More than 100,000 Americans are currently hospitalized with COVID-19 for the first time in eight months as the fourth wave of the pandemic continues.
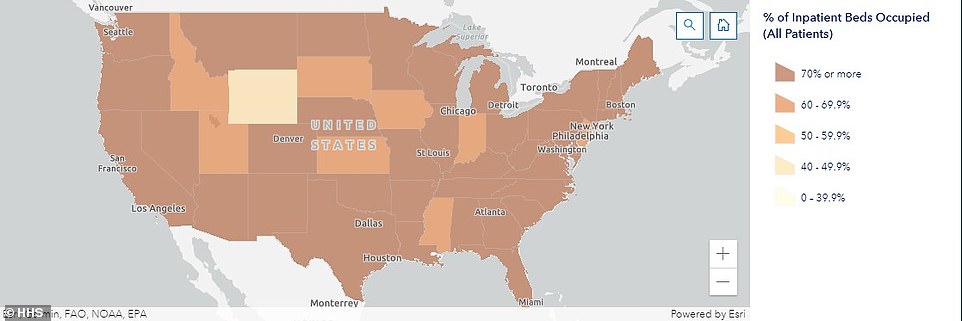
According to data from the Department of Health and Human Services (HHS), 101,050 hospital beds are occupied by people receiving treatment for the virus.
This is a 147 percent increase from the 40,791 patients who were hospitalized with COVID-19 four weeks ago and the first time this number has hit six figures since late January during the deadly winter 2020-21 surge.
What’s more, the number of people hospitalized with Covid is more than double the nearly 49,000 hospitalizations recorded on the same day in 2020.
Doctors say they’ve had to turn away patients because they don’t have enough beds to treat both virus patients and those seeking care for unrelated issues.
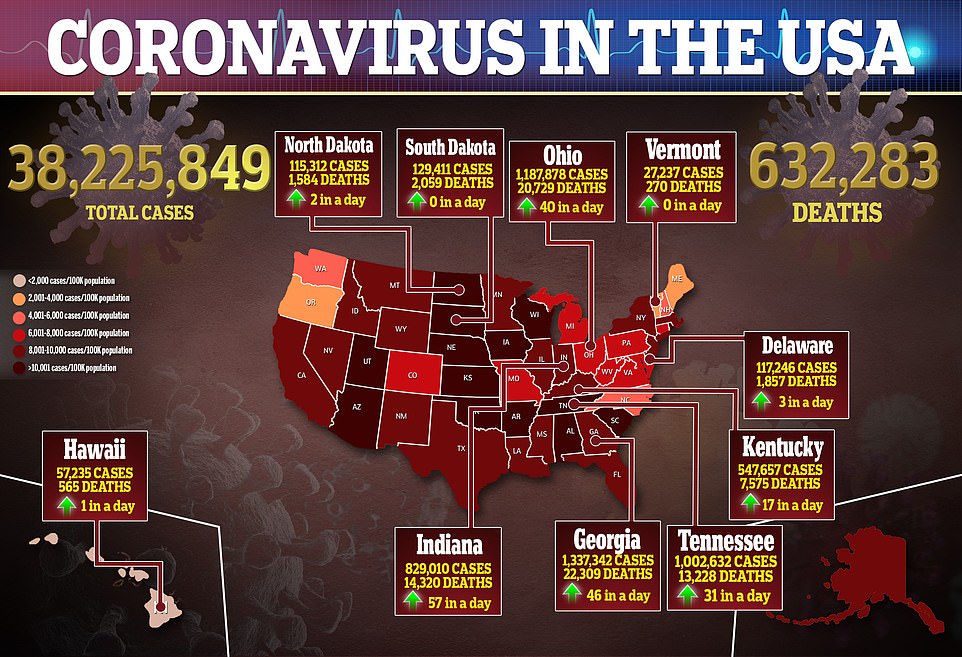
It comes as the U.S. recorded 148,143 cases of COVID-19 on Wednesday with a seven-day rolling average of 152,480, which is a 138 percent increase from the 63,842 average reported four weeks ago, according to figures compiled by Johns Hopkins University.
Deaths are also on the rise with 1,456 fatalities recorded and a seven-day rolling average of 1,100 – the fifth day in a row the average has surpassed four figures.
This marks a 291 percent increase from the average of 281 reported 28 days ago prior and the highest number reported since March 20.
More than 100,000 Americans are currently hospitalized with COVID-19 for the first time since January
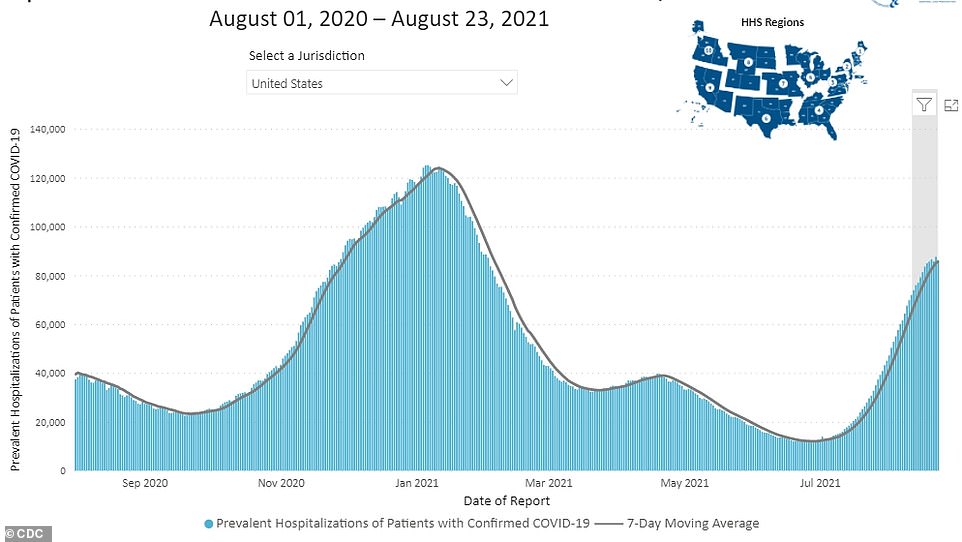
The 101,050 figure is a 147 % increase from the 40,791 patients who were hospitalized with the virus four weeks ago
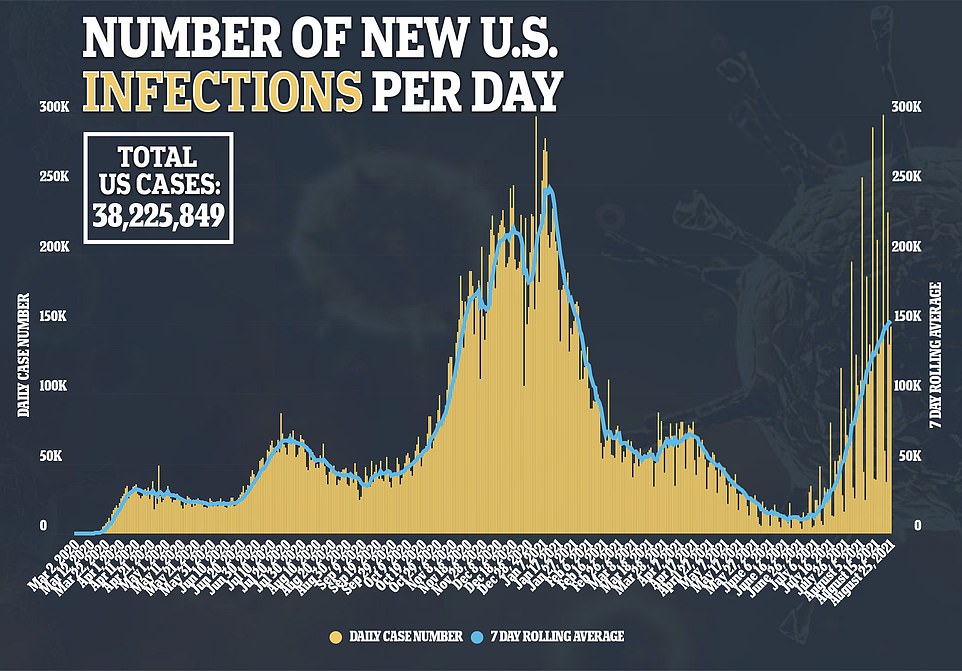
On Wednesday, the U.S. recorded 148,143 cases of COVID-19 with a seven-day rolling average of 152,480, which is a 138% jump in the last month
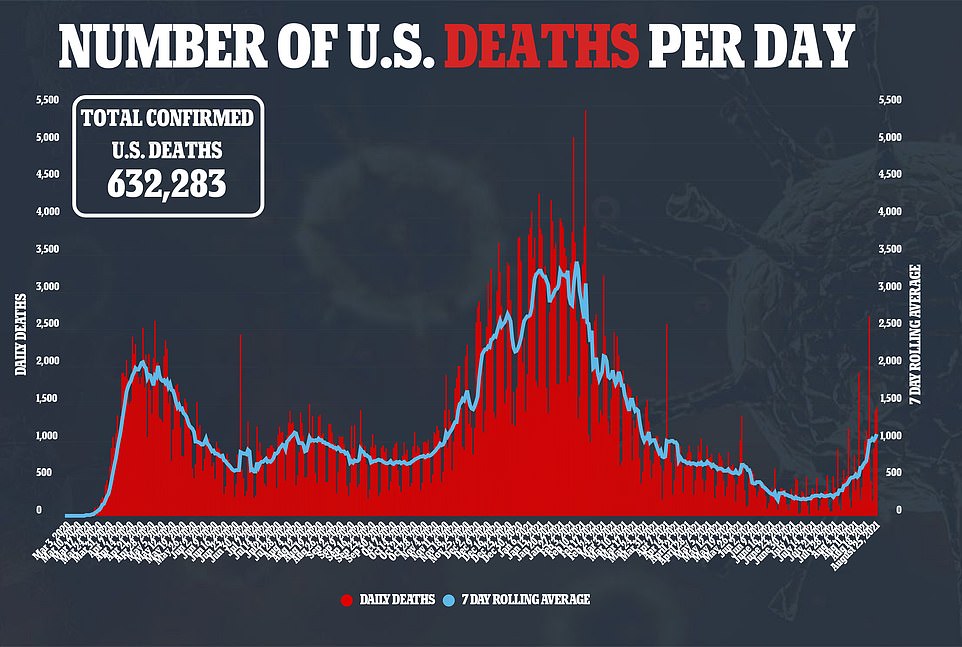
Deaths also rose with 1,456 fatalities recorded on Wednesday and a seven-day rolling average of 1,100, a spike of 391% from the average seen 28 days prior
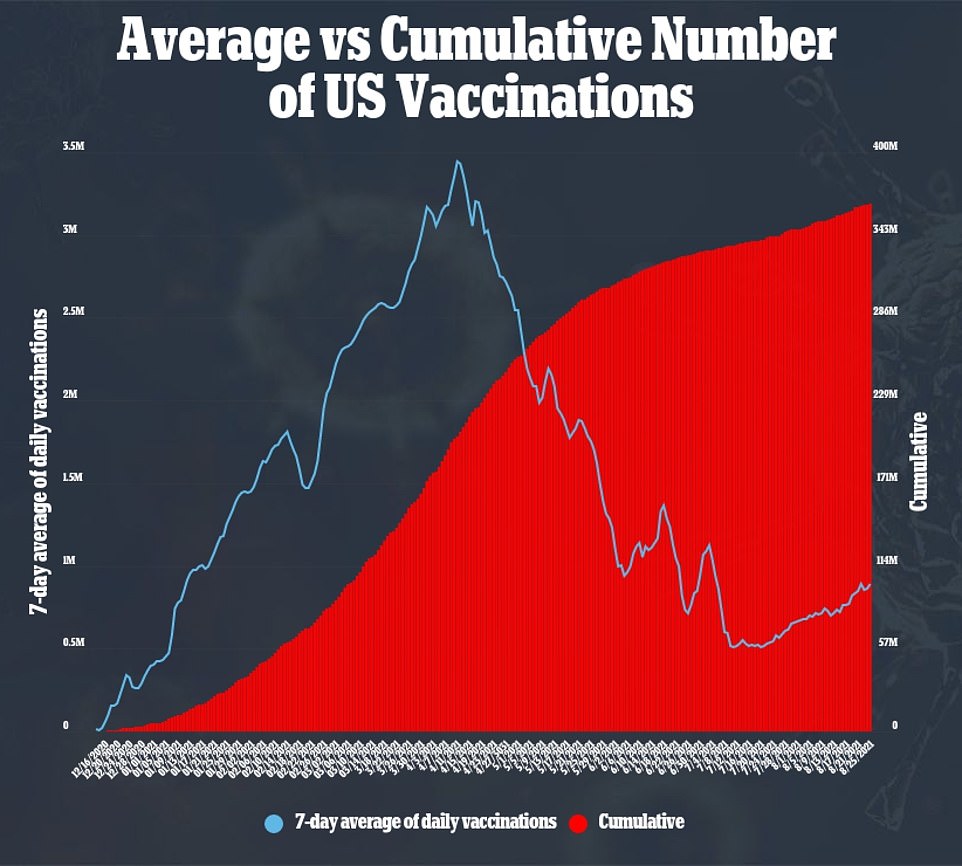
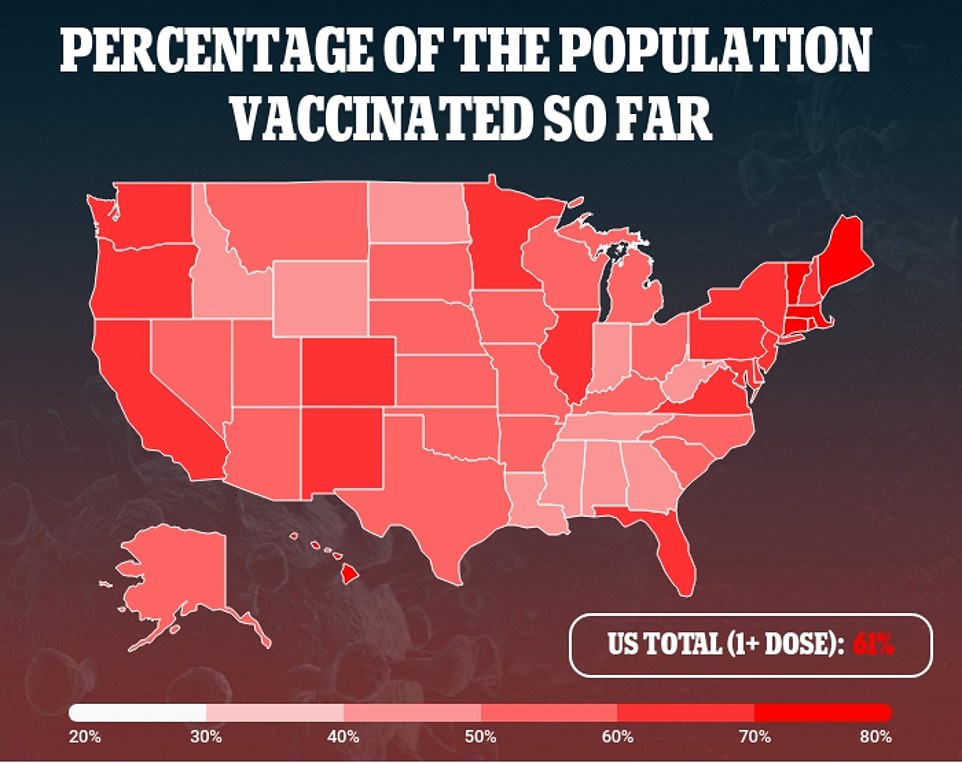
With about half of the U.S. population still not vaccinated against COVID-19 – according to the Centers for Disease Control and Prevention – hospitals are feeling strained as cases surge and beds get filled up.
Florida is currently experiencing the worst rate per capita in American with 80 hospitalizations per 100,000 people, according to HHS data.
Rounding out the top five are Alabama, Louisiana, Mississippi and Georgia, all of which are reporting more than 54 hospitalizations per 100,000.
‘I had to turn away a cancer patient that needed emergency treatment simply for the fact that because my hospital didn’t have any beds,’ Dr Nitesh Paryani, an oncologist at St Joseph’s Hospital in Tampa, Florida, told Bay News 9.
‘[The Indian ‘Delta’ variant] is just ripping through the hospitals in ways that we couldn’t have imagined and the strain it is causing on the health care system is unimaginable.’
He said that, recently, the emergency room at the hospital had a 12-hour wait for those seeking care.
Other hospitals across the country are reporting similar situations.
In New Mexico, 433 people are hospitalized, a 386 percent spike from the 89 hospitalized one month ago and a figure not seen since early February, state data show.
During a press conference on Wednesday, Dr David Scrase, acting Department of Health Secretary, said that New Mexico’s hospital system is days away from reaching ‘crisis standards of care’ status.
‘What it means is any of the normal routine services you would get for non-life-threatening emergencies may be less available,’ he said.
‘But in the end, what it really means is that we’re going to have to choose who gets care, who doesn’t get care, and we do not want to get to that point.’
The last time the state reached this status was in December 2020, when the country was well into third wave of the pandemic.
According to HHS data, 83 percent of ICU beds in New Mexico are occupied and nearly a third are being used to treat COVID-19 patients.
However, according to Scrase, the state has a waitlist of around 50 people waiting for ICU beds including in Albuquerque, the state’s largest city.
‘It’s a completely new phenomenon. You don’t take a lot of people off a waiting list when all of your beds are full, and that’s the problem,’ he said.
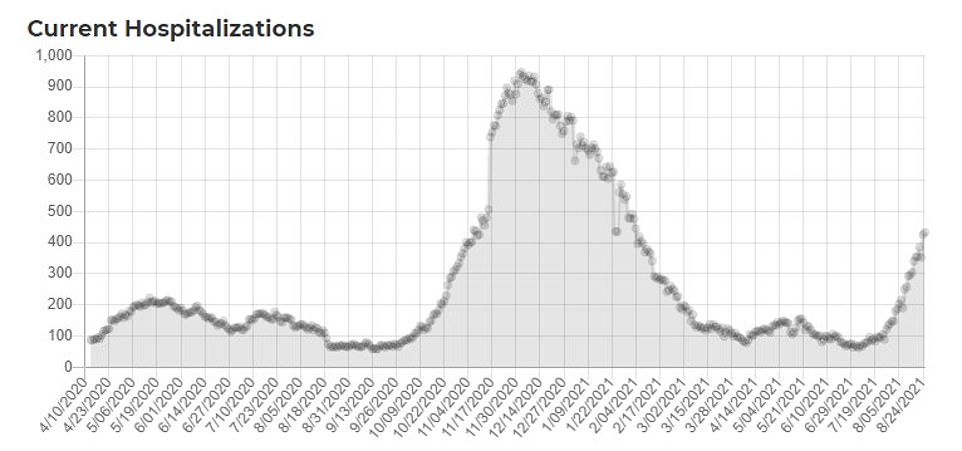
In New Mexico, 433 people are hospitalized with Covid, a figure not seen since February, and officials say the state is days away from reaching ‘crisis standards of care’ meaning doctors will have to decide who gets care
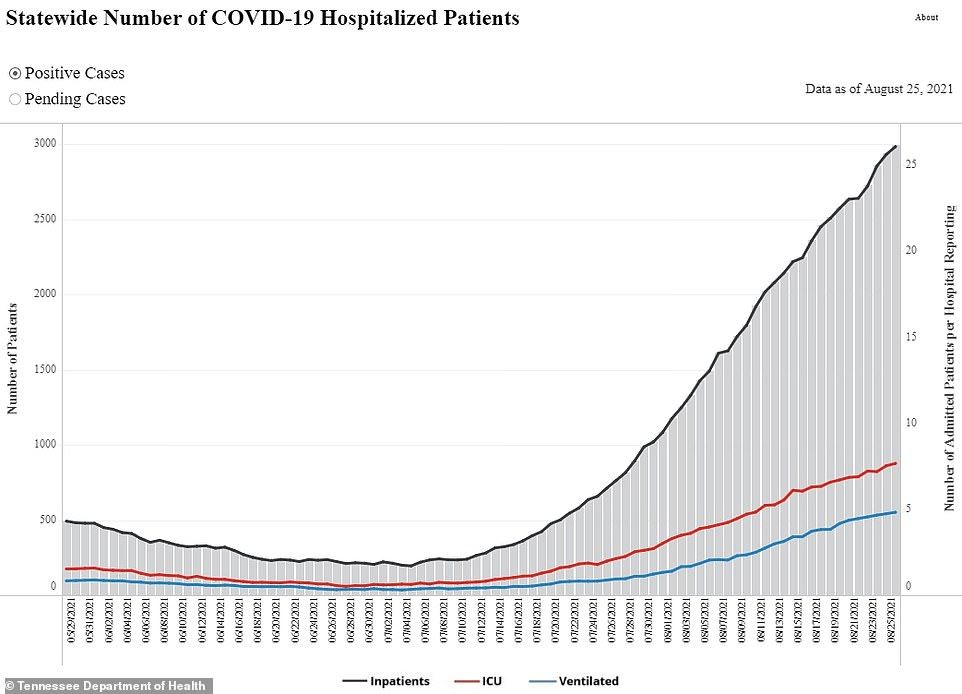
In Tennessee, 2,984 patients are hospitalized with COVID-19, a 319% jump from 712 one month ago, and hospitals say they have had to divert people to other medical centers
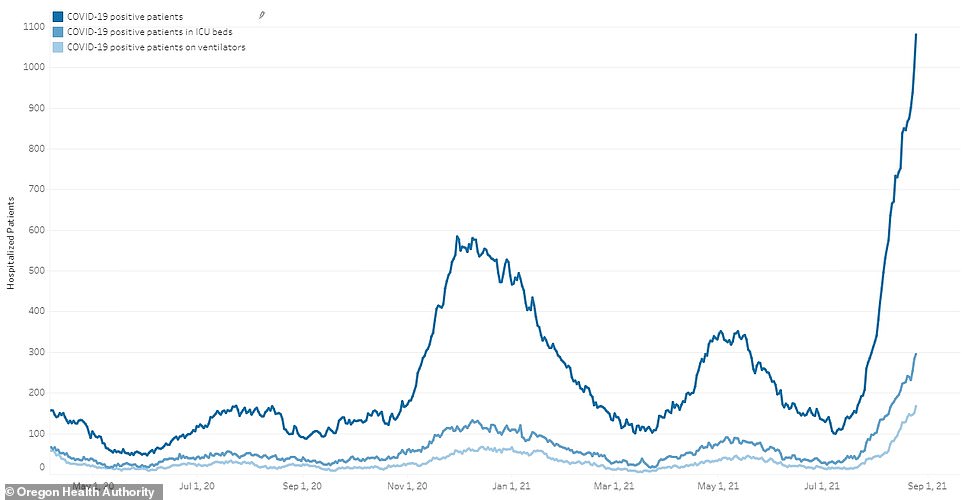
Oregon has a record-high 1,080 patients hospitalized and Gov Kate Brown announced the state is deploying ‘crisis teams’ of frontline workers to the hardest hit regions
In Tennessee, 2,984 patients are hospitalized with COVID-19, a 319 percent jump from 712 one month ago, and nearing the record 3,230 seen in early January, according to state data.
Dr David Sellers, the chief of staff at Ascension St Thomas Rutherford Hospital in Murfreesboro – 30 miles south of Nashville – said the hospital’s critical care unit has been at capacity for the last week.
About 60 percent of patients in the unit are infected with COVID-19.
‘For the immediate future, my focus is preparing for the worst,’ he told WKRN.
‘I’m preparing for more numbers to come in, preparing for maybe some of my physicians going down with this illness as well, since we’re exposed to it all the time. I mean, that’s just a reality that can happen.’
He explained that his hospitals and others have had to send patients elsewhere for treatment or, in other instances, turn patients away.
‘What it does is it causes us to have to ship patients elsewhere, or worse, patients coming from other facilities that are relying on our hospital because they’re in a small area…they can’t come to our facility, because we can’t accept them because we’re on diversion is what we call it when we don’t have the capacity anymore,’ Sellers said.
‘Those smaller facilities end up having to call around and just try to find a facility who can take care of their patient.’
In Oregon, a record-high 1,080 patients are hospitalized, which is a 990 percent increase since July 9, according to state health officials.
There are also fewer than 50 ICU beds available across the state with some hospitals reporting that patients have have been set up in beds in hallways.
On Wednesday, Gov Kate Brown said Oregon is deploying ‘crisis teams’ including nurses, respiratory therapists and others to areas that have been the hardest hit by the latest surge.
At least 500 front line workers are being sent to central and southern Oregon while smaller teams will be sent to other regions.
‘The deployment of crisis response teams should provide some welcome relief to our hospitals,’ Brown said during a press conference.
‘The hospital crisis we are facing isn’t just about beds – it’s about having enough trained health care professionals to treat patients.’
Source link : https://www.dailymail.co.uk/health/article-9929493/More-100-000-Americans-hospitalized-COVID-19-time-January.html











