Family doctors must carry out more appointments face to face, the Daily Mail demands today.
A string of deaths has heightened fears that cancers and other illnesses are being missed because of the rise of phone and video consultations.
Before the pandemic around 80 per cent of GP appointments were in person. But the figure was just 57 per cent in July despite life returning to normal.
In some regions, just 45 per cent of consultations are face to face – even though most adults are now double jabbed. A senior coroner warned this month that not seeing a doctor in person may have contributed to the deaths of five people across Manchester.
The Daily Mail’s campaign for more face-to-face consultations was backed last night by politicians, charities and families.
Lisa King, who lost her husband Peter after a GP denied him an in-person appointment, said: ‘I hope this Daily Mail campaign can make a difference because I never want another wife, husband, son or daughter to have to go through what me and my two sons are going through.’
Arun Ghosh, 42, a GP partner in Liverpool, says virtual consultations are no replacement for a ‘hand on the tummy or listening to someone’s breathing’.
In today’s Mail he writes: ‘Many GPs, especially locum and salaried doctors, who are not partners in a GP surgery, now prefer remote appointments.’
Health and Social Care Secretary Sajid Javid last night welcomed the Mail’s move.
He said: ‘I am committed to ensuring everyone, no matter who they are or where they live, can choose to see their GP face to face and I am grateful to the Daily Mail for launching this campaign.’
The low level of face-to-face appointments comes despite official NHS guidance telling surgeries to offer in-person consultations if patients wanted them, unless there were good clinical reasons, such as Covid symptoms.
Many family doctors argue that phone or video appointments via Skype or Zoom allow them to handle more patients in a typical day.
Doctors’ leaders also argue a long-standing GP recruitment crisis has made it harder to see everyone in person.
But others believe the pendulum has swung too far and that it is vital to get back to pre-pandemic levels of face-to-face appointments so that fewer serious conditions are missed.

Many elderly people, not only in Hightown, are unable navigate so-called ‘Zoom medicine’. Another option is to travel to Formby, more than three miles away, where the parent surgery is located in Chapel Lane [File photo]
THE MAIL’S FIVE-POINT MANIFESTO FOR GPsA guarantee that face-to-face GP appointments are the default – and anyone who wants to see their family doctor in person should be able to do soThe Government should act to ensure a greater proportion of GP appointments are ‘in person’ – providing incentives or penalties for local surgeries if necessaryEnd of the postcode lottery so everyone has the same chance of seeing their doctor face to faceUrgent action to ensure the Government delivers on its election promise to recruit 6,000 more GPs and provide 50million more appointments a yearIf necessary, pharmacists or nurses based at GP practices should receive extra training so they can ease burden on doctors and help with face-to-face cases Advertisement
And campaigners say it is often the vulnerable or elderly who lose out by not being able to see their family GP as they normally would.
The Mail is demanding action from ministers and the medical authorities to ensure the proportion of appointments carried out face to face is radically improved.
This newspaper is also calling for action to ensure there is no postcode lottery in the system and for the Government to deliver on its pledge to recruit 6,000 more GPs.
Dennis Reed of Silver Voices, a campaign group for the over-60s, is pressing for patients to have a legal right to ‘face-to-face GP appointments’.
His petition on an official government website has more than 16,000 signatures, and a survey of more than 500 elderly people by his group in May found 71 per cent had struggled to obtain an in-person appointment with a GP.
Mr Reed said: ‘Primary care is not a welcoming service any more. If you can get through to your GP surgery on the phone, you’ll be interrogated by a receptionist and have to jump through so many hoops to get an appointment.’
Caroline Abrahams, of the charity Age UK, called for increased resources for GP practices to enable them to carry out more in-person consultations.
And Gavin Terry, of the Alzheimer’s Society, said: ‘Virtual GP appointments cannot become the norm for everyone with dementia, as many people experience communication issues, and their true condition might not be picked up.’
Alison Cook, who works for Asthma UK and the British Lung Foundation, said that most asthma sufferers have told them they prefer face-to-face care.
An NHS spokesman said last night: ‘Every GP practice must provide face-to-face as well as telephone and online appointments.’
Pandemic caused a plunge in numbers who saw a GP… and this year is set to be worse than last
By SHAUN WOOLLER, Health Correspondent, for the Daily Mail
Family doctors are seeing fewer patients in person than they did last year, despite the hugely successful vaccine rollout, better Covid treatments and a more stable supply of PPE.
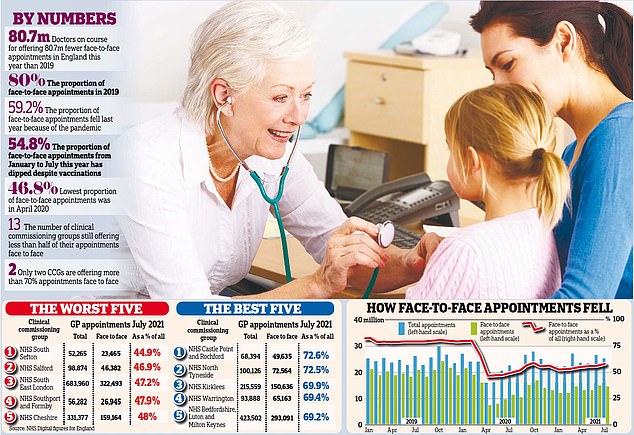
Shocking NHS figures reveal that patients were in the same room as their medic for just 54.8 per cent of consultations between January and July. That compares with 59.2 per cent last year, 80 per cent in 2019 and 82 per cent in 2018.

Overall, GPs are allowing 3.4 million fewer face-to-face consultations per month compared with before the pandemic [File photo]
Q & A
Q: Why are there fewer face-to-face appointments?
A: In March 2020, as the pandemic began, NHS England wrote to GPs to tell them to adopt a system of ‘total triage’. Patients were to be assessed on the phone or online to establish if they needed an in-person appointment.
The pandemic accelerated a move to more remote care that ministers had hoped to bring in gradually.
Q: What are the benefits of remote consultations?
A: They help to reduce the spread of Covid by limiting contact. Triage allows GP practices to filter out patients who could be dealt with by pharmacists, nurses or physiotherapists, leaving doctors more time to see people who really need their expertise.
Some queries can be answered quickly over the phone and some illnesses or conditions can be diagnosed from photographs or by video.
Some people prefer this because it saves the time of travelling to a surgery, which could mean taking time off work or having to arrange childcare. Some GPs like doing remote consultations as they are able to do them from home, rather than travel to their surgery.
Q: What are the downsides?
A: Campaigners warn it is now so difficult to see a GP face to face that some people have given up trying to get an appointment altogether. It can often be hard to get through on the phone.
Patients can feel uncomfortable being quizzed by a receptionist and those who are lucky enough to secure even a remote consultation may not have a smartphone or computer necessary for a video call or to send a photo.
Some feel uncomfortable talking about medical issues remotely and value the relationship they build with a doctor in the same room. Without physical examinations, doctors risk missing vital tell-tale symptoms.
Coroners warn it is difficult to give the same level of care during a remote consultation and problems are being missed – with fatal consequences.
Patients unable to secure a GP appointment are instead visiting A&E and piling pressure on already busy hospitals.
Q: Are GP surgeries back to normal after lockdown?
A: No. GP surgeries are seeing a lower number and lower proportion of patients face to face this year than last – despite the hugely successful vaccine rollout, better Covid treatments and a more stable supply of personal protective equipment.
NHS England wrote to surgeries in May telling them remote consultations could continue but they should be offered ‘alongside a clear offer of appointments in person’. It added: ‘Patients’ input into this choice should be sought and practices should respect preferences for face-to-face care.’
Rates have crept up only marginally and remain almost a third lower than pre-pandemic levels. In some parts of the country, still fewer than half of appointments are face to face.
Q: What other issues explain the crisis?
A: Doctors’ leaders cite ‘years of neglect’ of general practice by successive governments, which means there are too few GPs to meet demand.
The British population is ageing and more people are living with multiple, complex illnesses that place a bigger strain on primary care.
The Conservative Party’s 2019 election manifesto pledged to increase GP numbers by 6,000 by 2024/25.
The Royal College of General Practitioners and the British Medical Association say this is essential.
Q: What will happen next?
A: Health Secretary Sajid Javid has said it is ‘high time’ for GPs to start to operate in the way they were doing before the pandemic and he has vowed to ‘do a lot more about it’. GPs have pledged to offer a mix of face-to-face and remote consultations.
Campaign group Silver Voices, which represents the over-60s, has launched a petition calling for a legal right to in-person appointments.
Advertisement
The rest are conducted by telephone or video. However, this category also includes consultations at a patient’s home, which are extremely rare.
The figures also reveal that the figure for face-to-face appointments fell below 50 per cent during the lockdowns. GPs are on course to see 80 million fewer people face-to-face this year than in 2019, raising fears that more life-threatening conditions will be missed.
NHS England told surgeries in May to ensure they were offering face-to-face appointments to any patient who requests one.
But rates have crept up only marginally since, from 55.6 per cent that month to 57.2 per cent in July – still almost a third lower than pre-pandemic levels.
And the figures expose a postcode lottery of care, with just two local health areas – known as clinical commissioning groups – offering more than seven in ten appointments face to face.
NHS Castle Point and Rochford CCG topped the list with a rate of 72.6 per cent in July. But 13 CCGs are failing to offer even half of their appointments in person, with NHS South Sefton at the bottom of the league table on 44.9 per cent.
Dennis Reed, the director of Silver Voices, a campaign group for the over-60s, is leading calls for patients to be given a legal right to ‘timely face-to-face GP appointments’. His petition on the official Government website has more than 16,000 signatures and will be considered for a debate in Parliament if it reaches 100,000. A survey of more than 500 elderly people by the campaign group in May found 71 per cent had struggled to obtain a face-to-face appointment.
Mr Reed said: ‘If you can get through to your GP surgery on the phone you’ll be interrogated by a receptionist and have to jump through so many hoops to get an appointment. Many elderly people find this so daunting that they have just given up trying and are suffering at home. It’s very worrying and stressful for them.’
Mr Reed added: ‘We are worried that serious conditions are going undiagnosed, people are getting sicker and dying as a result. Ministers must get a grip on this now.’
Face-to-face GP appointments hit a low of 46.8 per cent in April 2020, the first full month after the first lockdown.
They remained below 50 per cent until August that year and have been above that level ever since.
But they are yet to return above 60 per cent in any month.
Lucy Watson, chairman of the Patients Association, said its helpline received regular calls from ‘frustrated’ and ‘distressed’ patients who can not see their GP face to face, and numerous health charities have warned of the harms of remote consultations.
Diabetes UK said it was ‘vital that those who weren’t able to access remote appointments were able to request face-to-face support’. Asthma UK said: ‘While some people with asthma may prefer phone and video doctors’ appointments because they can be more convenient, the majority have told us that they prefer face-to-face care. Some aspects of asthma care are currently more effective if delivered in person – for example, checking that someone is using their inhaler properly.’
And the Stroke Association said: ‘Some stroke survivors, particularly those with speech and communication difficulties like aphasia, have found online appointments challenging and felt it negatively affected the care they received. It is vital that stroke survivors have choices about how they access services in future, so they can receive the personalised support that best suits them.’ Professor Martin Marshall, chairman of the Royal College of GPs, said family doctors shared patients’ ‘frustrations’ with primary care.
He insists GPs have offered face-to-face appointments when needed but admits some have at times felt like they were working in a call centre, ‘which isn’t the job they signed up for’. He added that the real problem was a chronic shortage of GPs, which limited the total number of appointments available.
Professor Marshall said the move to ‘mainly’ remote consultations was in line with government guidelines, adding: ‘This was necessary for infection control and to keep patients – and GP teams – as safe as possible. Face-to-face appointments and physical examinations have continued throughout, wherever clinically appropriate and safe to do so.’
Dr Richard Vautrey, chairman of the BMA’s GP committee, said patients were seen in person when it is safe and clinically appropriate. He added that it had been necessary to cut back numbers to protect the public during the pandemic and the need to limit the spread of coronavirus remained.
‘Patients don’t want to come into the surgery with one illness, only to leave having caught Covid-19 as well. To protect our patients, we had to limit the number of people coming through our doors.’
Three anguished accounts of grief and pain that health chiefs MUST hear
by LIZ HULL for the Daily Mail
CASE ONE: We were fobbed off and now my mother is dead
The daughter of a woman who died of lung cancer months after being refused an appointment with her GP said: ‘Nobody will ever know if she could have been saved.’
Marina Sendall’s mother, Ellie Krzywy, 62, was ‘fobbed off’ by her GP surgery, which did not want doctors to see patients face to face during the pandemic.
Despite telling her family doctor she had a persistent cough and felt breathless in two phone consultations, Mrs Krzywy was not sent for an X-ray but was instead prescribed antibiotics for a chest infection.

Marina Sendall’s (L) mother, Ellie Krzywy, 62 (R), was ‘fobbed off’ by her GP surgery, which did not want doctors to see patients face to face during the pandemic. Despite telling her family doctor she had a persistent cough and felt breathless in two phone consultations, Mrs Krzywy was not sent for an X-ray but was instead prescribed antibiotics for a chest infection
Eventually, the cleaner’s condition became so bad that Mrs Sendall decided to take her to A&E herself. Doctors there X-rayed her chest and – after seeing something suspicious – referred her for more tests.
A week later, in August 2020, they delivered the devastating news that Mrs Krzywy had terminal lung cancer and only six months to live. She survived for longer before dying in May. Heartbroken Mrs Sendall, 34, told the Mail the GP who refused to see her mother had ‘robbed’ the family of precious time together.
The retail administrator said: ‘Covid was used as an excuse not to see her. It was impossible for my mum to get an appointment. She told them she had the cough for a few months but they still prescribed antibiotics over the phone. She should have been sent for an X-ray sooner.
‘My mum had an aggressive form of cancer. Who knows if she could have survived? No doctor can tell us that – but she would have had more time.
‘Instead the day she was diagnosed she had to start treatment straight away otherwise she would have had weeks [to live]. We would still have been waiting for the GP had I not taken her to A&E.’

In August 2020, they delivered the devastating news that Mrs Krzywy had terminal lung cancer and only six months to live. She survived for longer before dying in May. Heartbroken Mrs Sendall, 34, told the Mail the GP who refused to see her mother had ‘robbed’ the family of precious time together.
Mother-of-three Mrs Sendall added of the diagnosis: ‘We cried for four days straight after hearing the news – it was awful.
‘To hear she’d been suffering all those weeks with cancer was terrible. The Daily Mail campaign can only be a good thing.
‘Sadly, there are plenty of stories like my mum’s out there.
‘Somebody has to force the Government to do something. The past year has been a nightmare.
‘I was very close to my mum and I never thought I could survive losing her, but I’ve got three children myself so I’ve had to keep going for them.’
Distraught Mrs Krzywy, of Gloucester, had told of her ‘disappointment’ at not being able to get an appointment with her GP. She said at the time: ‘I felt completely helpless. I’m in shock that I have so little time left.’
CASE TWO: My husband should never have died
A heartbroken widow hailed the Mail’s campaign yesterday and vowed: ‘If that doesn’t move them into action then they’ve got hearts of stone.’
Lisa King, 55, sobbed as she told how she lost her beloved husband Peter after his GP denied him a face-to-face appointment. She said the 62-year-old retired taxi driver’s death had been ‘tragic and avoidable…just completely unnecessary’.
Mrs King insisted: ‘It should never have happened. Every night I cry myself to sleep and when I unfortunately wake up – I say unfortunately because I just want to be with him – I weep again. If it wasn’t for the fact we have children, I wouldn’t be here now – that’s how broken I am.’
Mr King, of Brentwood, Essex, complained of pain in his stomach in July last year. His wife emailed their GP asking for a face-to-face appointment because she was worried it was cancer.

Lisa King, 55, sobbed as she told how she lost her beloved husband Peter after his GP denied him a face-to-face appointment. She said the 62-year-old retired taxi driver’s death had been ‘tragic and avoidable…just completely unnecessary’
After a phone appointment, Mr King’s GP said he had acid reflux and prescribed medication, telling him to call back in a week if it had not improved.
Mr King was taken to hospital six days later and doctors removed a gallstone in his bile duct. It is thought the delay in treatment and going into hospital saw Mr King’s iron levels rise and damage his heart.
He had a heart attack four weeks after leaving hospital and died last October.
Mrs King said: ‘You can’t diagnose something like that over the phone. He passed away and it was all a result of not seeing his GP.
‘Our family has been torn apart by the incompetence and neglect. On September 30, 2020, Peter and I celebrated our 21st wedding anniversary. Nine days later, I was a widow at 55 and our two sons aged 21 and 19 will forever miss asking their dad for fatherly advice and sharing their experiences with him.’
She added: ‘No one goes to a GP because they have nothing better to do. They need treatment – there’s something wrong…Patients are losing trust in their doctors. They need to regain the public’s trust by seeing people face to face.
‘It seems as though GPs can do what they like. They can ignore patients, ignore the Health Secretary, the British Medical Association…They are a law unto themselves.
‘I hope this Daily Mail campaign can make a difference because I never want another wife, husband, son or daughter to have to go through what me and my two sons are going through.
‘Let them read Peter’s story. And if that doesn’t move them into action then they’ve got hearts of stone.’
CASE THREE: My head feels like someone is stamping on me
A woman had to undergo emergency surgery – after trying to get a face-to-face appointment with her doctor for more than a year.
Painter and decorator Katie Lee, 30, of Hartlepool, suffers from high pressure in her brain. She said since the pandemic started ‘it’s been impossible to get anyone to see me’. She added: I’ve been in terrible pain at times – as if my head is in a vice and someone is stamping on me.
‘I’ve tried getting through to my GP over and over but they don’t seem interested and kept putting me through to the hospital.
‘The pressure was becoming worse and worse. My vision was going. A simple eye examination could have shown something was seriously wrong.’

Katie Lee, 30, a painter and decorator is recovering in the James Cook Hospital in Middlesbrough after emergency surgery. She says: ‘I’ve been trying to get a face to face appointment with a doctor or a consultant for over a year but have been fobbed off with phone calls or online forms.’
She eventually saw a GP and later found out ‘I was only a cough or a sneeze away from having a stroke’.
Miss Lee said after the surgery ‘I can see again – but I feel like I’ve been hit by a bus’.
She called the GP service a ‘nightmare’, saying: ‘Every appointment has been over the phone and it’s not good enough.’
Why it’s crucial we save this life-saving human touch
by DR ARUN GHOSH

Dr Arun Ghosh
THERE is a case from the pandemic that will always stay with me of a man given appointments remotely. He was 24 and suffering from lower-back pain after exercising.
He was given a telephone assessment, and a colleague gave him ibuprofen and told him to rest. When the pain continued, again he booked in for a telephone call, and this time he was referred to a physiotherapist.
This young man had myeloma – a type of bone marrow cancer – which was eventually picked up late because he hadn’t actually been physically examined for almost six months.
I often think if he had been examined in person sooner, the doctor might have seen this was more than a simple back injury. Technology can work well for younger patients who need something straightforward, such as emergency contraception.
But my concern is that it really isn’t a replacement for a hand on the tummy or listening to someone’s breathing. As a junior doctor, you are taught to take a history of the patient’s symptoms, do a good examination, and then come up with a diagnosis.
On the phone, you can only really take someone’s history, and they may not think to tell you the most important symptoms – plus they only have a few minutes to tell you about it, as these appointments are generally shorter than face-to-face ones.
Even with video consultations, I often think afterwards, could I really be confident I had seen an infected insect bite, or was it a blood clot? Many GPs, especially locum doctors, now prefer remote appointments. They get paid to sit in their own home, which makes it easier to deal with family commitments.
But there are good reasons for face-to-face appointments. In a surgery a doctor can see from a patient’s medical records that someone hasn’t had their flu jab, or their child hasn’t had their vaccinations.
I also worry about the domestic abuse cases, where anxious women would repeatedly come in with children who had minor illnesses. We would ask questions about how they were coping, and then discover what was happening at home. But that is much harder to do on the phone or online, when they are speaking from home.
With phone appointments, there is also a risk that calls won’t be answered. And there is the importance of trust, now that most patients aren’t able to see the one family doctor they have had for years.
If a patient doesn’t feel the GP is really paying attention – often they can hear you typing as they talk – they may not provide all the information on their symptoms.
I want to embrace technology, but as a doctor who has been doing this for 20 years, I think face-to-face appointments are very important, particularly when it comes to mental health. Just seeing a patient in person, and reassuring them with a physical examination, can remove a burden they have been carrying for weeks.
Dr Arun Ghosh, 42, is a GP partner at Ghosh Medical, a private GP service run in Liverpool and across the North West.
DR MAX PEMBERTON: GPs who won’t see patients are hurting the NHS
At the age of 16, I started working for the NHS as an occupational therapy assistant. I later trained as a doctor because I was so proud of the NHS and the ideologies underpinning it. I have always thought of it as one of this country’s greatest achievements and over the 25 years I have worked in it, I have vociferously defended it.
This makes what I’m about to say all the more sad. I used to love the NHS but, increasingly, I feel my relationship with it is on the rocks.
I’ve never been so naive as to think the NHS is perfect. Far from it. Of course it has its faults. But I always argued that it was an equitable and cheap way of delivering healthcare.
Yet I — and many others — are starting to question who the NHS is for. Increasingly, it seems to be less and less about patients.
At the start of the pandemic we rightly rallied round, protected the NHS from being overwhelmed and applauded the staff on the front line.
But 18 months later, the goodwill the NHS built up is quickly being squandered.
Despite it now having had two years to prepare, we are still being told the NHS is at risk of collapse if there is another Covid wave; and we face the possibility of yet more lockdowns. What has the NHS been doing all this time if not getting itself prepared?

Dr Max (pictured) said rather than spending our time wishing away the years until we retire, perhaps the answer is to focus our energies on finding a job we don’t want to retire from
But surely most galling of all is that so many GPs are still refusing to see patients face to face. It has become a national crisis. Yet still many of my GP colleagues refuse to accept there is a problem.
They insist that, despite all the evidence, they still provide an adequate service. Move along. Nothing to see here.
Do they take us for fools? They are in denial. Seeing a doctor in person has become nigh-on impossible lately. This after Greater Manchester’s senior coroner reported that lack of face-to-face assessment had contributed to at least five deaths and warned of more to come.
Statistics released last week also suggest a lack of in-person appointments may have led to an 88 per cent spike in stillbirths in England during the pandemic.
Just this week my mum called me in a dither about my auntie, who had an infection but had been unable to see a GP. She ended up seeing a pharmacist privately who prescribed antibiotics but was only allowed to give a few days’ worth — the rest needed to be prescribed by a GP.
Yet the surgery informed her she still couldn’t see a GP until long after the course of antibiotics ran out. Utter chaos.
Like many others, my aunt had to resort to seeing a private GP, despite not really being able to afford it. My mum was beside herself with worry in case something similar happened to her, and wanted to know what she should do. I felt profound shame in the NHS when I had to say she should go private.
My mum, a staunch socialist, was horrified: ‘Is this really what we’ve come to in this country?’ she texted me afterwards.
Then, just days later, a man who works in my local dry cleaner’s texted me in desperation, asking what he should do because his wife was unwell but couldn’t get hold of a doctor.
Don’t tell me this is all just a coincidence. It is getting ludicrous. There was the atrocious case last week of a woman being unable to get an appointment for her son to see a GP, so in despair she paid for a private GP . . . only to find that the private GP was in fact the NHS GP she couldn’t get an appointment with.
People will only tolerate so many stories like this before there is a mutiny.
Nye Bevan, the father of the NHS, set out his idea for the Health Service in a book entitled In Place Of Fear — because that’s what he believed the NHS was.
Before it, people were scared of falling ill because it could bring financial ruin on a family. What a noble cause to address.
People are scared once more —but now it is because they feel the NHS isn’t there for them. They are scared they won’t get the help when they need it, won’t know where to turn and, increasingly, will have to pay for medical help. And it’s not just GPs. Hospital services that effectively shut up shop at the start of the pandemic have been woefully slow in starting up again.
Waiting lists for life-changing operations such as hip replacements are spiralling out of control — and the only solution seems to be to go to the Government, cap in hand, and ask for more money. The whole thing just feels so disheartening.
This isn’t about bashing the NHS for the sake of it. It’s about it being exposed as an antiquated, creaking system that can’t adapt fast enough to the demands being placed on it.
It’s about an institution based on a hotchpotch of short-term solutions that have been imposed by politicians in a haphazard way on an anachronistic model over the years that is now at death’s door.
It’s about a society that for years has had high expectations and a sense of entitlement but whose citizens don’t appreciate the cost of what they receive.
It’s about watching something I loved slowly die — and wishing the end would come sooner, because it’s agonising watching the death throes.
CAMILLA CAVENDISH: Backbone of the NHS… so why DO so many GPs avoid patients?
When Brian Mottram died from Covid-19 pneumonitis last November, he had been prescribed antibiotics by a GP over the phone. In Tameside, where Mr Mottram lived, the GP clinics had a policy of predominantly using telephone consultations rather than face-to-face or video appointments. As a result, no one realised what was wrong with him until he died.
A senior coroner has said that remote GP appointments may have been a factor in Mr Mottram’s death and that of four others in Greater Manchester.
The coroner’s report has bust open the anguish that has been simmering ever since the start of the pandemic: where have all the GPs gone?
Paramedics, pharmacists, ambulance drivers and care workers have dealt with people face to face throughout the pandemic. Nurses and hospital doctors have worked tirelessly on the wards. Yet many patients feel their GPs have become invisible. Despite the heroic efforts of some GPs, the service that ought to be the backbone of the NHS is crumbling.

Many patients feel their GPs have become invisible, writes Camilla Cavendish
Before the pandemic, around eight in ten patients saw their GP face to face. Now it’s under six in ten, with big variations around the country. But even these figures mask the fact that many people I know have not been able to get a GP appointment of any kind.
Earlier this year, a friend of mine noticed something worrying on her shoulder. A mole she’d had for years had started bleeding. Not only did it look awful: Google made it clear it could be cancerous. ‘See your GP if you notice a change in a mole,’ urges the NHS website. But that turned out to be impossible.
After dialling and re-dialling her GP for days, she finally got through to a brusque receptionist who asked: ‘Why are you bothering us with this?’ An astonishing comment. No, she couldn’t have an appointment this week. Or next week. Or it seemed, ever. Her anxiety mounting, she managed to get them to agree that she could send in a photo. The GP would look at it and call her, she was told. She never heard back. ‘I’ve given up,’ she says now. ‘It hasn’t got any worse, so I’m just hoping for the best.’
I hope the GP did look at the photograph, and decided that it wasn’t a problem. Remote consultation is convenient for doctors, and should in theory be more efficient. It also works well for patients with busy lives and relatively straightforward conditions.
Private services like Babylon Health have taken off in recent years because they let busy urban professionals get medical advice on video when they want it.
But with more complex conditions, talking to someone online is no substitute for examining them. One GP friend of mine is certain she saved a child’s life from meningitis, a few years ago, when she spotted a tiny rash behind the ear. It was a pin prick she thinks she would never have seen on video.

I could see manifest benefits for hard-pressed doctors in being able to switch to Zoom, writes Camilla Cavendish
Others tell me that listening to a heartbeat, testing reflexes, poking the abdomen, can provide clues that nothing else can. Especially if a doctor is examining someone they’ve seen over many years, they will notice if someone has lost weight, or is looking different.
As Professor Martin Marshall of the Royal College of GPs has put it: ‘The biggest challenge is when patients have complex health needs: as being in the same room as a patient, often who you have built up a relationship with over time, is incredibly useful and difficult to replicate remotely.’ GPs are also trained to pick up non-verbal cues: a child’s silent distress or a woman’s attempt to hide her bruises. We patients may struggle to say what’s bothering us.
‘Sometimes it’s only in the last 30 seconds, when the patient is putting their jacket back on, that they’ll say what they really came for,’ another GP tells me.
So when senior NHS executives started telling me excitedly last year that technology was going to revolutionise GP consultations, I felt worried. I could see manifest benefits for hard-pressed doctors in being able to switch to Zoom.
But equally it seemed vital to me that patients who wanted to see their GP could still do so.
I also wondered just how much more efficient the new system would be. Many surgeries are forcing patients to have a phone consultation first, before the doctor will decide whether to see them in person. But that can end up meaning two appointments for the same issue.
For years, getting an appointment has increasingly felt like breaking into Fort Knox.
If we reach the waiting room, we are assailed by signs warning us not to bring more than one ailment to each consultation. The doctor barely glances at us, so fixated are they on typing on their screen, and we rarely see the same doctor twice.
Continuity of care – having a GP who has known you and your kids for years, and who may therefore have deeper insights – is a thing of the past. When one of my favourite GPs took early retirement five years ago, it was because he was so frustrated by this lack of continuity, coupled with bureaucracy that meant he spent hours form-filling.
The result is a tragedy: a service that feels more and more like a job, not a vocation. The trouble started back in 2004, when the Government let GPs abandon out-of-hours care with no loss of salary. The days of GPs like my father-in-law, who would go to see patients at night and weekends, were over. From then on, we discovered that if we got ill at night or at a weekend, we were no longer the GP’s responsibility.
Remote consultation is accentuating the feeling some patients now have that their doctors see them as an irritant to be avoided. This is unfair to those GPs who are working incredibly hard, but it is undermining the doctor-patient relationship. At the start of the pandemic, patients were told to stay away from surgeries.
Eighteen months later, this is in danger of becoming a new normal, not least because GPs themselves seem to be so nervous about getting ill. A survey of 1,000 GPs in Pulse magazine has found 61 per cent saying they are ‘concerned’ about their own health.
Almost every GP I meet is unhappy and stressed. Almost every patient is anxious and furious. NHS England should urgently hire more GPs, relieve them of paperwork and support them with better administrators. But we also need to properly restore face-to-face consultations. Otherwise we will see more anguish, more anxiety, and more deaths that might have been avoided.
Camilla Cavendish is a Financial Times columnist.
Source link : https://www.dailymail.co.uk/news/article-10007039/Growing-toll-illnesses-missed-remote-doctors-fuels-concerns-healthcare-appointments.html











