More than 150 care homes across England have suffered at least 20 Covid deaths since the start of the pandemic, official data shows.
Figures released by the Care Quality Commission today — the first of their kind — showed nearly 7,000 facilities saw at least one coronavirus death.
Bedford Care Home in Leigh, Greater Manchester, had the worst virus death toll in the country, with 44 victims — 24 per cent of the home’s capacity.
But the second worst hit home in England — Calway House in Taunton, Somerset — had 41 fatalities, almost half its total number of beds (92).
Almost 40,000 care home residents have died from Covid, with the scandalous toll largely blamed on the move to discharge thousands of hospital patients into homes without testing them during the early days of the pandemic.

Bedford Care Home in Leigh, Greater Manchester, had the worst virus death toll in the country, with 44 victims — 24 per cent of the home’s capacity — Care Quality Commission has revealed
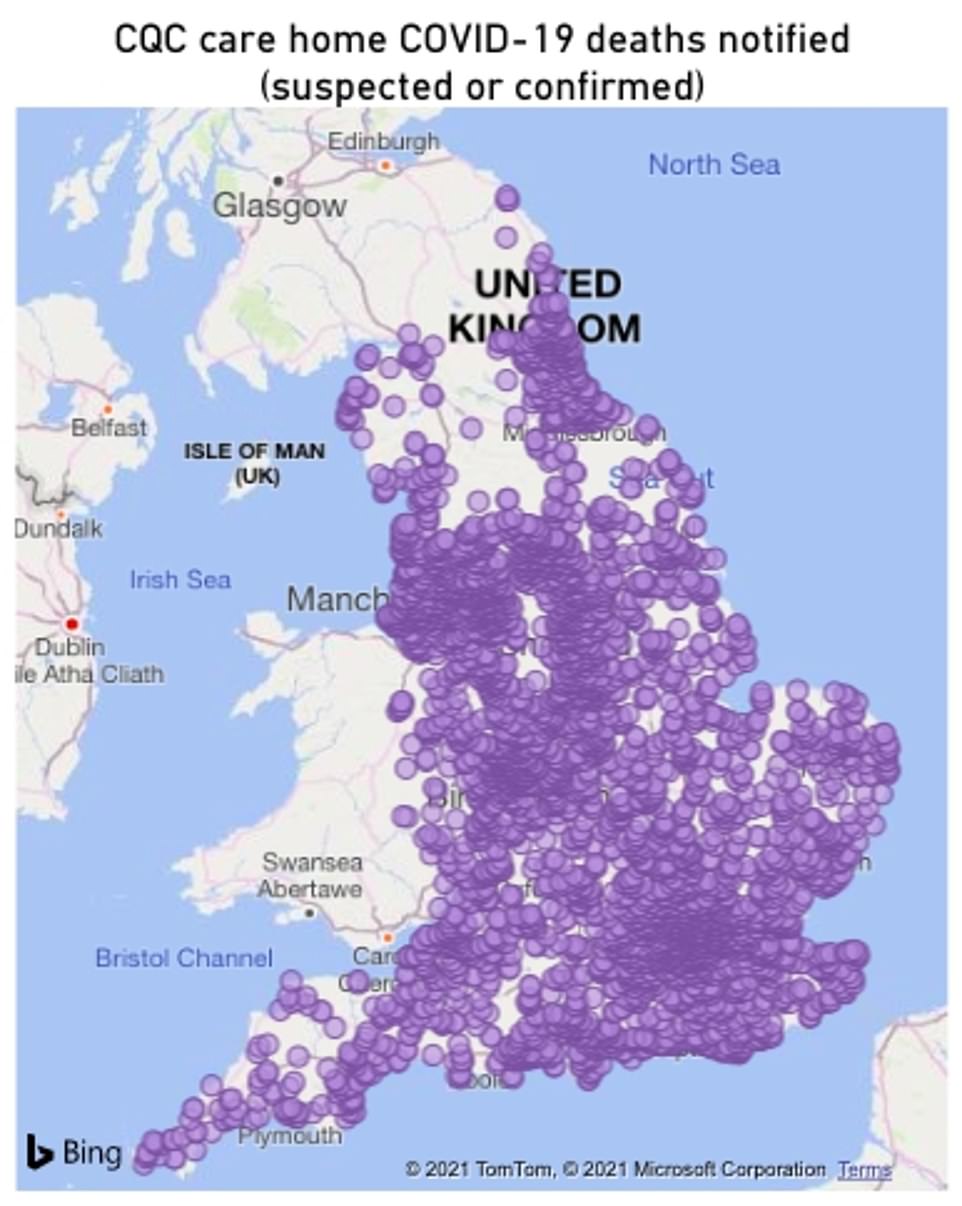
Nearly 7,000 homes saw at least one coronavirus death from April 2020 to March 2021. Map shows: All the care homes included in the CQC’s data release today
Boris Johnson is forced to put off announcing social care reforms until AUTUMN
Boris Johnson has been forced to put off announcing his social care reforms until the autumn after he failed to reach agreement with leading ministers.
He was understood be considering a 1p-in-the-pound increase in National Insurance (NI) contributions to fund his long-awaited plans.
But critics said such a plan would hit the low-paid and would spare even well-off pensioners – including those still working – from having to contribute anything to the cost of the new care system.
The plans are understood to include measures to integrate the NHS better with the local-authority-run social care system, to ensure elderly people are properly cared for. There will also be reforms to ensure better training.
It had been hoped that Mr Johnson would be able to bring forward his proposals – first promised almost two years ago – this week, before Parliament rises for its summer recess.
But the Prime Minister has been forced to isolate along with the Chancellor after Health Secretary Sajid Javid tested positive for Covid, meaning neither could unveil the reforms in the Commons.
It means the proposals will not be published until September at the earliest, leaving families facing sky-high care bills. Caroline Abrahams, charity director at Age UK, said the delay was deeply disappointing.
‘Every day the Government delays acting on social care, the more older and disabled people suffer, and the more pressure is diverted onto the NHS,’ she added.
‘We are also conscious that the experts are telling us to expect a difficult autumn and winter, due to Covid-19 and its variants, and because other respiratory viruses may become more prominent.
‘As a result, there’s a risk social care gets forgotten and that would not only breach the PM’s promise, it would be a tragedy for our older population too.’
Advertisement
The data released by the CQC — which regulates and inspects health and social care services in England — today was the first to reveal death tolls in nearly 6,971 individual homes across the country.
It did not include all care homes — with some smaller ones omitted to protect victims’ identities — so the true toll is likely to be higher. There are around 15,000 facilities dotted across the country in total.
CQC said it could not provide up to date occupancy numbers because the number of residents in homes varies day to day and it is impossible to offer accurate estimates over the course of the year.
Capacity figures also cannot be used to determine the proportion of residents who died because they do not give a fair reflection of how many people were living in homes over the year.
For example, homes can have multiple residents occupying the same bed at different times over a year, so it is impossible to determine the proportion of residents who died over the course the eleven months.
CQC added deaths were largely influenced by the way the virus spread in different areas of England, rather than being a result of the homes themselves.
Deaths were recorded as ‘involving Covid’ and provided by the care homes themselves, so may not reflect a doctor’s opinion that residents died because of the virus, the CQC said. Not all residents were tested in the early days of the pandemic.
And not all Covid deaths occurred in the homes themselves, with many taken to hospital for treatment and sometimes catching the virus there. CQC said 25 per cent of all care home resident Covid deaths occurred outside care homes.
Figures show a total of 152 homes recorded more than 20 deaths during the period, nine of which are classified as ‘medium-size’ — meaning they had a maximum of 49 residents at a time.
The Heathers Nursing Home in Bromley, Staffordshire, lost 31 residents to the virus — 61 per cent of its total capacity.
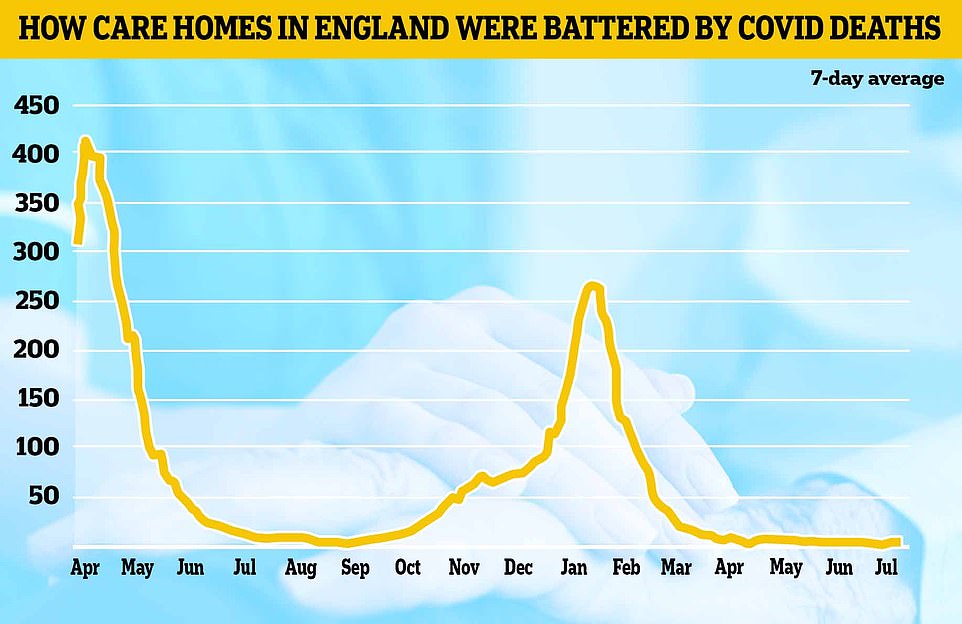
Some 18,329 deaths (46 per cent) occurred between April 10 and June 30 last year, during the first wave of the pandemic.
In contrast 13,343 (34 per cent) were from January 1 to March 31, which includes the height of the second wave, when deaths and cases were highest in wider society.
Care charities voiced their support to the families of the bereaved and paid tribute to the staff for their ‘heroic’ efforts on the frontline of the pandemic.
Professor Martin Green, chief executive of Care England, said: ‘Care homes have been right at the front line of this dreadful pandemic.
‘My thoughts go out to all those bereaved relatives as well as those dedicated staff who have been on high alert often working around the clock with no end in sight as well as all bereaved relatives.
Care home devastated by coronavirus: Two-thirds of the 27 elderly residents at a Lincolnshire care home die during second wave 
Staff at The Old Hall in Halton Holegate, Lincs, which has been hit by a coronavirus outbreak
A Lincolnshire care home boss has described the ‘absolutely horrendous’ ordeal of seeing 18 elderly residents die in a coronavirus outbreak.
All residents and 20 staff members at The Old Hall at Halton Holegate, near Spilsby, became infected with the virus in November, with the first resident dying on the 16th.
Over the next six weeks another 17 people died from Covid. Most were in their 90s, with the youngest aged 79 and the oldest 99.
Some of the deaths were so sudden staff did not have the chance to administer end-of-life treatment or arrange for loved ones to say goodbye.
Meanwhile the employees have even moved into caravans nearby to ensure they are able to provide help at short notice.
Following an inspection by CQC, the care home regulator, the home was found to have been doing everything it could to prevent the spread of the virus.
Diane Vale, the care home’s manager, said the home ‘didn’t have anybody who wasn’t positive’.
The home had plenty of checks in place to deal with an outbreak, but tragically the rapid spread left Diane and her team powerless.
Advertisement
‘Every death is a tragedy and it would be highly disrespectful if lessons were not learned at every level. Similarly, every death needs to be seen in context.
‘We do not believe that this data is a reflection of quality and I would like to pay tribute to all the frontline staff who have done a heroic job and it must not be forgotten that many of them lost their lives too.’
The CQC added the number of deaths in individual homes is not a reflection on institutions’ care standards.
Kate Terroni, CQC’s chief inspector of adult social care, said: ‘In considering this data it is important to remember that every number represents a life lost — and families, friends and those who cared for them who are having to face the sadness and consequences of their death.
‘We are grateful for the time that families who lost their loved ones during the pandemic have spent meeting with us and the personal experiences they have shared
‘We ask for consideration and respect to be shown to people living in care homes, to families who have been affected, and to the staff who have done everything they could, in incredibly difficult circumstances, to look after those in their care.’
MPs last year claimed homes were ‘thrown to the wolves’ during the pandemic and the Government’s actions were ‘at times negligent’.
The social care crisis was exacerbated further by a series of ‘reckless’ and ‘appalling’ policy errors, according to a damning Commons public accounts committee report.
Advising hospitals to discharge thousands of patients into care homes without knowing if they had coronavirus was an example of this, they said.
At least 25,000 patients were moved from hospitals to care homes between March 17 and April 15, when there was a lack of rigorous testing.
Estimates suggest around two-thirds weren’t swabbed.
The National Audit Office, which reviewed the scandal, said hospitals were told on March 17 to ‘discharge urgently’ all in-patients medically fit to leave in order to increase capacity’.
Care home bosses also warned that their staff didn’t have enough access to personal protective equipment such as gloves, masks and aprons.
The industry also warned of a lack of testing at the start of the crisis, when swabs were rationed because of a lack of supply.
Officials also asked care homes to take Covid patients again in the winter.
Under the scheme, designed to free up hospital beds and protect the NHS in the second wave, Covid-secure homes which passed inspection were asked to house infected patients.
WHAT WENT WRONG FOR CARE HOMES? A TIMELINE OF FAILINGS
FEBRUARY – SAGE scientists warned Government ‘very early on’ about the risk to care homes
Britain’s chief scientific adviser, Sir Patrick Vallance, revealed in April that he and other senior scientists warned politicians ‘very early on’ about the risk Covid posed to care homes.
He said: ‘So very early on we looked at a number of topics, we looked at nosocomial infection very early on, that’s the spread in hospitals, and we flagged that as something that the NHS needed to think about.
‘We flagged the fact that we thought care homes would be an important area to look at, and we flagged things like vaccine development and so on. So we try to take a longer term view of things as well as dealing with the urgent and immediate areas.’
The SAGE committee met for the first time on January 22, suggesting ‘very early on’ in its discussions was likely the end of January or the beginning of February.
MARCH – Hospital patients discharged to homes without tests
In March and April at least 25,000 people were discharged from NHS hospitals into care homes without getting tested for coronavirus, a report by the National Audit Office found.
This move came at the peak of the outbreak and has been blamed for ‘seeding’ Covid-19 outbreaks in the homes which later became impossible to control.
NHS England issued an order to its hospitals to free up as many beds as they could, and later sent out joint guidance with the Department of Health saying that patients did not need to be tested beforehand.
Chair of the public accounts committee and a Labour MP in London, Meg Hillier, said: ‘Residents and staff were an afterthought yet again: out of sight and out of mind, with devastating consequences.’
MARCH – Public Health England advice still did not raise alarm about care home risk and allowed visits
An early key error in the handling of the crisis, social care consultant Melanie Henwood told the Mail on Sunday, was advice issued by Public Health England (PHE) on February 25 that it remained ‘very unlikely’ people in care homes would become infected as there was ‘currently no transmission of Covid-19 in the UK’.
Yet a fortnight earlier the UK Government’s Scientific Pandemic Influenza Modelling committee had concluded: ‘It is a realistic probability that there is already sustained transmission in the UK, or that it will become established in the coming weeks.’
On March 13, PHE advice for care homes changed ‘asking no one to visit who has suspected Covid-19 or is generally unwell’ – but visits were still allowed.
Three days later, Mr Johnson said: ‘Absolutely, we don’t want to see people unnecessarily visiting care homes.’
MARCH/APRIL – Testing not readily available to care home residents
In March and April coronavirus swab tests — to see who currently has the disease — were rationed and not available to all care home residents suspected of having Covid.
Government policy dictated that a sample of residents would be tested if one showed symptoms, then an outbreak would be declared and anyone else with symptoms presumed to be infected without a test.
The Department of Health has been in control of who gets Covid-19 tests and when, based on UK testing capacity.
MARCH/APRIL – Bosses warned homes didn’t have enough PPE
Care home bosses were furious in March and April – now known to have been the peak of the UK’s epidemic – that their staff didn’t have enough access to personal protective equipment such as gloves, masks and aprons.
A letter sent from the Association of Directors of Adult Social Services (Adass) to the Department of Health saw the care chiefs accuse a senior figure at the Department of overseeing a ‘shambolic response’.
Adass said it was facing ‘confusion’ and additional work as a result of mixed messaging put out by the Government.
It said the situation around PPE, which was by then mandatory for all healthcare workers, was ‘shambolic’ and that deliveries had been ‘paltry’ or ‘haphazard’.
A shortage of PPE has been a consistent issue from staff in care homes since the pandemic began, and the union Unison revealed at the beginning of May that it had already received 3,600 reports about inadequate access to PPE from workers in the sector.
APRIL – Care home deaths left out of official fatality count
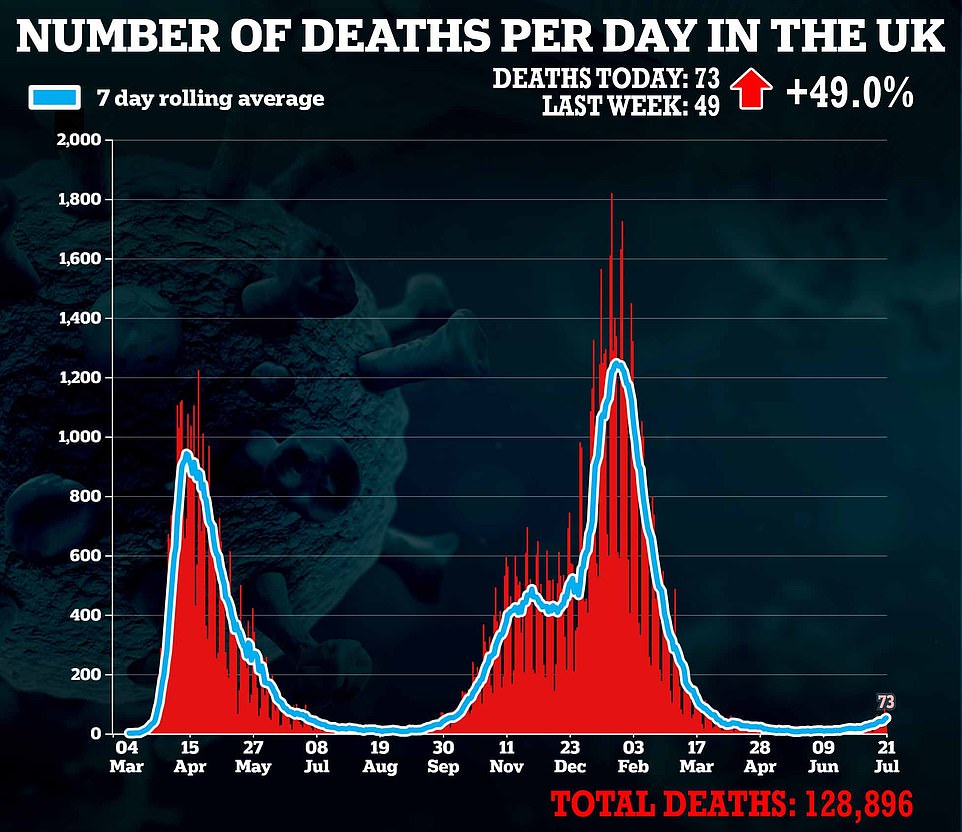
The Department of Health refused to include people who had died outside of hospitals in its official daily death count until April 29, three weeks after deaths had peaked in the UK.
It started to include the ‘all settings’ measure from that date and added on 3,811 previously uncounted Covid-19 deaths on the first day.
Advertisement
Source link : https://www.dailymail.co.uk/news/article-9810561/Covid-19-UK-150-care-homes-England-suffered-20-coronavirus-deaths.html











