Scientists have developed a new kind of Covid test which can detect the virus in spit – and tell infected people which variant they caught.
Researchers at Harvard University, the Massachusetts Institute of Technology (MIT), and several hospitals in Boston developed the home test.
The $6 (£4.30) test called Minimally Instrumented SHERLOCK (miSHERLOCK) can distinguish between three types of the virus and takes one hour to provide results.
It links to smartphones and can be configured to identify different variants, including the Indian ‘Delta’ strain.
Developers say it could replace lab-tested PCR tests to provide an accurate result much quicker than having to wait a day or two.
And the fact the tests do not involve an invasive nasal swab could make them more popular.

Scientists have developed a new kind of Covid test that can detect the virus in people’s spit. Pictured: The $6 (£4.30) test called Minimally Instrumented SHERLOCK (miSHERLOCK) after a positive result
They can spot Covid 96 per cent of the time and correctly identify 95 per cent of uninfected people.
Current genetic sequencing tests – which work out what variant someone has – can take several weeks to carry out.
Xiao Tan, one of the developers of the test, said: ‘Our goal was to create an entirely self-contained diagnostic that requires no other equipment.
‘Essentially the patient spits into this device, and then you push down a plunger and you get an answer an hour later.’
The device works using CRISPR technology — a controversial gene editing tool that has been used to detect HPV, a virus that causes several types of cancer — to detect Covid in the saliva.
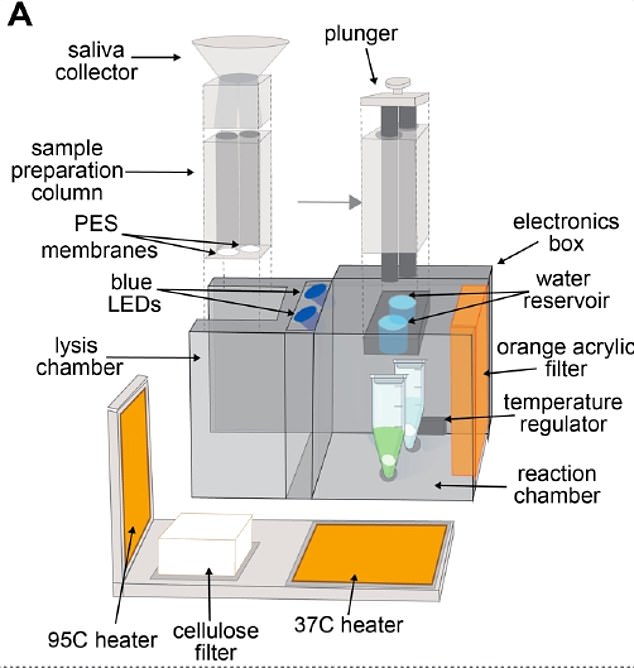
The device contains two chambers – one to spit in and one where the reaction takes place

The glow for a positive test can be seen with the naked eye but the developers also designed an app using a phone camera to help people read the results if they are not clear
HOW DOES CRISPR DNA EDITING WORK?
The CRISPR gene editing technique is being used an increasing amount in health research because it can change the building blocks of the body.
At a basic level, CRISPR works as a DNA cutting-and-pasting operation.
Technically called CRISPR-Cas9, the process involves sending new strands of DNA and enzymes into organisms to edit their genes.
In humans, genes act as blueprints for many processes and characteristics in the body – they dictate everything from the colour of your eyes and hair to whether or not you have cancer.
The components of CRISPR-Cas9 – the DNA sequence and the enzymes needed to implant it – are often sent into the body on the back of a harmless virus so scientists can control where they go.
Cas9 enzymes can then cut strands of DNA, effectively turning off a gene, or remove sections of DNA to be replaced with the CRISPRs, which are new sections sent in to change the gene and have an effect they have been pre-programmed to produce.
But the process is controversial because it could be used to change babies in the womb – initially to treat diseases – but could lead to a rise in ‘designer babies’ as doctors offer ways to change embryos’ DNA.
Source: Broad Institute
Advertisement
A person spits into a tube which leads into a heated sample preparation chamber.
They wait three to six minutes until the saliva has been wicked into a filter.
After that, they take the filter out and plunge it into the reaction chamber, where it goes into two vials containing the CRISPR technology.
CRISPR’s ‘molecular scissors’ are able to cut a specific strand of DNA that only exists in a given strain of SARS-CoV-2.
If the person is positive for Covid, a chemical reaction will cause the vial to glow fluorescent inside the box after around 55 minutes.
The glow can be seen with the naked eye but the developers also designed an app using a phone camera to help people read the results if they are not clear.
Dr Helena de Puig, co-first author and postdoctoral fellow at the Wyss Institute and MIT, said: ‘miSHERLOCK eliminates the need to transport patient samples to a centralised testing location and greatly simplifies the sample preparation steps, giving patients and doctors a faster, more accurate picture of individual and community health, which is critical during an evolving pandemic.’
The device components currently cost $15 (£10.80) to assemble, but the researchers say it would only cost $6 (£4.30) if made at mass scale.
They are also excited by the technology’s ability to detect specific variants.
Researchers tested their diagnostic device using clinical saliva samples from 27 Covid patients and 21 healthy patients.
The results, published in the Science Advances journal today, show the tests were about as accurate as a gold-standard PCR test.
They also tested its performance against the Alpha, Beta, and Gamma variants by spiking healthy human saliva with RNA containing mutations representing each variant, and found that the device was effective at spotting all three.
Dr de Puig said: ‘The ability to detect and track these variants is essential to effective public health.
‘But unfortunately, variants are currently diagnosed only by nucleic acid sequencing at specialised epidemiological centres that are scarce even in resource-rich nations.’
Source link : https://www.dailymail.co.uk/news/article-9868303/Scientists-develop-new-kind-Covid-test-detect-virus-peoples-spit.html











