Hospitalised Covid patients who have low antibody counts face a higher risk of dying from the virus than those with high levels, a study has confirmed.
Spanish researchers looked at nearly 100 critically ill coronavirus sufferers in ICUs in the first wave of the pandemic last spring.
They measured the levels of antibodies – virus-fighting proteins produced in response to infection – in their blood during their hospital battle.
These levels are a good indication of how well the immune system is firing.
The study found patients who had the lowest amount of antibodies were the least likely to survive the illness.
They also had the highest viral load, showing their bodies were struggling to stop the virus from multiplying.
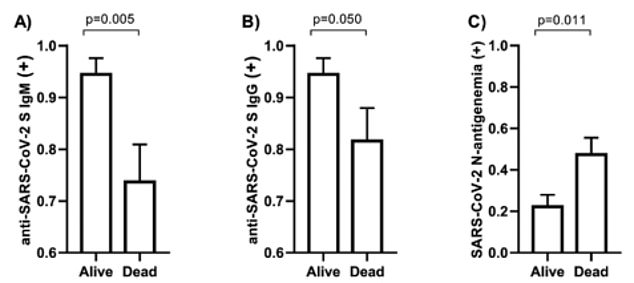
The graphs show the level of Covid antibodies (left and middle graphs) and the amount of the virus present in the blood samples (right graph) of patients hospitalised with the virus in Spain, in relation to survival rates. The figures show that those who formed a more robust immune response against the virus were more likely to survive, while a higher viral load was linked with dying from the virus
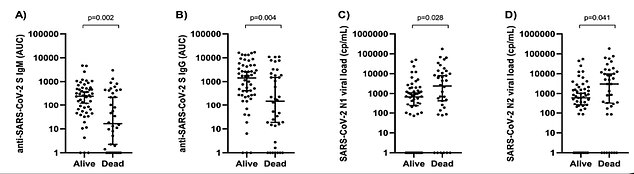
The graphs show level of Covid antibodies IgM and IgG (left graphs) and the amount of the virus present in the blood samples (right graphs) among patients hospitalised with the virus in Spain, in relation to whether they died from Covid or survived it 30 days after admission. Low levels of the antibodies was a risk factor for subsequently dying from the virus, while a low viral load increased the chance of survival
Antibodies are molecules that bind to Covid’s spike protein (pictured) — which the virus uses to invade cells — to it from multiplying in the body.
The researchers, from Spain’s National Centre for Microbiology found, said their findings could help identify the ‘optimal’ antibody levels needed to recover.
Antibodies are molecules that bind to Covid’s spike protein — which the virus uses to invade cells — to it from multiplying in the body.
They make up one part of a broader immune response to the virus, which also includes memory cells.
These T cells are harder to measure and remember how to fight an infection long after antibody levels fade.
Antibodies can come from natural infection or vaccines and there is intense scientific debate over which response is stronger and longer-lasting.
The study, published in the Journal of Internal Medicine, examined blood samples taken from 92 critically ill patients at two hospitals in Spain who tested positive between March 16 and April 15 last year.
Professor Lockdown says ministers may need to resort to winter Covid ‘Plan B’ if daily admissions breach 1,200
England may have to resort to its winter Covid ‘Plan B’ if daily hospital admissions for the virus breach 1,200, ‘Professor Lockdown ‘ Neil Ferguson suggested today.
Boris Johnson announced last month that masks, social distancing and vaccine passports might need to be brought back if the NHS comes under unsustainable pressure.
Ministers said the trigger point will be hospital rates now that the jabs have made case numbers less important — but they have not put a threshold on admissions.
Professor Ferguson — a key Government adviser whose modelling prompted the first lockdown last March — suggested that England should not tolerate more than 1,200 daily hospitalisations.
Speaking to a cross-party committee of MPs today, he said that the country was currently recording 600 Covid admissions per day.
He added: ‘If that figure were to double, we’d need to think about moving to “Plan B”.’ The Imperial College London epidemiologist called for ‘more intense’ curbs if there is a sharp rise in admissions.
To get ahead of a winter wave, he said second doses for 16 and 17-year-olds could be brought forward and advised we are ‘more aggressive’ in administering boosters.
Advertisement
They examined how much of two different Covid antibodies – called IgM and IgG – that the patients had in their blood within the first 24 hours of being admitted to hospital.
Ten patients had no detectable levels of the IgG antibody, while the IgM antibody was not detected in 13 patients.
Patients who died were more likely to have no or low levels of these two markers, the team said.
Older people struggle to mount much of an immune response, so too do immunosuppressed people or those with underlying heath conditions.
That’s why they were targeted first with vaccines and why they are most vulnerable to the virus.
The Spanish researchers noted that patients in their study with the lowest antibody levels were admitted to ICU faster from the onset of symptoms, compared to those who had a stronger immune response.
As a result of the findings, medics could test patients blood for antibodies and viral load to identify earlier who is most at risk of becoming seriously unwell or dying from the virus, the researchers said.
The findings could help personalise how Covid ICU patients are treated, including whether monoclonal antibody treatment should be used, they added.
The treatment, which was approved by Britain’s medical regulator in August, contains drugs casirivimab and imdevimab and is administered by injection or intravenously.
Costing £2,000 per patient, the brand new drug – made by US biotech firm Regeneron and Swiss company Roche – was found to slash the risk of death or hospitalisation by 70 per cent among patients with at least one risk factor for severe Covid.
It was the first treatment developed specifically to target Covid and be approved in the UK, after steroids and anti-inflammatories were repurposed to treat the virus.
The researchers noted that the blood samples were taken in the first wave, so their findings should be tested against patients hospitalised during subsequent waves.
And further studies are needed to confirm whether Covid antibodies block the virus from replicating, they said.
Dr Simon Clarke, a cellular microbiologist at the University of Reading, told MailOnline: ‘This is not a surprising finding, we already know that people who don’t mount a decent antibody response to Covid are more susceptible to the disease, it’s why some younger people are due to be given vaccine boosters in the UK.
‘But these findings do show us that there’s a greater correlation between disease severity and antibody levels, this might well be used by doctors to predict the course of someone’s disease and tailor their treatment accordingly.
‘It’s also a very useful reminder that merely having antibodies to the coronavirus does not automatically mean that we are protected from it, as some people assume.
‘We need enough of the right types of antibodies for that to happen.’
Source link : https://www.dailymail.co.uk/health/article-10060745/Covid-ICU-patients-low-antibody-levels-face-higher-risk-dying-study-confirms.html











