Some Americans who got Johnson & Johnson’s one-dose COVID-19 vaccine are seeking out booster shots of other vaccines despite the practice not recommended by U.S. health officials.
Those seeking extra doses want more protection as the Indian ‘Delta’ variant spreads across the U.S. cases with studies showing that J&J is less effective against it than the Pfizer and Moderna vaccines.
Other studies have suggested that boosters may be necessary for cancer patients, organ transplant recipients, and others with weakened immune systems.
Countries including France, Israel, and South Korea are allowing boosters and mix-and-match shots for certain patients – including those who are immunocompromised.
But in the U.S., although the practice is legal, health officials are still looking into safety concerns.

Americans who received the J&J vaccine are seeking out additional doses from other manufacturers. Pictured: A Los Angeles resident gets vaccinated at a mobile clinic on July 9
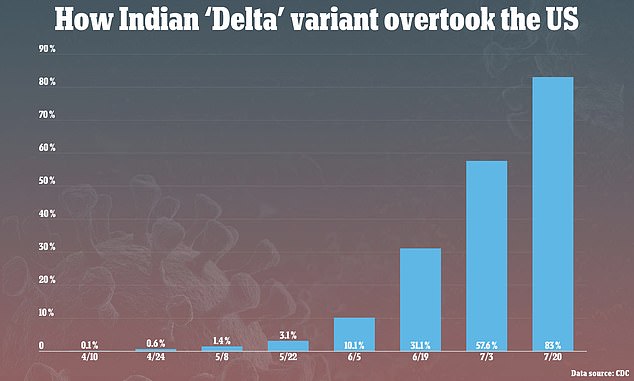
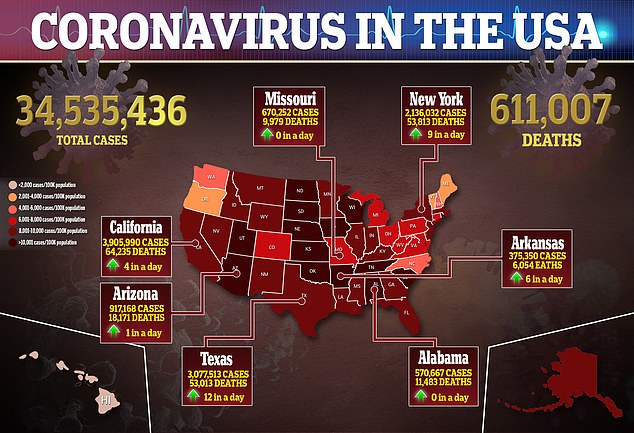
One reason for boosters is the Delta variant, which now accounts for the vast majority of cases in the U.S. after an exponential rise this spring and summer
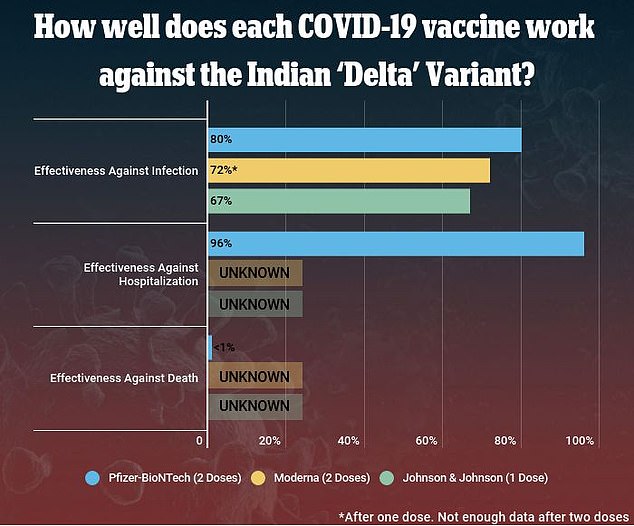
Several studies have shown that the Pfizer-BioNTech and Moderna vaccines are more effective against the Delta variant the J&J vaccine
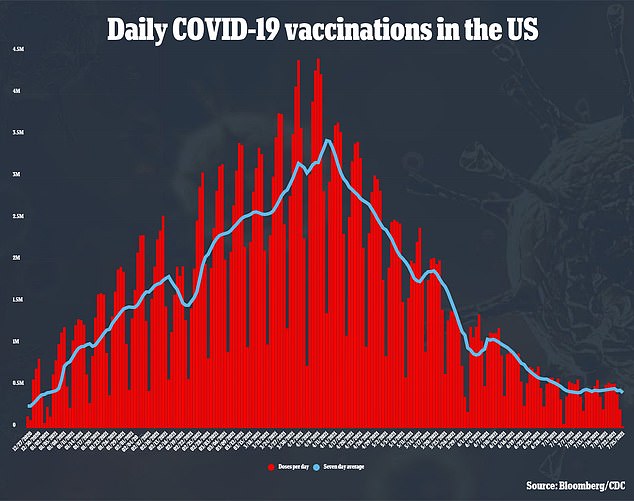
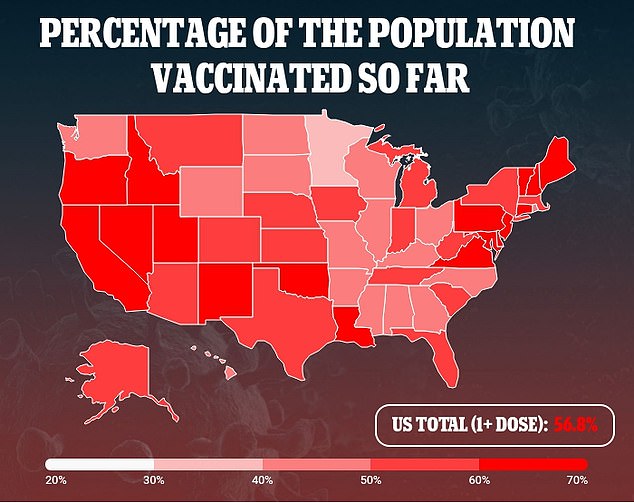
Covid booster shots – or mix-and-match regimens – aren’t recommended by the Centers for Disease Control and Prevention (CDC) but some Americans are seeking out additional vaccine doses anyway.
The strategy may be a way to protect against the Delta variant, scientists say.
This variant is now dominating cases in the U.S. It’s causing at least 83 percent of cases nationwide as of mid-July.
People infected with the Delta variant are super-contagious, with about 1,000 times as many copies of the virus in their respiratory tracts compared to people infected with the original strain of Covid.
As a result, those patients who received the JJ&J or AstraZeneca vaccines – which are less effective than Pfizer and Moderna – may want a boost to their immune systems.
One such patient is Dr Angela Rasmussen, a virologist at Georgetown University who described her choice in an interview with CNBC.
Rasmussen originally opted for a J&J shot in April.
She was planning to move from Seattle to Canada, and was concerned that she’d be unable to complete a two-dose regimen due to supply concerns in Canada during the spring.
But once Delta started making headlines, she sought additional protection against the variant.
‘Once the supply issues were addressed here in Canada and there really wasn’t a supply shortage of the mRNA vaccines, I decided to go get a Pfizer shot just because I thought that at the very worst, it couldn’t hurt,’ Rasmussen told CNBC.

The J&J vaccine is about 70 percent effective against illness from Delta, while Pfizer and Moderna are closer to 90 percent effective. Pictured: A health worker gives a J&J shot at a homeless shelter in Bogota, Columbia on July 2
Studies have shown that the J&J vaccine is about 70 percent effective at protecting recipients against illness from the Delta variant.
The Pfizer and Moderna vaccines, meanwhile, are closer to 90 percent effective against this variant, though different studies have shown values between 64 and 96 percent.
Still, all three vaccines are very good at protecting patients against severe disease and death from Covid – which public health officials say is the most important reason to get vaccinated.
‘Even though we are seeing infections after vaccination… the effectiveness against severe disease is still substantial, which is, yet again, another argument which all of us say continually: “Get vaccinated. It offers good protection against disease,”‘ Dr Anthony Fauci said at a press briefing last week.
The situation is more complicated, however, for patients with weakened immune systems due to cancer treatments, organ transplants, and other conditions.
While some studies have shown that Covid vaccines successfully produce an antibody response in these patients, others show that certain groups of patients – such as those who received organ transplants – are not well-protected after vaccination, especially after a single dose.
As a result, the CDC is considering a recommendation of booster shots for these patients.
An advisory committee to the agency met last week to evaluate evidence for this recommendation, though a formal decision can’t be made until the Food and Drug Administration (FDA) approves a third shot.
In other countries, however, booster shots and mix-and-match regimens are available for patients with weakened immune systems and other specific populations.
France and Israel are both offering third doses to immunocompromised patients.
A mix-and-match regimen is the norm in Italy – where adults under age 60 are no longer eligible for the AstraZeneca vaccine due to cases of blood clotting. Those who got a first dose of this vaccine may receive a different shot for their second dose.
Meanwhile, in South Korea, about 760,000 people have received a first dose of AstraZeneca and a second dose of Pfizer due to shipping delays.
Studies on these mix-and-match regimens – including a paper published Monday in Nature – have suggested that patients receiving doses of two separate vaccines may have stronger immune responses than those who receive two doses of the same vaccine.
This is especially true for those who receive doses of vaccines that protect against Covid through different mechanisms, such as one AstraZeneca dose and one Pfizer dose.
‘If you’re using a vectored vaccine, like the J&J or AstraZeneca, which use adenovirus, you generate antibodies against the vector so that your second shot with the same vector makes it less likely to induce a robust immune response,’ Yale immunologist Dr Akiko Iwasaki told CNBC.
In fact, it’s common to mix and match vaccines to protect against HIV and other diseases.
Still, there may be some safety concerns – an issue the National Institutes Health is currently examining with a mix-and-match vaccine trial that began in June.
The World Health Organization, like the CDC, is not recommending mix-and-match vaccine regimens at this time.
Dr Soumya Swaminathan, the organization’s chief scientist, recently said the practice is a ‘data-free zone’ and called for more safety investigations.
Once more data are available, however, it seems likely that additional shots may be recommended for immunocompromised patients, those who received J&J shots, and other populations.
Source link : https://www.dailymail.co.uk/health/article-9831405/Americans-got-Johnson-Johnsons-Covid-vaccine-mixing-matching-booster-shots.html











