Health chiefs have ordered a review of Covid rules in a move that could pave the way to more face-to-face GP appointments.
It comes less than a week after the Daily Mail launched a campaign to secure better access to family doctors.
GPs claim an ongoing two-metre social distancing rule stops them seeing more patients in person because waiting rooms are too small to accommodate them.
NHS England insists the requirement, which is specific to healthcare, should not prevent GPs from seeing people face to face.
But the number of consultations taking place in surgeries has plummeted from 80 per cent before the pandemic to just 57 per cent this July.
The huge rise in telephone and video consultations has sparked fears that serious diseases such as cancer are being missed.
The Prime Minister has himself stressed the importance of face-to-face appointments, warning: ‘I am absolutely certain that unless we can deliver that there will be people sadly whose symptoms are not picked up and who will suffer as a result.’
The Department of Health last night launched a review into infection prevention and control (IPC) measures across the NHS, which could see the limit of two metres reduced – or scrapped entirely.
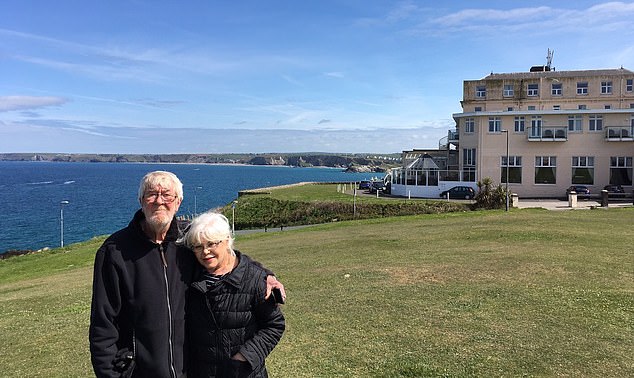
June Walker, 67, first called her family doctor about her constant headache and sore shoulder last November. However, with no GP prepared to see her in person, she was simply referred for physiotherapy

Health chiefs have ordered a review of Covid rules in a move that could pave the way to more face-to-face GP appointments
Months of pain because I couldn’t see a doctor
A retired estate agent endured eight months of excruciating headaches because her GP would not see her face to face and take her blood pressure.
June Walker, 67, first called her family doctor about her constant headache and sore shoulder last November.
However, with no GP prepared to see her in person, she was simply referred for physiotherapy.
But the headaches failed to improve and – despite repeatedly ringing her surgery – she was not able to see her GP.
Only when she was admitted to hospital as an emergency for another problem, in June, was her blood pressure eventually taken.
Surgeons wanted to perform a colonoscopy, but refused after realising her blood pressure was off the scale.
They wrote to her GP and she was put on blood pressure tablets, which have cured the headaches. Last night she said: ‘I had a terrible headache every single day for eight months that was completely unnecessary.
‘Taking your blood pressure and listening to your chest used to be the first thing a GP did when you went to see them.
‘If I had been able to see my doctor in person in November I could have saved myself so much pain.
‘Some things simply can’t be diagnosed over the phone. I went from taking 120mg of codeine every day to nothing – it’s like a miracle.’
She said she was being prepared for a major operation at hospital for a separate medical issue ‘when they took my blood pressure and refused to do it.
‘The doctor said he was worried I would have a stroke on the table.
‘Only then did it become an emergency, but I’d been walking around for months with it, it was scary.’
Mrs Walker, of Aylesbury, Buckinghamshire, added: ‘I feel very let down by my GP practice. If I had seen a GP and had my blood pressure taken it would have relieved me of eight months of terrible pain and I would have been safeguarded from any potentially life threatening illness.’
Mrs Walker, who is married to production manager, Noel, 71, and has seven grandchildren, said she ‘absolutely’ supported the Mail’s campaign to get patients seen by GPs face to face.
‘I am so pleased that the Mail has taken up this issue,’ Mrs Walker added.
‘It’s appalling that GPs seem to hold themselves on a pedestal and aren’t prepared to treat their patients.’
Advertisement
A source said: ‘The review will examine which rules need to stay in place and which can now be safely dropped or amended. It is too soon to know what the outcome will be, but it will consider the obstacles that GPs have used to avoid seeing patients face-to-face.’
Dr Lisa Cameron of the SNP, chairman of the all-party health group in Westminster, said yesterday: ‘It’s great news that the Government is finally acting. It is time these guidelines are reviewed because most people are now double-jabbed, meaning they are much less likely to get significantly ill if they catch Covid.
‘I’m really concerned with the difficulty people are having securing appointments and the situation is now critical.
‘We need to start getting more people to their GP face to face. If GPs can’t fit lots of people in their waiting room they should stagger appointments better.’
NHS England introduced widespread remote consultations in March last year in a bid to control the spread of coronavirus at the start of the pandemic.
It wrote to surgeries this May, telling them that virtual appointments could carry on when doing so is beneficial.
However, it made clear that they should be an option ‘alongside a clear offer of appointments in person’.
It added: ‘Patients’ input into this choice should be sought and practices should respect preferences for face-to-face care unless there are good clinical reasons to the contrary – for example, the presence of Covid symptoms.’
Doctors have pointed to separate guidelines on infection control produced by the NHS and Public Health England, which state that practices must enforce two-metre social distancing and the use of face masks.
Dr Chaand Nagpaul, chairman of the British Medical Association, has written to Health Secretary Sajid Javid, claiming GPs who fail to see patients face to face are simply following these rules.
A poll for the Mail this week found that 85 per cent of people believe they should be able to have a face-to-face consultations if they want one. Yet a study has revealed that GP access of any kind has now become a postcode lottery.
In the worst-hit district, North East Lincolshire, just 35.8 per cent of patients get to see a doctor either in person or via a Zoom call according to the latest figures covering July.
The rest of those seeking a GP consultation were referred instead to a nurse or another member of practice staff. At the other end of the scale, almost twice as many people – 67.1 per cent – of those in South Sefton in Liverpool were seen by their GP.
The analysis from the Liberal Democrats also shows a massive disparity across the country when it comes to same-day appointments.
In the worst area, the Vale of York, just 38 per cent of consultations took place on the day they were requested – compared with 57 per cent in the top-performing area, Blackburn with Darwen.
Lib Dem health spokesman Munira Wilson said: ‘These figures reveal the postcode lottery facing GP patients, with people in some areas struggling to see a doctor or get a same-day appointment.
‘The Conservatives are failing to get to grips with this worsening crisis, with growing NHS waiting lists piling more pressure on GP surgeries. People deserve a fair deal where they can get an appointment with their local GP when they need one.
‘We need to see urgent action to train more GPs, boost funding for practices and ensure the vaccine booster programme doesn’t overwhelm them further.’
This week saw the Mail issue a five-point manifesto for change which includes a call for the Government to make good on its pledge to deliver 6,000 more GPs.

June Walker (pictured) endured eight months of excruciating headaches because her GP would not see her face to face and take her blood pressure
If I hadn’t seen my patient in person, he’d have died… that’s why it would be a disaster to rely on remote appointments
By Martin Scurr, Retired GP and Daily Mail Good Health Expert
Some weeks ago one of my former patients, a man in his mid-70s, asked if I would meet him.
As we made our way to a coffee outlet near his office, I noticed he’d developed a shuffling gait, though what he actually wanted to discuss was how he suddenly felt old.
While I could see no evidence of tremor, I was convinced that he might have Parkinson’s disease and urged him to see a neurologist.
Within days he’d undergone a brain scan and a lumbar puncture to collect cerebral spinal fluid, and was diagnosed with a brain condition I’d never come across, caused by a dangerous build-up of fluid.
He underwent urgent neurosurgery to drain the fluid – and within 24 hours he was cured, back to his old self.
This story highlights just why face-to-face consultations matter so much.
‘Doctoring’ isn’t simply about patients telling you their symptoms – the vital skill is in observing the unspoken signs, their demeanour, how they move, even the way their skin looks, the non-verbal communication.
1 in 3 who can’t speak to GP go without care
One in three people who are unable to secure a GP appointment end up going without any care, an NHS study suggests.
The GP patient satisfaction survey of 850,000 raises concerns that sick Britons are being left to suffer and deteriorate at home.
It revealed that 32 per cent of those who failed to speak to their family doctor in-person or remotely did not speak to anyone else about their medical condition.
And 8 per cent went to A&E for help, piling pressure on already busy hospitals.
The poll found that more than two in five patients had avoided making an appointment in the past 12 months.
They were either worried about the burden on the NHS or else were concerned about Covid risks.
Patient groups also warned that some people may have given up because they have tired of the struggle to secure an inperson or remote appointment.
Professor Martin Marshall, chairman of the Royal College of GPs, said that although there was little evidence, ‘I think it’s probably reasonable to suggest that when… patients feel perhaps they can’t get access to their GP, then they will go into the emergency department because the lights are on’.
An NHS spokesman said 70 per cent of patients said their ‘overall experience of making an appointment was good – up five per cent on 2019.
Advertisement
It’s about spotting the symptoms the patient themselves might not have noticed – such as this man’s change in gait.
The fact is, without seeing a doctor in person, he would probably have died after months of deteriorating health and senility. And I have little doubt an online consultation would not have led to the brain scan that diagnosed this man in time.
But that is where we are at this point, with alarming figures showing that in parts of England, less than half of patients see their GP face to face. As a result, illnesses are being missed.
The Mail recently reported the desperately tragic story of 27-year-old Jessica Brady, from Stevenage in Hertfordshire, who died of liver cancer after a series of virtual appointments over five months failed to spot her tumour.
And while I fear the elderly and vulnerable are particularly at risk from the inadequacies of remote medicine, her story demonstrates that no one of any age is immune.
One of the key things you miss with online or phone consultations is physically examining a patient. At medical school we were taught: ‘If you don’t put your finger in it you will put your foot in it.’
There is no doubt actually examining patients saves lives, and without the return of more face-to-face consultations, I predict more tragedies – and increasing litigation.
I no longer want to have friends tell me of terrible stories, such as the accountant I know who suffered a fall at home and was only permitted a telephone consultation. Painkillers were prescribed ‘to help the pain of the bruising’ but that was the only care offered.
After two days bedridden at home he eventually rang an ambulance, and went to hospital where he was diagnosed with a fractured thigh – a serious injury, and potentially lethal. He was lucky: he survived. But it shouldn’t have been a life and death situation.
The pendulum has swung too far. I fully support the Mail’s campaign to get more patients in front of their GPs, but we need to think where the solution lies – and that’s not in the hands of the individual GP, or even edicts from government ‘requiring’ more face-to-face appointments.
For while I suspect there are some individual GPs who would prefer the new status quo, because it’s simpler, saves time and helps cut waiting lists, it is too simplistic to say ‘it’s the doctors’ fault’ – or worse, ‘they’re lazy’.
For the fact is this was a juggernaut of governments’ making: we just don’t have enough GPs.
Well before the pandemic, patients were finding it difficult to see a GP, with too many having to wait days or even weeks.
The blame for this – and now, the online mess – lies at the door of successive governments who are guilty of gross failures of forward planning. Put simply: they’ve failed to ensure there are enough GPs.
For instance, it was obvious that allocating more medical school places, quite rightly, to women, from 10 per cent in the 1960s, to 50 per cent, would eventually create manpower difficulties as women needed time out to have families.

‘Doctoring’ isn’t simply about patients telling you their symptoms – the vital skill is in observing the unspoken signs, their demeanour, how they move, even the way their skin looks, the non-verbal communication
At the same time more GPs began retiring early – the demands of an ageing population, and escalating obesity and diabetes, hugely increased workloads, while red tape spiralled out of control – dealing another crushing blow.
The shortage of GPs along with the workload had already compelled doctors to devise additional ways of providing at least some sort of service, which led to telephone consultations.
The fact is, online and phone consultations do have their use – for instance, a brief assessment before sending a patient to the right place for minor problems, or for then shifting the case to the practice nurse.
Remote consultations are particularly suitable and safe when the GP and patient know each other.
I remember my heart sinking last year when then health secretary Matt Hancock said all GP appointments should be done remotely by default, unless a patient needed to be seen in person.
This would be disastrous. While there is no doubt remote consultations are here to stay, it’s time the default is for patients to be back in front of their GPs.
It can be done: just look at secondary care – treatment in hospitals – which is functioning well, with consultants clearing the waiting list backlog, doors wide open, and skilled personnel getting on with the job. Face to face.
So how can we get out of this mess? One of things we need is a campaign to bring back retired GPs to assist with triage, patient workloads, and the continued winter vax programmes. Hitherto this has been blocked by impossible and frustrating bureaucracy.
When the pandemic emerged I was reinstated by the General Medical Council within 24 hours and by my insurer the Medical Defence Union the following day.
All that happened quite spontaneously and without asking, and I readily complied.
Yet NHS England, despite that acknowledgement by the GMC of my suitability, required a copy of my passport, a utility bill, and 29 pages of questions to be answered. I did all of this but never heard any more.
And I know from frustrated peers, I was not the only one. Slash red tape to ensure this can’t happen.
What about setting up pop-up GP centres at A&E units or other venues to ease the backlog, with staffing from healthcare assistants and other nursing staff for non-critical care – and some of those retired GPs!
We also need a strong advertising campaign to encourage greater use of pharmacists – and clear guidelines about when a ‘e-consultation’ is appropriate.
Last but not least in the longer term, we need more GPs.
Source link : https://www.dailymail.co.uk/news/article-10023339/Covid-curbs-waiting-rooms-review.html











