The highly transmissible Delta variant made up nearly all cases in Southern California by mid-summer, with some groups at higher risk of infection than others, a new report finds.
Researchers from the Centers for Disease Control and Prevention (CDC) found that the variant accounted for 95 percent of Covid cases that underwent genome sequencing at Kaiser Permanente Southern California (KPSC) as of July 21.
Hispanic Americans and adults under age 45 were the most likely to be confirmed to have Delta.
What’s more, the report found that unvaccinated patients infected with Delta were almost twice as likely to be hospitalized as fully vaccinated patients who had breakthrough infections.
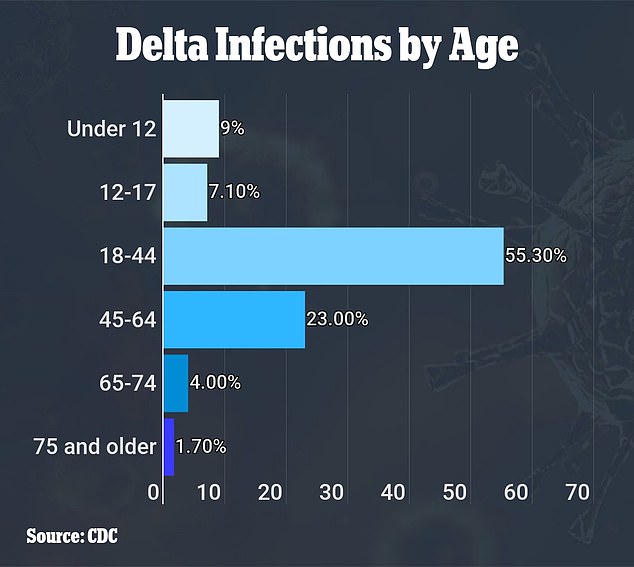
A new CDC report from Kaiser Permanente Southern California found that adults between ages 18 and 44 accounted for more than half of positive Delta specimens at 55.3%
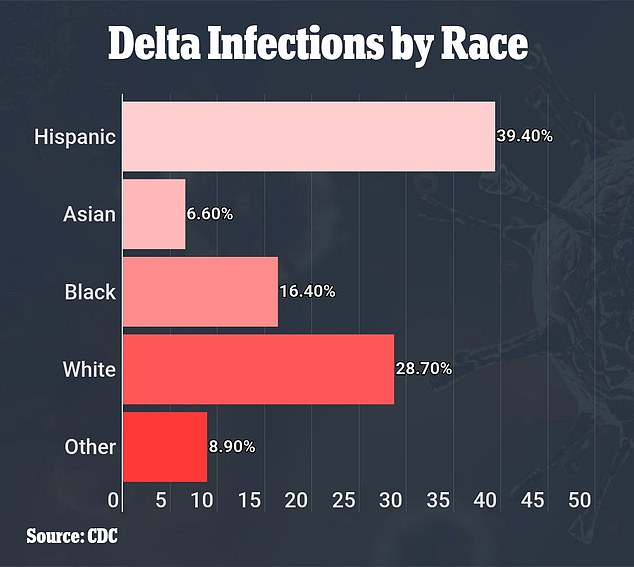
Hispanics were the most likely race/ethnicity to be confirmed with Delta, accounting for 39.4% of all infections
Known as B.1.617.2, the Delta variant first originated in India and was labeled a ‘double mutant’ by the country’s Health Ministry because it carries two mutations: L452R and E484Q.
L452R is the same mutation seen with the California homegrown variant and E484Q is similar to the mutation seen with the Beta and Gamma variants.
Both of the mutations occur on key parts of the virus that allows it to enter and infect human cells.
The Delta variant is twice as contagious as previous variants, and some studies have suggested it can cause more severe illness in unvaccinated people compared to earlier strains.
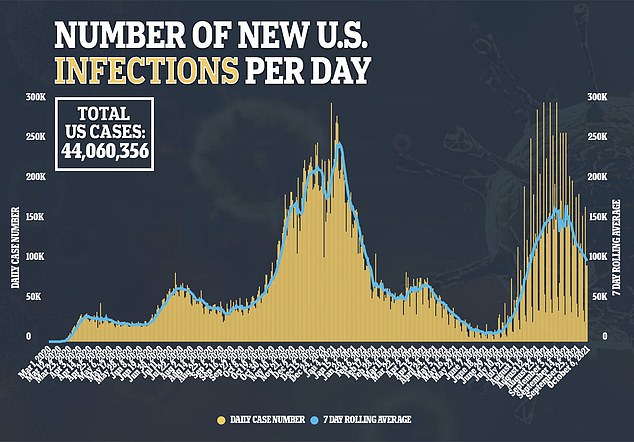
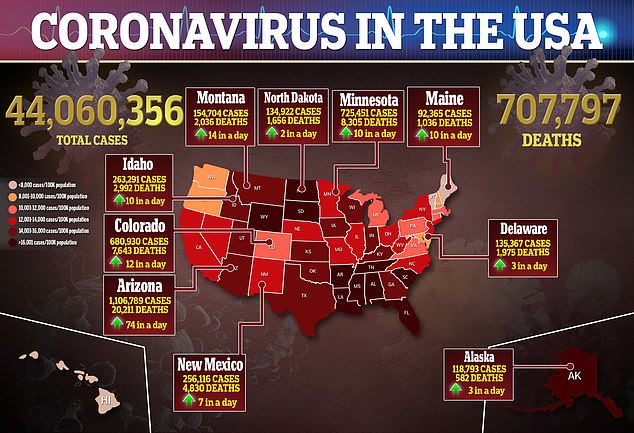
The CDC says that Delta and its sub-lineages are currently responsible for 99.5 percent of all new infections in the U.S.
However, there is little research detailing the demographic breakdown of those infected by variant, including Delta.
For the new report, published on Thursday, the team looked at data from patients at KPSC.
Researchers sequenced data from 6,798 specimens positive for COVID-19 between March 4 and July 21.
Of the positive samples, 88 percent came from unvaccinated patients, 10 percent from fully vaccinated patients and two percent from those partially vaccinated.
At first, the Alpha, which originated in the UK, variant made up the most cases, increasing from 20 percent in early March to 67 percent by May 19.
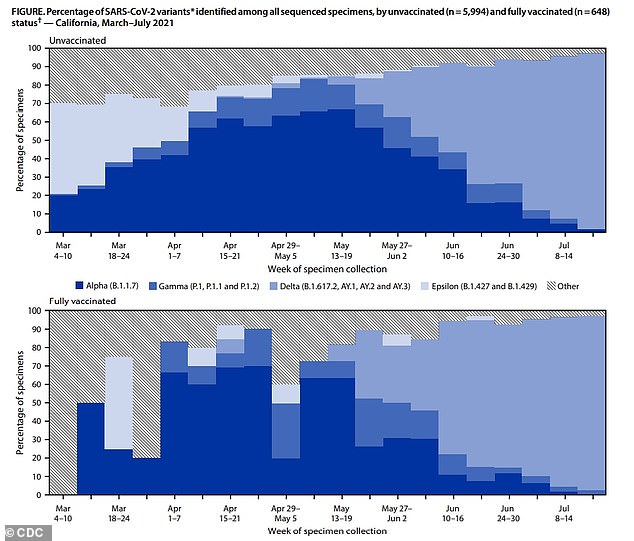
The Alpha variant made up the majority of cases from March to May, increasing from 20% to 67%, before the Delta variant took over, making up 95% of all cases
However, the Delta variant soon took over and, by July 21, it made up 95 percent of all samples that underwent sequencing.
Researchers found that certain age groups were at much higher risk of contracting Delta.
Of the specimens that were positive for the variant, more than half – 55.3 percent – were among those aged 18 to 44.
‘Similar to previous reports, persons with infections attributed to the Delta variant were younger, relative to all persons with positive sequenced specimens,’ the authors wrote.
‘This could be due to multiple factors, including increasing vaccination coverage among older adults and increased social interactions among younger adults during periods when the Delta variant predominated.’
There were also large differences when it came race and ethnicity.
Hispanic Americans made up the plurality of Delta specimens at 39.4 percent while white patients made up the second-highest amount at 28.7 percent.
‘Similarly, the observed differences in prevalence of Delta variant infections across race/ethnicity categories might reflect differences in risk for COVID-19 exposure among these persons during periods of high Delta variant transmission,’ the authors wrote.
The researchers also compared outcomes for patients infected with Delta by vaccination status.
Unvaccinated patients were 1.7 times as likely as those fully vaccinated to be admitted to the hospital at 6.6 percent compared to 3.9 percent.
‘These findings reinforce the importance of continued monitoring of SARS-CoV-2 variants and implementing multicomponent COVID-19 prevention strategies, particularly during the current period in which Delta is the predominant circulating variant in the United States,’ the team wrote.
‘Such preventive strategies include increasing COVID-19 vaccination coverage among eligible populations in coordination with other strategies such as universal masking and physical distancing.’
Source link : https://www.dailymail.co.uk/health/article-10069553/Hispanic-Americans-younger-adults-likely-test-positive-Delta-variant.html











