Continuing our landmark series of pullouts to mark the 30th anniversary of the indispensable Good Health section, here are more inspiring stories, practical advice and medical breakthroughs taken from our archives.
Today, we look at a disease — cancer — where these advances have had a major impact, slashing death rates. There is much for cancer patients and their families to be hopeful about.
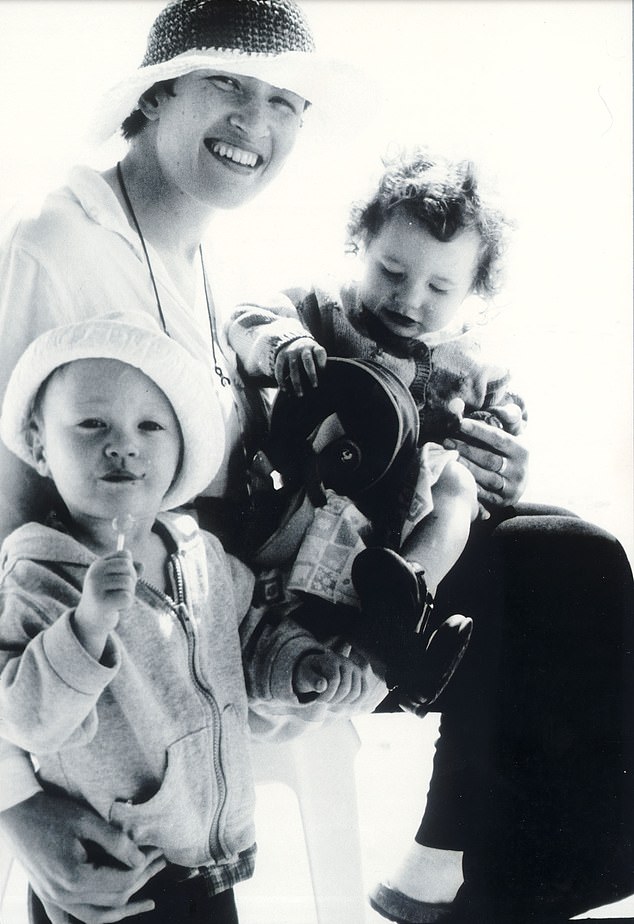
But for too many, there is heartbreak — highlighted in this moving interview with Gary Lineker from 2005, where the TV sports presenter spoke about his support for a hospice for desperately-ill children, and the agony of watching his own son, George, then a baby, undergo gruelling — but ultimately successful — treatment for leukaemia …
December 20, 2005
When Gary Lineker turned up to open a new playroom at the Kent hospice [Demelza House], there was a subdued atmosphere in the normally bustling living areas.
‘They’d lost two children that day,’ he recalls. ‘It was hard to get away from that. The other kids were delighted to be getting a new facility, but there was a note of sobriety about the whole event. It brought it home to me what an amazing job these people actually do, in circumstances most of us would consider impossible.’
Like most celebrities Lineker, a former England captain turned sports TV presenter, gets his fair share of requests from charities. But when he was asked to become involved with Demelza House, which the Mail chose to be the beneficiary of its annual Christmas appeal [back in 2005], he didn’t hesitate to say yes.

In a moving interview with Gary Lineker from 2005, he speaks about the agony of watching his own son, George, (pictured together) then a baby, undergo gruelling, but ultimately successful, treatment for leukaemia
And there was a deeply personal reason why the father of four wanted to lend his support to the charity.
Thirteen years ago, Lineker discovered just how difficult it can be for a family to cope alone in the face of a child’s critical illness. His eldest son, George, was diagnosed with leukaemia when he was just a baby.
Lineker and his then wife, Michelle, spent much of George’s early life at his bedside in Great Ormond Street Hospital for Children, in London, where tiny George underwent chemotherapy.
Although the treatment appeared to be successful immediately, George did not get the all-clear until he was five. Memories of those painful days are clearly never far from Lineker’s mind.
A MAGIC PILL TO SWALLOW
March 6, 2001
A revolutionary device that is so small it can fit in a pill could stop thousands developing bowel cancer. Nicknamed the Magic Pill, it is actually a digital camera hidden in a capsule the size of an aspirin.
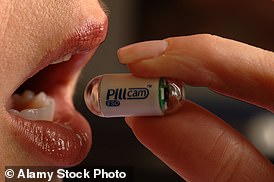
TODAY’S UPDATE: The gadget was developed into a device called PillCam, now widely used worldwide (pictured)
After being swallowed by a patient, it begins its voyage through the intestinal tract, snapping perfect colour images every five seconds. Until now, examining the central part of the small intestine with an endoscopy or colonoscopy has been almost impossible, making it difficult to detect warning signs of cancer.
Dr Paul Swain, one of the UK’s leading gastroenterologists, was the first person in the world to swallow a Magic Pill, just over a year ago. Since then, 50 patients have used it worldwide, including nine in the UK.
TODAY’S UPDATE: The gadget was developed into a device called PillCam, now widely used worldwide. Earlier this year, the NHS launched a pilot scheme with pills based on similar technology, which have been sent out to 11,000 patients to carry out at-home checks. As well as aiding early diagnosis of bowel cancer, it’s hoped this could tackle the backlog in colonoscopies due to the pandemic.
Advertisement
‘When I come to a place like Demelza and see families who are so anxious, it does all come flooding back,’ he explains.
‘No family who has ever had to sit by a child’s bedside, racked with worry, will ever forget how awful it feels. But there was a big difference with us.
‘When George was ill, we always had hope that he would get better, and we clung to that hope. I think being positive was the only way we could have got through it. The families here, though, have had to face the worst. Most have had to accept that their children will never get better. Some are right at the end.’ He shudders. ‘The strength of character you see in a place like this really is humbling.
‘I honestly don’t know how some families do it — but places like this really do seem to help them cope with the impossible.’ When he visits Demelza House — where he spends time talking to the parents, or kicking a football about with the youngsters — Lineker does not talk about his own family, save to say that he understands, to a point, what they are going through.
‘It’s very different,’ he explains. ‘I never make a big deal about what happened to us, but most people know that we’ve had experience with a very ill child, and they seem to appreciate that.
‘But I wouldn’t say for one minute that I understand what they are going through because I don’t. You can’t unless you have to go down that route.’
With each visit, however, he returns home — to his own four boisterous sons — reminded of his own good fortune.
Perhaps this is why Lineker has long immersed himself in the fundraising arena.
As well as supporting Demelza House, he is a tireless campaigner for Great Ormond Street.
He also supports leukaemia charities, and was a high-profile campaigner for donor cards.
‘Part of me would like to forget about what we went through, but I just can’t do that, and putting a little back is perhaps our way of saying thank you, and perhaps helping other people in the process,’ he says.
IVF fears over breast cancer
The death in 2003 of Paul Merton’s wife Sarah Parkinson once again brought IVF treatment into the spotlight — for all the wrong reasons. Learning she had breast cancer after finishing fertility treatment, Sarah, 41, was convinced it was triggered by the IVF treatment.
So what is the truth? Here, JUSTINE PICARDIE, whose sister Ruth conceived twins through IVF and later died of breast cancer, gave her very personal reasons for suspecting there may be a darker side to fertility treatment…
September 30, 2003
Last week, I was interviewed on the radio about an anthology of short stories to which I’d contributed — A Day In The Life, which is being sold in aid of Breast Cancer Care — and the presenter asked me a difficult question. ‘Do we really need to know anything else about breast cancer?’
I gave the usual grim statistics: that one in nine women in this country develops breast cancer; that it’s the most common form of female cancer; that nearly 40,000 women are diagnosed every year, and the incidence is rising.
But afterwards I realised that what I should have said is we still don’t know very much about breast cancer at all.
Adored: Ruth Picardie (pictured) had twins through IVF and later died of breast cancer aged 33
I was still thinking about this several hours after the interview when I was told that Sarah Parkinson — who’d also contributed a story — had just died of breast cancer at the age of 41, someone who’d eaten sensibly, done yoga, and was irrepressibly happy.
And just like Sarah, my sister Ruth — who died of it at 33 — seemed equally glowing with vitality. What, then, had made them so unfortunate? Was it just bad luck? Or was it that Ruth and Sarah had both undergone IVF?
Sarah, certainly, had no doubt that the fertility treatment had been a factor in her development of the disease. She’d felt a swelling in her breast before she commenced IVF two years ago. But after a mammogram and ultrasound, Sarah had been told not to worry about it.
Yet her cancer was diagnosed just a few months later, in February 2002, and it was sufficiently advanced — and aggressive — to have spread to her lymph nodes.
RED FLAG
Women often have one slightly larger breast, but a change in size or shape of one or both breasts should be checked by your GP.
Advertisement
Similarly, one of the first questions my sister had asked when her cancer was diagnosed was: ‘Could it have been caused by the IVF?’ (Her longed-for and much-loved twins were conceived after one cycle of IVF, a year before her diagnosis.) Her doctors gave her varying answers: from no, to maybe (but the maybe was always strictly off the record).
Yet as both Ruth and Sarah pointed out, given that the Pill and HRT have been associated with breast cancer, then why not IVF?
All of them involve doses of female hormones, and while we don’t yet know the exact effect that they have on breast cancer, we do know they can be linked, in myriad ways.
After Ruth’s death, I helped to set up the Lavender Trust, which provides support and services for younger women with breast cancer. I’ve lost count of the times I’ve heard anecdotal evidence about a link between IVF and cancer.
Of course, not all women who have IVF get breast cancer, and I’d hate to create unnecessary alarm. Certainly, there is no conclusive medical research. I’m aware, too, that the rage I feel about their deaths may cloud my judgment. But that doesn’t stop me feeling angry that Ruth’s and Sarah’s questions are still unanswered.
So now, if anybody asks me about it, I’ll say I’m not an expert but I’d always advise women to ask doctors plenty of questions, talk to relatives about any strong family history of cancer, and speak to the Lavender Trust (breastcancernow.org).
TODAY’S ADVICE: A major review looking at data from 1.8 million women undergoing fertility drug treatments has found ‘no significant increase’ in their risk of developing breast cancer compared to women who hadn’t taken the drugs. The review, by King’s College London, is the largest study to date assessing fertility drugs as a potential cancer risk.
Don’t die of embarrassment
For many years the Mail has been a vociferous campaigner for men affected by prostate cancer…
November 2, 1999
Every hour at least one British man will die from prostate cancer. Yet last year a derisory £47,000 was spent searching for a cure. Today the Mail launches a campaign to raise £1 million to research this taboo disease. It’s a series all men — and the women who love them — must read . . .
What’s more, every pound donated by Mail readers — up to £500,000 — will be matched by the Southon Charitable Trust, whose founder Arthur Southon died of prostate cancer. For too long, prostate cancer has been the disease no one will talk about, least of all our politicians.
For too long it has been greeted with giggles, embarrassment or a shocked silence. Masculinity, virility, the very essence of what it was to be a man, was somehow challenged by prostate cancer.
HEALTH HACK
Men should consider adding a scoop of nuts to their breakfast, suggests urologist Dr Neil Haldar.
They’re rich in tocopherols, compounds thought to combat cancer.
Advertisement
‘Real men’ have been reluctant to admit that anything could be wrong with their private parts, and they certainly never bother to get themselves examined. Much the same was once true of breast cancer.
For a woman to admit that her breast was diseased and might have to be operated on, or even removed, was to question — if only at a subconscious level — her beauty and desirability.
But things have changed for women. Today, we spend almost 100 times as much on breast cancer as we do on studying and treating cancer of the prostate.
There are well-organised and high-profile breast screening programmes and national breast cancer awareness weeks.
But the number of men who die from prostate cancer is rising. The number of deaths in Britain from prostate cancer has doubled since the late 1970s to 10,000 a year, and the figure is still growing.
Best-selling author Jeffrey Archer spoke to Good Health in 2018 about his diagnosis with prostate cancer, urging readers to be more vigilant than he was …
February 27, 2018
Five years since I had my operation for prostate cancer, and I have never felt better. However, it’s possible that’s only because my wife insisted on me seeing a specialist when I told her my PSA score was 6.8.
Frankly, at the time, I didn’t know what PSA stood for, let alone the significance of mine being 6.8.
During my annual check-up with my GP, among other things I always have a blood test, and in 2014 when the results came back from the lab, Dr Page wrote to tell me that my PSA level was slightly on the high side.
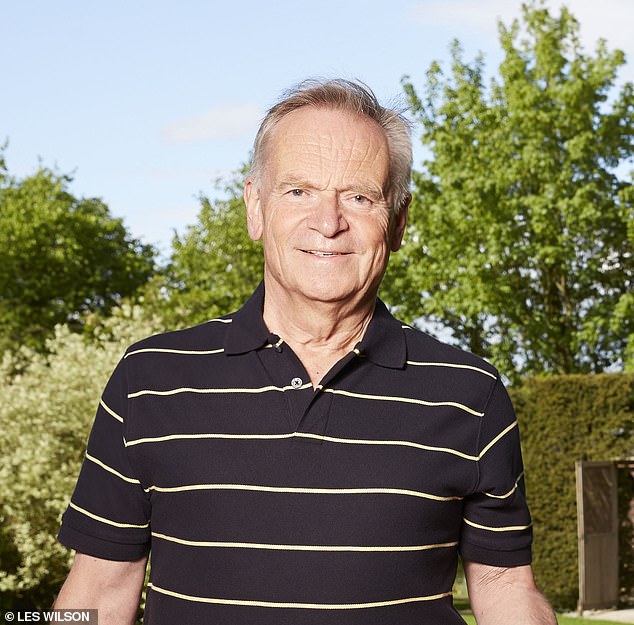
Lord Jeffrey Archer (pictured) spoke to Good Health in 2018 about his diagnosis with prostate cancer, urging readers to be more vigilant than he was
‘What does PSA stand for?’ I asked when I called him, ‘and how bad is 6.8?’
‘PSA stands for prostate-specific antigen,’ he replied, explaining that it’s a protein produced by the prostate gland and raised levels can be a sign of prostate cancer.
‘And 6.8 is fairly normal for someone of your age [then 73], but it’s heading in the wrong direction, so perhaps you should see a specialist.’
As Mary and I live in Cambridge, Dr Page made an appointment for me to see Nimish Shah, the clinical director of urology at Addenbrooke’s Hospital.
The first thing Mr Shah wanted to do was take another blood test so that he could double-check my PSA level. Same result — 6.8.
‘We should conduct an image-guided biopsy,’ announced Mr Shah, ‘and have a proper look at your prostate.’
Under local anaesthetic, several tissue samples were taken from my prostate — not very pleasant — but the results confirmed that I did have prostate cancer. Mr Shah told me I had three choices. The first, active surveillance, which would involve regular checks, but no treatment.
Mr Shah then produced a chart showing that I had a 90 per cent chance of dying from something other than prostate cancer during the next 15 years, which sounded pretty good to me. After all, 88 is not too bad an age to finally report to the Almighty.
But Mary pointed to a 37 per cent risk of mortality from my particular cancer if I did nothing, so I had no choice but to listen to what else Mr Shah had to offer.
Plan B was to have an operation to remove the whole prostate, and plan C — commence hormone therapy to shrink the tumour, followed by a seven-week course of radiotherapy.
The other major factor to consider is the effect it may have on your sex life. If you have the operation, you will no longer produce sperm.
However, with the help of Viagra, you can still experience the same sensation. But if you still want children, you will have to opt for radiotherapy (not a problem I had to consider).
When Mr Shah told me that my procedure would be performed by a robot — known as the da Vinci — I was initially a little sceptical, but recalled from my schooldays that da Vinci was well ahead of any of his rivals, not just as an artist, but as a scientist.
I was booked in for surgery soon afterwards. Did I spend the next few weeks becoming anxious, fearful, even paranoid? Certainly not. After all, I had witnessed my wife going through a far more demanding and experience, when she’d had a cancerous bladder removed a few years before, without a murmur. So I was not going to make a fuss, even if I wanted to.
On December 18, 2013, I checked in to Addenbrooke’s with an overnight bag at 7am as instructed.
Once I had fully recovered, I never had any problem with discussing the operation with friends and fellow sufferers, most of whom were fascinated by what I’d been through.
However, there was one remarkably stupid man from my rugby club, who felt he was far too macho to bother with being tested. It’s common sense to find out whether you are at risk. I have asked several of my friends in the past five years whether they knew their PSA and with one exception, none of them had a clue.
If we are to reduce the number of deaths through prostate cancer, as the Mail’s campaign is calling for, we must start by encouraging more men to get tested.
I hope any men over the age of 50 reading this article — and especially black men, who are more susceptible to prostate cancer than white men — will be sensible enough to do as Prostate Cancer UK recommends.
After all you might be like me, and not have any prostate symptoms, yet have cancer. So visit your GP, have a blood test, and find out what your PSA is. It may save your life.
■ The fee for this article has been donated to Prostate Cancer UK.
Health hero who made young patients smile again
In 2014, then Prime Minister David Cameron launched the annual Daily Mail Health Hero Awards, our hunt for the unsung health workers who go the extra mile. We met the inspirational woman who helped young cancer patients smile again. Bianca Effemey has devoted her life to helping sick children, as AMANDA CABLE reported…
April 22, 2014
Halfway into his chemotherapy for testicular cancer, 15-year-old Ed Scott fell into a deep depression. The fight seemed to have gone from him, recalls his mother Jo.
‘It was just awful to see him so low,’ says Jo.
‘He’d always been so brave and upbeat, but he was terribly sick from the chemo, he’d had a testicle removed, lost his hair, and while his friends were dating and going to parties, Ed felt really down.
‘He was too exhausted and too nauseous even to watch TV. He just lay in his hospital bed in dark despair.
‘I understood totally — but I felt utterly helpless.
‘The doctors were worried about his despondency, too. They said he needed all the fight he had to cope with the chemotherapy.
‘But Ed told me he just wanted to rip out his drips and walk out of the door.’ Jo herself was under unbearable strain.
The overwhelming anxiety about her son, compounded by a house move and trying to maintain a normal life for two daughters at home, aged 13 and five, meant she and husband Tom spent shifts in the hospital, passing only in their cars.
Late one night, she picked up the phone and rang Bianca Effemey.
A former hospital receptionist, Bianca often works with as many as 200 families at a time.
Much of that support is practical: thanks to her relentless fundraising she’s collected enough money for a holiday home in Hampshire where families can take vital breaks, as well as paying for days out.
But perhaps more important is the emotional support. For while at night she runs her charity, by day she works at Kingston Hospital as a parent supporter.
She contacts every family who arrives at the paediatric unit at the hospital with their newly diagnosed child, giving out her number for them to call day or night.
‘When I rang Bianca, I told her how worried I was about Ed, and how the nurses and doctors were very concerned, too,’ says Jo.
‘The next day, she turned up and talked to him.’
Jo added: ‘Bianca stepped in to provide unstinting support during the lowest moments for all of us.
‘She was the one person who saw behind the forced smile painted across my face.’
The fight never stops to find out why we lose so many loved ones to cancer
Kylie Minogue’s diagnosis of breast cancer at just 36, and more recently the tragic death of Sarah Harding from the disease at the age of 39, have highlighted a growing toll on younger women, and what might be driving it…
May 31, 2005
When Kylie Minogue announced she had breast cancer two weeks ago, the news was particularly shocking because of her age. At just 36 and the picture of health, she seemed terribly unlucky to have an illness that normally hits women over 50.
But Kylie’s case is not an aberration. Figures revealed last week showed that the number of under-40s with breast cancer has increased by more than 50 per cent in just one generation.
Of the 41,000 women diagnosed with the disease in this country each year, 2,200 are in their 20s and 30s. Although still a minority, it is a sizeable one and, when compared with figures for 1975 — when 1,266 under-40s were diagnosed — it raises questions as to why modern women seem to be at a greater risk of breast cancer than their mothers were.

When Kylie Minogue (pictured) announced she had breast cancer two weeks ago [in 2005], the news was particularly shocking because of her age. At just 36 and the picture of health, she seemed terribly unlucky to have an illness that normally hits women over 50
Hisham Hamed, a consultant breast surgeon at Guy’s Hospital and Cancer Research UK, says the statistics cannot be explained simply by an increased awareness of the disease.
He says: ‘That means more young women will come to a clinic and be checked earlier, so their chances of survival are much better — but it does not increase the number of young women getting breast cancer.’
‘In older women, however, screening has meant that we are now detecting cancers before they are visible: cancers that might not have been diagnosed 30 years ago.’ For many years, it seemed those most at risk of contracting the disease under 50 had a family history of it. But statistics show that only 5 to 10 per cent of such cases are likely to be caused by a hereditary link.
Mr Hamed says: ‘I have had patients as young as 18. I treated one woman who was 21 and died at 23, and this week I have seen a 28-year-old with breast cancer who is 24 weeks pregnant. None had a family history of the disease.’
He says that, although it is impossible to make definite causal links between lifestyle and breast cancer, women may now be ‘paying the price for our modern life’. He cites the ‘style of life, oral contraception, alcohol consumption and delaying pregnancy’ as factors that could be increasing young women’s risk of the disease. Carcinogens and toxins in the environment may also play a part.
breastcancernow.org
FIGHT TO STOP TEENAGE CANCER
June 26, 2018
In this hard-hitting report, CAROLINE SCOTT examined why cancer drugs used for adults are not used to treat teen cancers as families questioned whether pharmaceutical companies are to blame for not allowing young people to take part in new trials.
When Debbie Binner’s sporty 14-year-old daughter, Chloe, complained of pains in her right leg, she thought the problem might be muscular.
The family GP believed it could be a torn muscle, says Debbie, 52, a journalist and author. But when, a couple of months later, Chloe started to limp, the GP referred her to Epsom Hospital in Surrey for an MRI scan. Not for a moment did Debbie think her dance-mad teenager might have cancer.
‘After Chloe had her scan, the surgeon explained that Chloe had a tumour in her pelvis, and that the cancer had spread to her lungs,’ says Debbie. ‘He made it very clear that she might not live.’
Chloe’s diagnosis was the start of an ordeal which revealed the lack of treatments for children with cancer, and culminated in her dying before she was eligible to try a drug which might have given her more time.
HEALTH HACK
Swap regular broccoli for tenderstem — it can contain up to 45 per cent more glucosinolates, compounds shown in lab studies to trigger cancerous cells to self-destruct.
Advertisement
Chloe had Ewing sarcoma, a rare bone cancer which mainly affects children and young people. The cancer was so advanced at diagnosis that Chloe had a 20 per cent chance of survival. ‘She never once broke down or asked: ‘Why me?’ says Debbie. ‘We held on to hope. I was determined to find out everything about her disease and make sure Chloe was one of the 20 per cent.’
But Debbie discovered there had been no new treatments for Ewing sarcoma for 40 years. When Chloe’s tumours stopped responding to chemotherapy, Debbie discovered a clinical trial of a drug called talazoparib, which stops damaged cells from repairing themselves.
It was being trialled for cancers with similar genetic alterations, including Ewing sarcoma. Debbie contacted the Institute of Cancer Research to enrol Chloe on the trial. But as the lower age limit was 18, and Chloe was then 17, she was not allowed to take part.
Chloe was accepted on the trial when she turned 18, but was too ill to benefit. She died two weeks after her 18th birthday.
Cancer doctors say nowhere near enough cancer medicines are being trialled or licensed for use in children. According to Accelerate, a platform that aims to improve early access to drugs, fewer than 10 per cent of children in relapse with a terminal cancer have access to experimental drugs.
Dr Lynley Marshall, a consultant in paediatric and adolescent oncology drug development at the Royal Marsden, says: ‘There is nothing in the regulations to say a young person can’t be included, but historically, that’s just the way the boundaries have been set.’
Source link : https://www.dailymail.co.uk/health/article-10043545/Heres-good-health-Gary-Lineker-proud-support-haven-hope.html











