
Dr John Chisholm, chair of the BMA’s medical ethics committee, said the neutral position means the association will not lobby for or against a change in the law, but represent the views, interested and concerns express by its members.
Britain’s biggest union for doctors today dropped its 15-year stance opposition to assisted dying.
The British Medical Association, which represents around 150,000 members, held a landmark vote after a survey last year revealed the majority supported a change to the law.
More than 300 members of the BMA’s representative body participated in the poll.
A slim majority backed the change to adopt a neutral stance on the issue.
Slightly fewer than half of the BMA members who voted did so in favour of holding a neutral stance on assisted dying. Another 48 per cent were against it and 3 per cent abstained.
But, it assisted dying becomes legal, they said they would support medics’ right to refuse prescribing lethal doses of medication to patients if they object.
Assisted suicide is currently illegal. Anyone caught helping or encouraging someone to take their own life faces up to 14 years in prison.
But euthanasia, which is the act of a doctor deliberately giving a terminally ill patient a drug they don’t need with the sole aim of ending their life, is regarded as either manslaughter or murder. Offenders face spending the rest of their life in prison.
Assisted dying sparks strong debate from both sides, with some arguing that no one should be intentionally deprived of their right to live.
But others say the blanket ban causes needless suffering for terminally ill patients and their families.
Dr John Chisholm, chair of the BMA’s medical ethics committee, said the union’s neutral position means the association will not lobby for or against a change in the law, but ‘represent the views, interested and concerns’ expressed by its members.
The move comes after more than 100 medics penned a letter calling for the BMA to end its opposition to assisted dying.
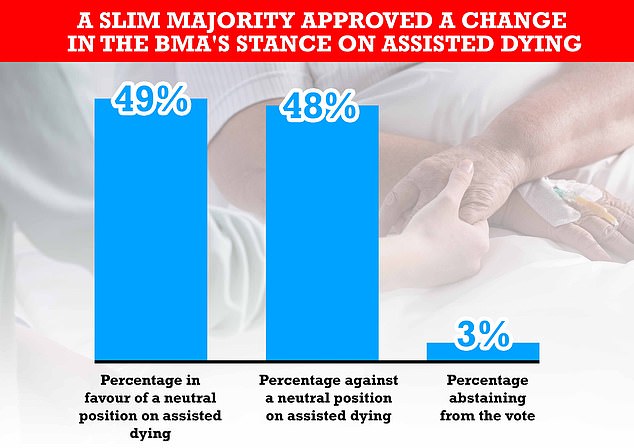
Some 302 members of the BMA’s representative body, out of the 560 eligible, participated in the landmark vote. Some 49 per cent supported a change in stance, while 48 per cent were against it and three per cent abstained from the vote
Doctors and medical student representatives at the BMA’s annual representative meeting, which was held virtually, debated the issue today.
Just 54 per cent of the 560 members of the union’s representative body who were eligible to participate decided to vote.
While the body passed the motion to support people choosing to end their life, they also said they would safeguard healthcare workers right to refuse engaging in the act.
The vast majority (79 per cent) voted in favour of healthcare staff being given the right not to assist death if the law changes.
What is the law on assisted dying?
There are two types of assisted dying. Both are currently illegal in England.
Euthanasia is the act of deliberately ending a person’s life to relieve suffering, such as a doctor deliberately giving a patient with a terminal illness a drug with the aim of ending their life.
Offenders face spending the rest of their life in prison.
Assisted suicide is when someone helps another person to kill themselves, such as providing a family member with a fatal amount of medication, while knowing they plan to use it to commit suicide.
Anyone caught helping or encouraging someone to take their own life faces up to 14 years in prison.
Assisted dying is also illegal in Wales under the Suicide Act 1961, and in Northern Ireland under the Criminal Justice Act 1966 which says anyone who ‘encourages or assists a suicide’ is liable to up to 14 years in jail.
There is no specific crime of assisting a suicide in Scotland, but it is possible that helping a person to die could lead to prosecution for culpable homicide.
A bill to legalise assisted dying in Scotland was brought forward by a Liberal Democrat MP Liam McArthur in June.
Advertisement
But 72 per cent said medics who object to assisted dying should still provide factual information to any decision-making body about the practice.
And doctors who would refuse to provide assisted dying services, if it becomes legal, should refer patients seeking that form of care to another medic, the majority said.
The series of votes follow on from a poll by the BMA last year on whether there should be a change in the law to permit doctors to prescribe life-ending drugs to eligible patients.
Some 40 per cent said they think the association should actively support attempts to change the law, a third said it should oppose assisted dying and 20 per cent said the BMA should adopt a neutral position.
And in that poll, half of surveyed members said they personally believe the law should change to allow doctors to prescribe life-ending drugs, while four in 10 were against it and 11 per cent were undecided.
Dr John Chisholm, BMA medical ethics committee chair, said: ‘Assisted dying is a highly emotive and sensitive topic that inspires a broad spectrum of views and opinions both across the wider public and among the medical profession, for whom any change of law would have a profound impact.
‘As evidenced by the results of our recent survey of the profession and in today’s in-depth debate, doctors have a wide range of personal views on this important issue, and as such representatives have decided that the most appropriate position for the BMA, as the professional body which represents all doctors and medical students in the UK, to hold is to be neutral on the topic.
‘This is an important day for the BMA and the medical profession, clearly demonstrating that we as an organisation are listening to our wider membership on such a crucial issue, and developing policy based on their valuable feedback.
‘Moving to a position of neutrality means that the BMA will not lobby for or against a change in the law, but far from remaining silent on the issue, we will continue to represent the views, interests and concerns expressed by our members.’
On the need for healthcare workers to have the right to conscientiously object to participation, Dr Chisholm added: ‘Indeed, as with many other issues that ignite such deeply held personal beliefs in healthcare staff, it is vital that these are respected and protected should there be any change in law.
‘The need for the right of doctors to conscientiously object to participation in physician-assisted dying was something that was made overwhelmingly clear not just in today’s discussions, but also in the results to our survey, which found that 93% of respondents supported this.
‘As medical professionals, we believe that it is our first responsibility to preserve life.
‘But that does not mean we should prolong it at any cost.’
They added that ‘strong palliative medicine and the choice of an assisted death are not mutually exclusive’.
More than 100 leading doctors in the UK yesterday urged the association to no longer oppose assisted dying and adopt a neutral position.
In a letter published in the Guardian, the medics wrote: ‘In an era when modern medicine can extend the length of an individual’s life, but not necessarily its quality, we believe that those with terminal or incurable conditions deserve a choice about how, where and when they die.’
Dr Gillian Wright said: ‘This motion is actually about euthanasia, the BMA defines physician-assisted dying as assisted suicide and euthanasia.
‘We know that neutrality means tacit approval and has enormous political significance.’
The move was welcomed by some campaign groups, with Dignity in Dying chief executive Sarah Wootton branding it ‘a victory for common sense’.
She said: ‘This is an historic decision and a victory for common-sense.
‘It brings the BMA in line with a growing number of medical bodies in the UK and around the world that truly represent the range of views that healthcare professionals hold on assisted dying.
‘By adopting a position of engaged neutrality the BMA can now proudly and accurately advocate on behalf of its members, while sending a message to Parliament that assisted dying is, rightly, an issue for society, where the views of dying people and their loved ones should be heard loud and clear.’
But Care Not Killing chief executive Dr Gordon Macdonald said that current laws protect vulnerable people and do not need changing.
He added: ‘We are naturally disappointed at the divisive nature of this vote as it exposes the divide between doctors who care for patients at their end of life, whether in hospitals or hospices, who oppose assisted suicide and euthanasia and those medics who work in unrelated discipline such as child and adolescent psychiatry and occupational health.
‘As the BMA’s own survey found, doctors at the coal face who deliver care to the elderly and terminally ill, who work in palliative care, geriatric medicine and general practice continue to oppose assisted suicide and euthanasia, because they know it is not needed and the subtle pressure it could put on patients to end their lives prematurely.’
Source link : https://www.dailymail.co.uk/news/article-9989011/Britains-biggest-doctors-union-BMA-drops-15-year-opposition-assisted-dying.html











