moisture Exchange (HME) filters? 
Heat and moisture exchangers (HME) can be placed at the patient’s end of the breathing system
In normal breathing, air is filtered, warmed and moistened by the nose and the upper airway.
However when endotracheal intubation – a procedure in which a tube is inserted through the mouth into the trachea – is performed on a patient this can result in an increased build up of mucus secretions.
This can increase the risk of infections and cause blockages in the breathing tube.
In order to combat this a heat and moisture exchangers (HME) can be placed at the patient’s end of the breathing system.
The filters humidify the airway in circuits.
Lack of any humidification in the circuit will increase likelihood of secretions becoming thickened – blocking the patient’s airways and ET tube.
Anti-viral filters will also be used to prevent contamination between patient and the ventilator machine.
Advertisement
However on April 26, Mr Patel’s 23-year-old son Anish received a call telling him his father was dying and that he should go to the Nightingale as soon as he could to say his goodbye.
A month later, Barts Health Trust sent the family a Serious Incident Report that confirmed that ten ventilated patients had been identified as not having heat & moisture exchange (HME) filters within their ventilator circuits – with harm recorded for three of these patients.
The report said Mr Patel required re-intubation after his ET tube was found to be blocked.
It went on to suggest a number of reasons that could have led to the error, including a ‘lack of expertise within the clinical team working in the ICU’ and ‘potential confusion regarding what each patient needs’ due to the different types of ventilators in place.
The report said there were ‘multiple, potentially confusing disposable filters’ available for staff and it would not have been ‘immediately obvious on sight which filters are HME’.
It added the correct use of filters and their position within the circuit was ‘complicated’ and may not have been clear to all ICU employees before going on to state that suctioning was undertaken by staff with ‘limited expertise’.
The report also said that ventilation was being provided to the majority of patients using anaesthetic machines, which are designed to provide short term ventilation in the operating theatre under the use and supervision of an anaesthetist and operating department practitioner (ODP).
When used in the ICU setting these machines can create a ‘high risk scenario’, with the use of filters within the machines being one of them, according to the report.
Mr Patel’s son Anish was also sent a letter of apology from Barts Health Trust which said the filter error had ‘reduced effectiveness of the circuit’ and ‘contributed to his father’s deterioration on 19th April’.
A section of the letter read: ‘We discovered that an issue had occurred with the filter in the breathing circuit that was providing ventilation to your father. The wrong filter had been placed in the circuit and as a result the circuit was not functioning as effectively as it could be.
‘We feel that the reduced effectiveness of the circuit and contributed to his deterioration on 19th April; it is very difficult to say if this event contributed to his sad death.’
In August, Ms Lee described how the temporary hospital, which was the first of the Nightingale hospitals to open, was not equipped to meet the demands of the pandemic.
She said: ‘It was a fast train going at high speed, but it didn’t have a driver.
‘It wasn’t equipped with sufficient equipment and staff lacked expertise. It was a catastrophe.
‘I also don’t feel my brother should have been transferred there in the first place. ‘

The field hospital, which shut its doors on May 15, was set to hold up to 4,000 Covid-19 patients

Barts Health trust said the incident would have ‘reduced effectiveness’ of the ventilator and ‘contributed to Mr Patel’s deterioration on April 19’

Earlier this year it emerged that a second patient, Kofi Aning, 66, from Enfield, north London, who worked as a carer, was also among the patients to have been affected by a wrong filter in his breathing system.
He passed away on April 23.
In August a Barts Health spokesperson said: ‘We offer our deepest sympathies to Mr Patel’s family.
‘We have fully investigated the circumstances, changed our practice accordingly and do not believe that the incident with the filter was a direct cause of Mr Patel’s death.
‘This will be further considered by the coroner at the inquest.’
The Nightingale Hospital in London, which was opened by Prince Charles on April 3, was one of seven temporary hospitals opened to great fanfare at the start of the pandemic last year, along with centres in Birmingham, Manchester, Exeter, Harrogate in North Yorkshire, Bristol and Washington in Tyne and Wear.
Prior to its opening, images from inside the field hospital showed military personnel erecting cubicles and carrying equipment into the transformed centre- which was set to hold up to 4,000 Covid-19 patients.
The centre was hastily put up in less than two weeks in March, amid fears the capital’s hospitals could be overwhelmed by spiralling Covid-19 admissions.
However by May 6, 2020, the Government dashboard showed only five patients remained at the facility and just six weeks later the hospital was moved to ‘standby’ and closed its doors on May 15.
The inquest continues.
Source link : https://www.dailymail.co.uk/news/article-10060077/Londons-Nightingale-hospital-did-not-systems-care-needed.html











