Faced with a 12 to 18-month wait for a hip replacement on the NHS, housewife Barbara Price decided to do something she had never done before — she went private.
After the 85-year-old’s left hip suddenly ‘went’ due to wear-and-tear arthritis in June last year, she was housebound and unable to get up to make a cup of tea.
Barbara could no longer do any cleaning, washing, cooking, gardening or shopping, and the stairs were impossible to climb, so she lived downstairs and relied on the help of her son Karl, 58.
In agonising pain that even prescribed painkillers could not touch, earlier this year Barbara spent £14,000 of her life savings to have the operation privately.
‘We felt we had no alternative,’ says her daughter Loraine, 54, from Coventry, a full-time carer for her husband.

A recent survey it conducted with 1,750 UK adults revealed that 51 per cent were now more likely to consider private healthcare given the growing NHS waiting lists [File photo]
‘Mum was in so much pain, she struggled to sleep — which left her exhausted the next day. She couldn’t manage and it was really making her feel low.
‘Her NHS appointments and scans were delayed for months because of Covid and there was nothing we could do, so we decided we’d pay to have the operation done privately.’ Within two days of contacting the private hospital, Barbara saw a consultant and two months later, she had the operation.
‘She can now walk around the garden and there is a sparkle in her eyes again,’ says Loraine.
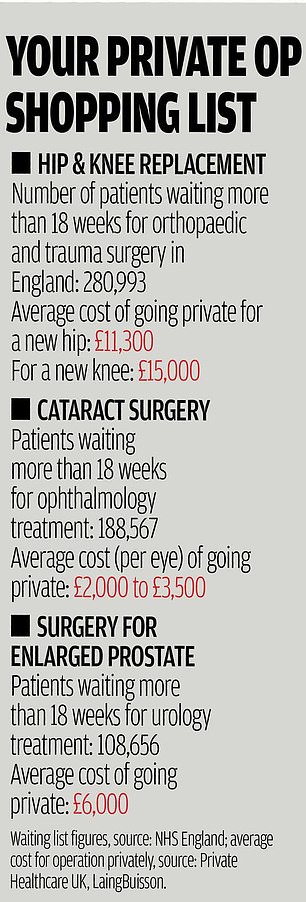
With NHS waiting lists for hospital treatment in England now topping 5.3 million, the highest on record, and estimates that they could hit ten million — as patients who have been reluctant to seek medical help during the pandemic come forward — increasing numbers of people are, like Barbara, deciding to pay rather than delay their treatment.
Since the end of the first wave of the pandemic, Spire Healthcare, which has 39 private hospitals across the UK, says it has seen ‘a significant rise’ in enquiries from those who want to pay for treatment.
A recent survey it conducted with 1,750 UK adults revealed that 51 per cent were now more likely to consider private healthcare given the growing NHS waiting lists.
HCA Healthcare UK, which has eight private hospitals in England, has carried out double the number of self-pay hip, cataract and abdominal operations compared with the previous year; and 30 per cent more gynaecological procedures.
Meanwhile, the number of people buying private medical insurance for the first time has doubled in the UK since the start of the pandemic, according to the price comparison website ActiveQuote.
Brian WALTERS, managing director of health insurance broker Regency Health in Cheltenham, says it is witnessing ‘a spike in demand’. Yet it doesn’t come cheap.
Even for the most basic package, which includes a £500 excess, private health insurance costs between £40 and £70 a month for someone who is 55, doesn’t smoke and lives in Tunbridge Wells.
And many policies have multiple caveats, such as not including pre-existing medical conditions.
From the start of the first lockdown to March this year, private hospitals were locked into special agreements with the NHS to provide extra beds and treatments for those needing essential care.
However, two thirds of the private sector capacity that was block-purchased by the NHS went unused last summer, according to a Health Service Journal report, with poor communication and confusion in the NHS about how to use the private sector blamed.
If more people choose to go private, there are concerns that the NHS will suffer, because an increase in private work might encourage doctors who work in the NHS to ditch their jobs and instead work only privately.
‘More people choosing to go private will not in itself help ease pressure on the NHS as it is the same consultants and clinicians that will find themselves under greater demand from both private and NHS patients,’ says Nigel Edwards, chief executive of health think tank The Nuffield Trust.
‘This could, in fact, distort the market which, if the demand is there, could see urgently needed doctors opting to work solely privately.’
Consultants’ contracts state that private work must ‘not result in a detrimental effect on NHS patients or services, nor diminish the public resources that are available for the NHS,’ according to the British Medical Association.
Nigel Edwards says it’s ‘unsurprising’ that more people are seeking private medical care as ‘the pandemic continues to heap pressure onto the NHS.
‘There have been around four million referrals from GPs that haven’t taken place, massive cuts in planned surgery and the prospect of several years of longer waits as the service tries to recover against a spiralling backlog.’
Tracey Loftis, head of policy and public affairs at the charity Versus Arthritis, agrees, adding: ‘Thousands of people with arthritis are having to endure long waits for joint replacement surgery because of the backlog, which existed anyway but has been made worse by the pandemic.
‘We’re hearing from people who are turning to private treatment, often as a last resort, and requiring financial support from family, so they’re no longer in constant pain.’
The galling thing is that when people go private, they often end up having the same surgeon they would have had on the NHS.
So by paying you may get seen quicker, but you won’t necessarily be getting a different standard.
This was the case for Paul Nelson, 80, from Poole, Dorset, who recently paid more than £8,000 for spinal surgery at the private Spire hospital in Southampton.
The ex-serviceman had been told he’d have to wait 12 to 18 months for NHS surgery to correct a disc problem that was causing terrible lower back pain.
But going privately, he waited just two months from diagnosis last October to having the operation (and this included a one-month delay because his surgeon tested positive for Covid). ‘If you can afford it, why would you wait for an operation?’ he says.
The same consultant who was treating me on the NHS was able to do it privately in December and did a marvellous job.
‘I was discharged from hospital after two days and after six weeks I was back to normal. I hope to be playing golf again soon.’
Private hospitals have been treating NHS patients for the past 20 years — and in considerable numbers: in a typical year, they will perform around 500,000 operations (including joint replacements) for the NHS, according to the Independent Healthcare Providers Network (IHPN).
Special agreements with the health service during the pandemic meant many more NHS patients received their care in the private sector.
Since the end of last March, over 3.2 million NHS operations, scans and tests, consultations and chemotherapy sessions have been delivered by independent hospitals (over 100,000 were cancer treatments).
Those deals ended in March this year.
So far, the rise in the number of people taking out private medical insurance or choosing to self-pay has not translated into an overall rise in private patients as the private sector has also lost some of its usual patients, such as overseas patients, who normally make up between a quarter and a third of patients in private hospitals in London.
But private hospitals are now bracing for an increase in demand as NHS waiting lists increase. David Hare, the head of the IHPN, played down fears that NHS surgeons may take on more private work to the detriment of NHS patients.
‘The time commitment that doctors make to the NHS must be honoured,’ he told Good Health. ‘However, outside these hours, they are free to work in the private sector if they want.’
Source link : https://www.dailymail.co.uk/health/article-9828177/Forced-pay-thousands-surgery-Waiting-lists-mean-theres-one-option.html











