The Delta variant and changes in human behavior – such as the end of masking and social distancing – may explain why COVID-19 vaccines became less effective at protecting New Yorkers against infection, a new study from the state’s Department of Health (DOH) finds.
DOH scientists used statewide immunization, testing, and hospitalization datasets to examine vaccine effectiveness trends during New York’s Delta surge over summer 2021.
Results showed that efficacy against infection declined for the Pfizer-BioNTech, Moderna and Johnson & Johnson vaccines by as much as 25 percent.
Despite decreased effectiveness for infection, the study foun the vaccines remained highly protective against hospitalization with Covid – with effectiveness over 90 percent for adults ages 18 to 64 during the Delta surge.
Only New Yorkers over age 65 saw a slight decline in the vaccines’ protection against hospitalization over the summer – which the team says support the need for booster shots in older adults.
These data suggest that ‘ongoing waning protection may be less of a current concern for adults younger than 65 years,’ said DOH scientist Dr Eli Rosenberg.
New analysis from the New York Department of Health suggests that vaccines became less effective against COVID-19 infection this summer due to Delta and behavior changes, not waning immunity. Pictured: Vaccination at a church in the Bronx, New York, June 2021
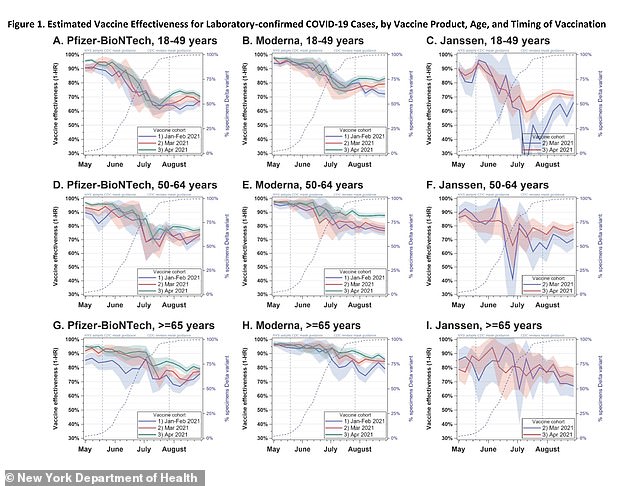
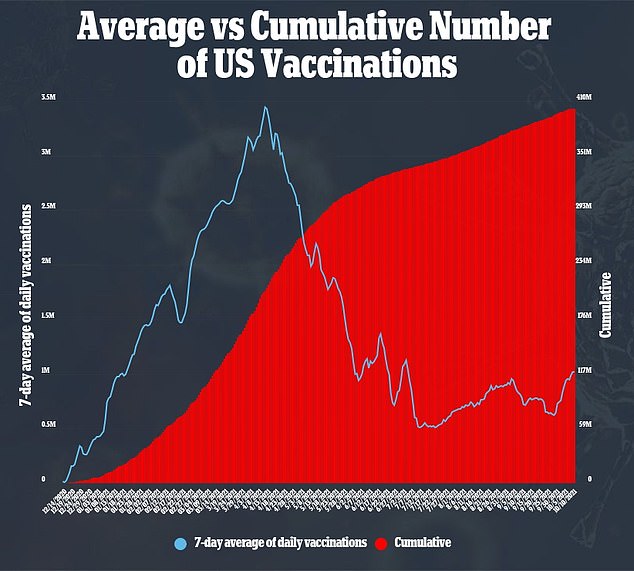
From May to August, the vaccines became less effective at protecting New Yorkers from a coronavirus infection, with the largest decrease seen for Pfizer vaccine recipients between ages 18 and 49 of about 25% (top left)
Booster shots have spurred endless confusion and debate in the U.S. in recent weeks.
The Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA) recently authorized booster shots of Pfizer’s vaccine for seniors and other Americans deemed at high risk for breakthrough Covid.
Later this week, the FDA’s advisory committee on vaccines will discuss similar booster shot authorizations for Moderna’s and Johnson & Johnson’s vaccines.
In part, these discussions are complicated because the U.S. has limited data available on how well the vaccines are working – and who is at most risk for a breakthrough case.
The CDC is not comprehensively tracking all breakthrough infections, focusing instead on severe cases and specific groups, such as healthcare workers.
As a result, many booster shot discussions have used data from Israel and the UK – two countries that are tracking breakthrough infections more closely. But these nations’ populations and vaccine rollouts are very different from the U.S.
A new study from the New York DOH helps to fill this data gap and suggests why the state saw a rise in breakthrough infections this summer.
The study – which is not yet peer reviewed – was posted online at the preprint server medRxiv on October 9.
‘This latest study conducted by our renowned scientists here at DOH is the largest to examine in-depth changes in vaccine effectiveness over time broken down by all three COVID-19 vaccines types currently authorized for use in the United States,’ said New York Health Commissioner Dr Howard Zucker, a senior author, in a statement.
‘It clearly demonstrates what we’ve been saying all along – getting a COVID-19 vaccine continues to be the best way out of this pandemic, and the best way for New Yorkers to prevent serious illness and hospitalization.
‘We urge all New Yorkers to remain vigilant and get vaccinated against COVID-19 if you have not already done so.’
The DOH scientists linked several statewide datasets with information on New Yorkers’ Covid vaccinations, test results, and hospitalizations in order to compare vaccine effectiveness over the course of 2021.

The new study demonstrates that ‘getting a COVID-19 vaccine continues to be the best way out of this pandemic,’ said NY Health Commissioner Dr Howard Zucker. Pictured: A resident of the Hebrew Home at Riverdale, New York receives his booster shot, September 2021
In addition, the researchers compared vaccine effectiveness by age, by which vaccine patients received, and by their vaccination timing.
Vaccination timing is particularly crucial in studies like this one, because some past research on Covid antibodies has suggested that vaccines could lose their effectiveness over time.
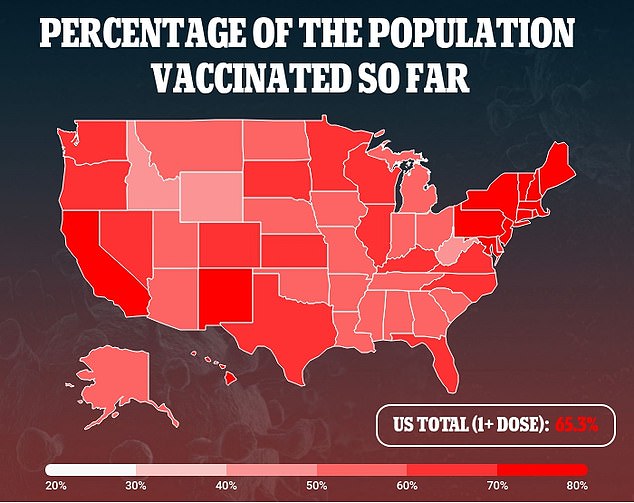
In total, the study included about 8.8 million adults living in New York – of whom about two-thirds were fully vaccinated.
The researchers focused their analysis between May 1 and August 28, 2021, during which the Delta variant went from accounting for two percent of cases in the state to 99 percent of cases.
Vaccine effectiveness against infection declined during the Delta surge – meaning fully vaccinated New Yorkers were more likely to have a positive Covid test during this time than they had been earlier in 2021.
For Pfizer vaccine recipients between the ages of 18 and 49, vaccine effectiveness against infection declined by 25 percent during the Delta surge.
Effectiveness declined by 19 percent for Pfizer recipients ages 50 to 64, and by 14 percent for Pfizer recipients over age 65.
Moderna vaccine recipients saw similar effectiveness declines: 18 percent decline for those ages 18 to 49, 14 percent decline for those ages 50 to 64, and nine percent decline for those over age 65.
J&J vaccine recipients also saw reduced protection from Covid infection: 19 percent decline for those ages 18 to 49, and 11 percent declines for those ages 50 to 64 and over 65.
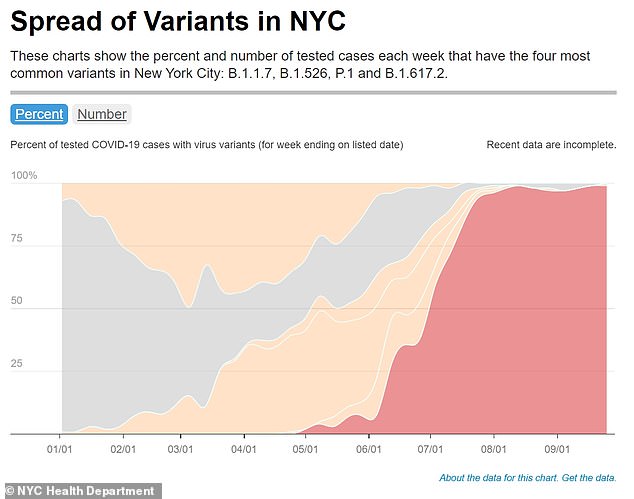
From May to August, the Delta variant (shown in red) completely dominated Covid cases in New York City and in the state overall. By the end of August, Delta caused 99 percent of cases
The researchers found similar declines in the vaccines’ protection against a Covid case, regardless of when they had their shots.
This finding suggests that the immune system was not facing ‘waning immunity’ from reduced antibodies, the team said.
Instead, the increase in breakthrough cases was ‘highly correlated’ with Delta’s takeover of the Covid landscape in New York state.
Once Delta fully dominated New York cases – at 85 percent prevalence – the researchers saw vaccine effectiveness plateau, further suggesting that this highly contagious variant was behind the drop.
In addition, the researchers suggested that changing Covid safety behaviors in New York may have contributed to an increase in breakthrough cases.
The study authors noted that New York followed CDC guidance early in the summer, telling fully vaccinated residents that they could go maskless in public locations.
At the same time, more New Yorkers took part in indoor dining, events, and other activities as the city reopened.

Despite decreasing vaccine effectiveness against Covid infection, all three vaccines remained very protective against hospitalization – with effectiveness over 90% for most groups (above)
Despite decreasing vaccine effectiveness against infection, all three vaccines remained very protective against severe disease and hospitalization, the DOH study found.
For younger adults (ages 18 to 64), the vaccines were at least 90 percent effective against hospitalization throughout the Delta surge, with no significant declines over time.
Only New Yorkers over age 65 saw slight declines in the vaccines’ ability to protect against hospitalization during the Delta surge.
For seniors who’d received the Pfizer vaccine, effectiveness against hospitalization dropped from 95 percent to 89 percent.
For those who received the Moderna vaccine, effectiveness dropped from 97 percent to 94 percent.
‘The findings of our study support the need for boosters in older people in particular, and we encourage them to seek out a booster shot from their health care provider, pharmacy or mass vaccination site,’ said DOH scientist and lead author Dr Eli Rosenberg.
‘We saw limited evidence of decline in effectiveness against severe disease for people ages 18 to 64 years old.
‘While we did observe early declines in effectiveness against infections for this age group, this appears to have leveled off when the Delta variant became the predominant strain in New York.
‘Together, this suggests that ongoing waning protection may be less of a current concern for adults younger than 65 years.’
Source link : https://www.dailymail.co.uk/health/article-10084527/Delta-variant-behavior-caused-vaccine-efficacy-drop-summer-New-York-DOH-study-finds.html











