Sexually transmitted infection rates dropped by 32 per cent in England last year, official figures show.
Some 317,901 people tested positive for an STI in 2020, down from 467,096 in 2019, data from Public Health England revealed.
Rates of chlamydia — the country’s most common STI — dropped by 29 per cent, while those with gonorrhoea dropped by 20 per cent.
The biggest decrease was in cases of genital warts, which fell 46 per cent, and herpes which was down 40 per cent.
PHE said Covid rules led to ‘changes in behaviour’ which influenced the decline, such as having less casual sex, as well as reduced testing and diagnoses.
Now that restrictions have eased across the country, the agency warned people to be careful not to ‘swap social distancing for an STI’.
Various Covid rules imposed from last March meant socialising indoors with anyone from a different household was a breach of restrictions.
And legislation reduced last June meant anyone having sex with someone they did not live with could be prosecuted.
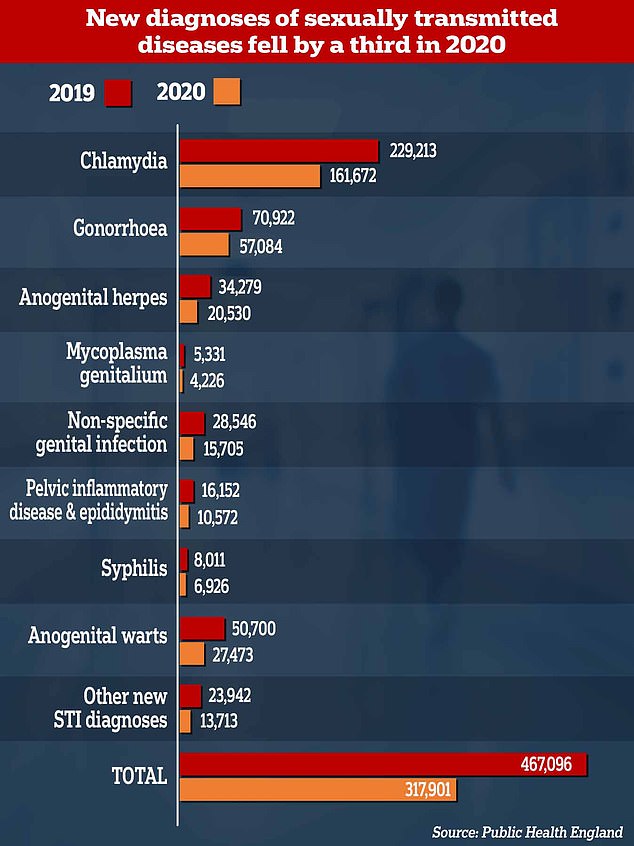
Chlamydia remained the most common STI in England, with 161,672 people being diagnosed with it, down from 229,213 in 2019. Meanwhile, 57,084 people tested positive for gonorrhoea, there were 27,473 diagnoses of genital warts and 20,530 found out they had herpes — the next most common STIs. The biggest drop was seen in diagnosing STIs that require an in-person assessment, such as genital warts (46 per cent) and herpes (40 per cent)
Some 317,901 people tested positive for an STI in 2020, down from 467,096 in 2019, data from Public Health England revealed. This was due to changes in behaviour during Covid lockdowns and less people getting tested for STIs, PHE said
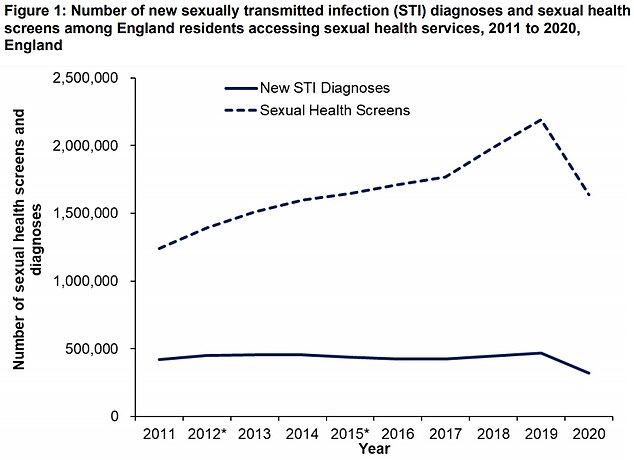
Healthcare staff diagnosed more than 300,000 STIs in 2020, after scaling up testing accessed through phone and online appointments during national and regional lockdowns.
But consultations fell by 10 per cent overall compared to 2019 and face-to-face appointments dropped by 35 per cent.
Which STIs had the biggest drop in diagnoses in 2020?
Anogenital warts: -46 per cent
Non-specific genital infection: -45 per cent
Other new STI diagnoses: -43 per cent
Anogenital herpes: -40 per cent
Pelvic inflammatory disease and epididymitis: -35 per cent
Chlamydia: -29 per cent
Mycoplasma genitalium: -21 per cent
Gonorrhoea: -20 per cent
Syphilis: -14 per cent
Advertisement
Additionally, 25 per cent less tests for chlamydia, gonorrhoea, syphilis and HIV were carried out.
Chlamydia remained the most common STI in England, with 161,672 people being diagnosed with it, down from 229,213 in 2019.
But despite the 29 per cent drop, PHE warned the rate of people testing positive for chlamydia remained stable at 9.8 per cent.
This suggests there was ongoing transmission despite restrictions, it added.
Meanwhile, 57,084 people tested positive for gonorrhoea, there were 27,473 diagnoses of genital warts and 20,530 found out they had herpes — the next most common STIs.
The biggest drop was seen in diagnosing STIs that require an in-person assessment, such as genital warts (46 per cent) and herpes (40 per cent).
Conditions that can be diagnosed through self-testing saw a smaller than average drop in being diagnosed, such as chlamydia (29 per cent) and gonorrhoea (20 per cent).
The data did not include HIV diagnoses, which will be published later this year.
Despite the drops in testing last year, the high levels of STI diagnoses is ‘clear evidence’ that there was sustained STI transmission, PHE said.
This is supported by community surveys, which suggest that despite less people meeting new sexual partners in 2020 compared to previous years, a ‘substantial proportion’ were still at-risk, such as by having condomless sex with new partners, it said.
People aged 15 to 24, black people and those who are gay, bisexual or are men who have sex with men were the most likely to be diagnosed with an STI. These trends are the same as in previous years, PHE said.
Those who have an STI often do not experience symptoms, meaning they can be infected and pass it on to others without knowing.
Condoms can be used to prevent the spread of some STIs.
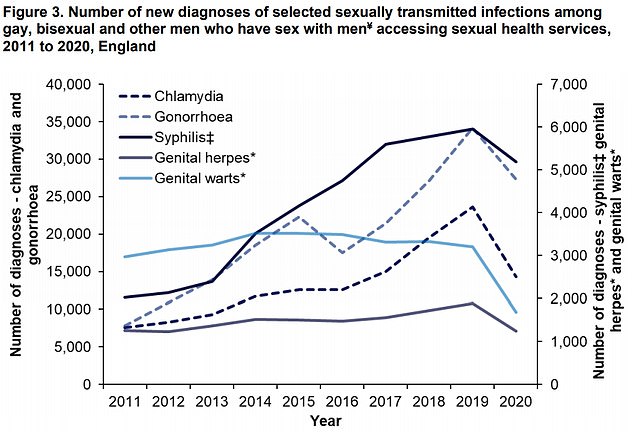
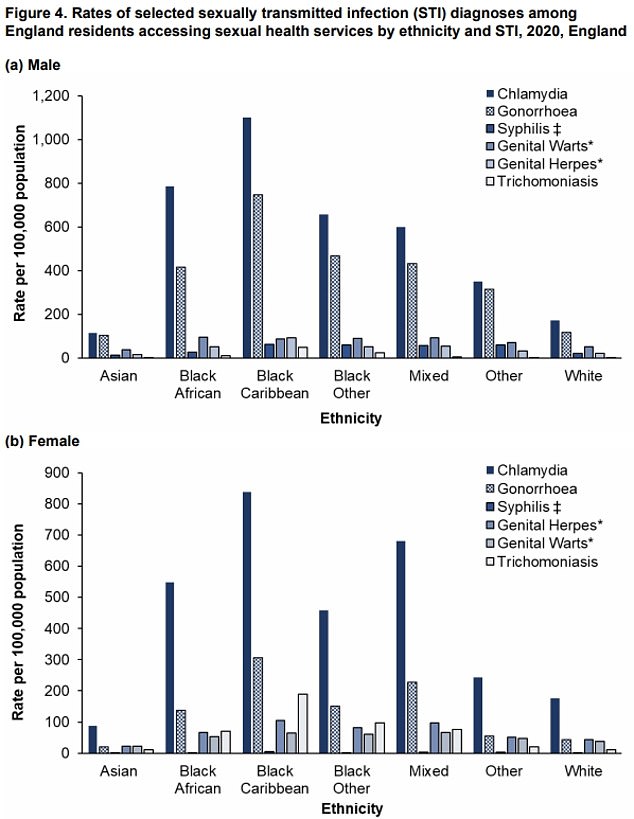
People aged 15 to 24, black people and those who are gay, bisexual or are men who have sex with men were the most likely to be diagnosed with an STI. These trends are the same as in previous years, PHE said
PHE urged those having sex without using a condom with new or casual partners to get tested regularly, even if not experiencing symptoms.
People can get tested at local sexual health services, or order free online tests to use themselves at home, which they can post to a lab for testing and receive a test of their results.
Dr Katy Sinka, head of the sexually-transmitted infections section at PHE, said: ‘No-one wants to swap social distancing for an STI and as we enjoy the fact that national Covid-19 restrictions have lifted, it’s important that we continue to look after our sexual health and wellbeing.
‘If you are having sex with new or casual partners, use a condom and get tested – STIs can pose serious consequences to your own health and that of your current or future sexual partners.’
Debbie Laycock, head of policy at Terrence Higgins Trust, said: ‘2020 was not a normal year and that was certainly true for many people’s sex and relationships.’
The drop in STIs is ‘one unexpected good news story from the coronavirus pandemic’, she said.
‘But the question for government is will this once in a lifetime opportunity be capitalised on or squandered as rates quickly creep up again,’ Ms Laycock said.
She added: ‘This 32 per cent drop reflects a year when all of our behaviour was changed and when health services – including sexual health services – were severely impacted.
‘But we applaud the flexibility of sexual health services and community organisations in responding quickly to such an unprecedented challenge as Covid with just a 10 per cent decrease in consultations at clinics compared to 2019 and an increase in the roll out of online STI testing.
‘Online testing must now be maintained and expanded with greater consistency across the country.’
The data ‘clearly shows’ the drop in STI diagnoses is primarily a result of a decline in testing, Covid-related behaviour change – with many people having less sex during much of the year – rather than Government action to tackle ‘consistently high rates’, Ms Laycock added.
Councillor David Fothergill, chair of the Local Government Association’s Community Wellbeing Board, said there could be a surge in demand as ‘life returns to normal’.
He warned that despite the decline in rates, there is likely some infected people who did not seek advice during lockdown restrictions.
Investing in councils’ public health budget would ‘help relieve pressure’, he added.
Source link : https://www.dailymail.co.uk/news/article-9965545/STI-rates-plunged-year-Covid-lockdowns-forced-changes-behaviour.html











