Henry Scowcroft’s beautiful book Cross Everything may be the most heartbreaking medical memoir you’ll read.
Henry, 43, a science writer at Cancer Research UK (CRUK) for 17 years, describes precisely how cancer evolves, adapts and survives, fighting the body’s own defences for supremacy.
But at the centre of this searingly painful book is his much-loved, ‘compassionate, hilarious, open-hearted’ fiancée Zarah, who died of bladder cancer aged 37 on October 23, 2016, just nine months to the day after she was first diagnosed.
‘Even though I talked and wrote about cancer every day, I realised when Zarah was diagnosed that I knew nothing about living with it,’ he says.
‘I felt as everyone does, desperate to help in any way I could.’

Zarah had just started a job she loved and the pair were thinking about moving house. Her only health niggle was the urinary tract infections (UTIs) she’d suffered since her teens, which flared up once a year. She is pictured above with Henry Scowcroft
For Henry, that meant talking to everyone he knew in the research world, ‘leaving no stone unturned’ in the hunt for a drug or treatment they could try in the race to buy Zarah more precious time.
Henry and Zarah, a digital marketing manager for M&S, were both in the same group of outgoing friends and got together at a music festival in 2010.
‘We were in our 30s, so life was simple, fun and happy,’ says Henry. ‘We were best friends as well as lovers; we did everything together.’
Zarah had just started a job she loved and the pair were thinking about moving house. Her only health niggle was the urinary tract infections (UTIs) she’d suffered since her teens, which flared up once a year.
‘She had pain when she went to pee, mild fever and sometimes backache,’ says Henry. ‘It was annoying but it wasn’t a major part of her life.’
In 2010, Zarah had been given a cystoscopy — where a small tube with a lens is fed into the bladder — but other than a small area of inflammation, everything looked normal. Her GP continued to prescribe low-dose antibiotics, which she took daily to keep infections at bay.
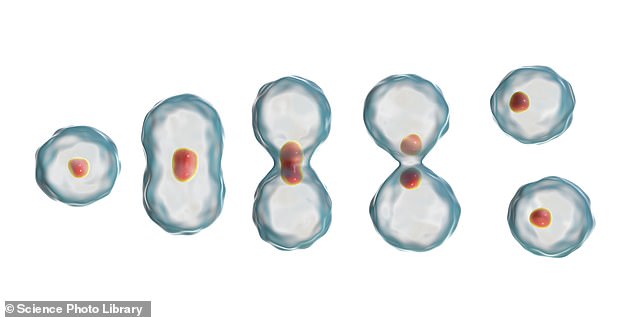
‘We start where it always begins — with a single cell. The scene? It could be anywhere in the body, but in my late partner Zarah Harrison it was the interior lining of her bladder’, writes Henry Scowcroft. Cells are seen dividing above
So when Zarah started to suffer the familiar symptoms in January 2016, she assumed it was another infection.
But when she passed a large blood clot, her GP sent her to A&E and she was kept in overnight while specialists examined the results of a CT scan.
‘I’ll know it’s serious if I see a bunch of consultants racing down the corridor towards me with their coats billowing,’ Zarah quipped over the phone to Henry.
That was exactly what she saw next. The scan had revealed a mass in her bladder. The couple were told Zarah would need surgery to remove it for analysis.
A nightmare that starts with one rogue cell
By Henry Scowcroft
We start where it always begins — with a single cell. The scene? It could be anywhere in the body, but in my late partner Zarah Harrison it was the interior lining of her bladder.
Imagine if we could zoom in. Nestled alongside millions of identical neighbours in this delicate layer is a cell: a tiny, unremarkable, disc-shaped bubble of gelatinous life just micrometres in diameter.
From the outside, all is quiet, the silence belying a hum of invisible activity as the cell’s energy is devoted, as it has been for the past few weeks, to replicating what would be — if stretched out — nearly two metres of DNA, the cell’s blueprint, packed into the nucleus at its centre, with near-perfect fidelity, checking, double-checking, preparing, recharging.
Suddenly, inside the cell, things spring into life as it starts once more to divide, each step tightly co-ordinated and refined by evolution over billions of years. The delicate membrane surrounding its nucleus dissolves, while simultaneously the DNA contained within begins slowly to condense into 46 chromosomes, each subdivided into genes, containing two duplicates of a vital chunk of genetic information — thousands of genes held in a few nanometres; the book of life, in duplicate.
From nowhere, a rigid scaffold emerges, stretching out across the cell’s interior, forming a series of ghostly, skeletal tracks that run from one end of the cell to the other. This causes the disc-shaped cell to swell into a sphere.
Then, like a regiment of soldiers lining up in formation, all 46 condensed DNA chromosomes start to assemble across the cell’s diameter, perpendicular to the skeleton, each somehow knowing its precise place in the proceedings.
So far, so good — and with everything in place, the real action begins. The skeleton expands, forcing the cell apart, tugging one half of each chromosome pair in an opposite direction.
The balloon inflates further and yet more newly formed scaffolding (this time radiating out from the centre to the cell’s outer membrane) pulls inward, constricting the membrane around the balloon’s centre as if it were being cut in half by a belt strapped around its middle. Slowly at first, then increasingly rapidly, the membrane draws in further while the chromosomes segregate into two matching groups that are safely separated, one in each ‘half’ of the balloon.
Then the belt tightens to pinch the cell clean in two. The mother cell has a new daughter. But something is amiss. Somehow, at some point during the replication and the wrenching violence of the cell division, a defect has become embedded in its DNA that will sow the seeds of a future tragedy.
Years pass. Deep in the lining of the bladder, the mother cell has been robotically carrying out its duty, division after division, daughter after daughter, its lifetime progeny now numbering millions.
And all this time, despite appearing outwardly normal, this particular mother cell and all its progeny have carried that tiny defect in their DNA, in the process losing the instructions to assemble a particular protein that governs whether the cell that contains it should divide or not (if it’s faulty).
Luckily, the chromosome carries a back-up to this control gene, on its identical twin. But today, again by awful coincidence, something inexplicably jams, twisting and breaking the DNA strands as the cell replication process begins again. Immediately, the replication machine seizes up and the working copy of the gene on that twin chromosome is destroyed.
Molecular alarms ring out. Sensing the error, the cell finds the chromosome’s faulty sibling and uses it as a template to try to patch up the fractured DNA.
In doing so, it embeds the defect for ever into the cell’s genome. A vital cog in the cell’s control system has just been irretrievably overwritten in error. From now on, whenever the mother cell uses this garbled template, each of her daughters will bear this deranged, faulty cellular software, and each is now free to grow and divide unchecked. Nature’s brake cable has been decisively cut. And each cell exponentially becomes two, becomes four, becomes eight, becomes 16 . . . and gradually, in Zarah’s case, from this small patch of the bladder’s lining emerges an ever-expanding clump of millions of proliferating, impatient, unruly cells — mere millimetres in diameter but massive in consequences.
As each of these rogue cells gears up for a new round of division, yet more catastrophic genetic events occur as they try to replicate their jumbled, muddled chromosomes in slapdash, make-do fashion. Frequently, these catastrophes are just too much for the resulting progeny to bear: the cells self-destruct, shedding debris far and wide. Yet others survive to accumulate new errors — and new powers.
Sensing something amiss, nearby immune cells mobilise to try to contain the damage, amassing at the edges of the anomaly.
Gently, carefully, the immune cells extend their tiny molecular sensors, stroking the surface of each rogue cell, looking for outward signs of aberration. Alas, despite their odd behaviour, their scrambled DNA and their impatient, rapid growth, as far as the immune system is concerned, each of the rogue cells still ‘feels’ just like every other cell in the bladder.
Nothing to see here. Move along. And so, ignored by the immune system, the mass continues to grow unhindered, now just a few steps away from transforming into cancer.
Advertisement
‘Although we knew a mass meant it might be cancer, at that point we were very hopeful,’ says Henry. ‘I thought: we’ll go through something horrible and come out the other side.’
Henry immediately called CRUK’s chief clinician, who recommended Zarah should ask her GP for a referral to Professor John Kelly, a consultant urological surgeon at University College London Hospital (UCLH).
‘We both felt relieved to know things were in hand, with the top experts on the case,’ says Henry.
But surgery a week later confirmed it was advanced cancer that was growing into her pelvis. Henry describes feeling numb with shock. He held himself together until Zarah dropped off to sleep, then returned to their empty flat and cried.
About 10,000 new cases of bladder cancer are diagnosed in the UK every year and while most patients are over 60, any age can be affected. The most common symptoms are similar to those of UTIs — needing to pee more regularly and blood in your urine. Smoking is thought to be a factor in half of all bladder cancer cases — but Zarah was not a smoker. The disease is curable if caught early, but the problem is that recurrent UTIs mask the symptoms.
‘Even with my background, where I discussed cancer every day, the thought never crossed my mind that Zarah’s UTIs might be connected,’ says Henry.
Results of tumour tissue analysis a week later showed it was muscle-invasive transitional cell bladder cancer, the most common type. It was fast-growing — and then came the hammer blow: it was stage 4, meaning it had already spread to the point where it couldn’t be cured, only treated with chemotherapy to buy more time — how much, no one knew.
They left the consultant’s room ashen-faced and shaking, tears streaking down Zarah’s face; Henry holding her hand tightly, determined to do everything he could to help.
In March, Zarah started chemotherapy, which, says Henry, she ‘handled like a trooper’.
At the same time, he enlisted the help of a friend, Professor Charles Swanton, a clinical scientist at the Francis Crick Institute in King’s Cross, who was part of a team trying to find clues in cancer’s faulty DNA for better treatments. Professor Swanton offered to take samples from Zarah’s tumour and perform sophisticated DNA sequencing to find the gene mutations driving her cancer. The hope was that experimental drugs could be found — there were none. ‘But at the time it felt as if someone had thrown us a lifeline,’ says Henry.
The most promising option now was for Zarah to get onto a clinical trial of one of the new immunotherapy drugs, which harness the body’s own immune system to fight cancer. ‘We were just so incredibly, tearfully grateful to still have options,’ says Henry. ‘What we didn’t know was that the tumour was marshalling its forces and getting ready to come roaring back.’
For as soon as the chemotherapy ended in July, Zarah’s condition went downhill very quickly. ‘Why that happened is one of the great mysteries of cancer,’ says Henry. ‘Chemotherapy is the best treatment we have — it can put a lid on the disease for many patients; but then the disease can somehow become resistant.
‘In Zarah’s case, it seemed to kill all the sensitive cancer cells and the dominant ones were left behind to proliferate.’ And there was more bad news. Further analysis of her tumour by the Francis Crick team showed her immune system was misfiring.
‘As with so many patients, her immune system mistook her cancer for a ‘healing wound’,’ explains Henry. ‘And instead of attacking, it switched itself off.’ (See book extract, right.)
Scans showed Zarah’s tumour, which she’d nicknamed ‘Tina’, was growing again and had spread to her liver and lymph nodes. She was given more chemotherapy and lost her hair. She also developed painful lymphoedema in her legs — when lymph nodes are blocked by cancer or removed by surgery, it can cause a build-up of fluid.
Even then, Zarah was stoic. ‘There was always a sense there was nothing we couldn’t take,’ Henry says.
It wasn’t until October, two months after her chemo finished, that Zarah was accepted onto an immunotherapy drug trial. Both she and Henry were filled with hope. ‘Everyone who participates in a trial thinks: ‘I might be the one who is cured’; we were no different.’
Zarah had her first dose but ‘although she was still able to hold a conversation, she was drowsy a lot of the time’, Henry recalls. ‘It was obvious ‘Tina’ was moving through her body fast.’ Zarah’s oncologist suggested she move to a hospice, yet Henry says: ‘The penny didn’t drop at all. I thought we were waiting for the drugs to work.’
Even then, although Zarah slept a lot, there were moments she was fully herself. Once, Henry and Zarah’s mother, Florence, wheeled her into the garden to share a can of gin and tonic. ‘I don’t think she’ll want it,’ Florence said.
Quick as a flash, Zarah’s arm shot out and grabbed it. ‘That was so Zarah,’ says Henry. ‘She’d never pass up a gin and tonic. She had all these hilarious stories of daft things she’d done. We added this one to our canon of Zarah stories which still make us laugh and cry now.’
Twenty four hours later, ‘stoic, brave’ Zarah died with Henry’s arms wrapped around her. He recalls: ‘I’d been so focused on keeping us both going, I didn’t see the end coming.’ Although for, Zarah, all the hope came to nothing, the prospect of hope was everything. ‘Knowing immunotherapy was an option, knowing there was a trial, got us through on a day-to-day basis,’ says Henry.
‘And importantly, the study of Zarah’s samples to try to find cancer’s weak spots will help move treatment on another micro-step for other patients.’
Scientists have known for over a decade that tumours shed their DNA into their surroundings, potentially allowing cancer’s progress to be tracked using blood or urine samples. These ‘liquid biopsies’ are tantalisingly close to routine use and mean cancer progression could be visible in a blood or urine sample before being seen on a scan.
After Zarah died, Henry persuaded resear-chers to analyse her samples, stored in UCLH’s laboratories, as part of a nationwide research programme. Bur-eaucratic and logistical hurdles, coupled with Covid, meant the results didn’t come through until mid-2020, four years after Zarah died.
But they confirmed the promise of this technology. The amount of cancer DNA in Zarah’s blood showed her tumour had been on the march far earlier than had been visible on scans.
‘The potential offered by liquid biopsies is huge,’ says Henry, ‘because doctors will no longer have to wait until tumours are big enough to see on a scan to act — this is where we are losing people.’
A year after Zarah’s death, Henry went back to work for CRUK. He is also patient editor for The BMJ. But the role he is most proud of is being patient representative for the National Cancer Research Institute bladder and kidney research steering group.
He has gathered the ‘lab folks’ who run university research programmes and the ‘clinical folks’ — NHS oncologists who treat patients every day — around a table in hope that the different skills sets will lead to some top-notch ideas for research he can then take to funding bodies.
He would love to eradicate for ever what cancer patients call ‘scan-xiety’, when you ‘cross everything’ waiting to see what the next scan will reveal.
Most of all, he wants to inspire the next generation of researchers to work in bladder cancer by passing on something of Zarah’s remarkable spirit.
Cross Everything, by Henry Scowcroft, is published by Bloomsbury at £18.99. © Henry Scowcroft 2021.
To order a copy for £16.71 (offer valid to 28/2/21; UK P&P free on orders over £20), visit www.mailshop.co.uk/books or call 020 3308 9193.
actionbladdercanceruk.org; fightbladdercancer.org
Source link : https://www.dailymail.co.uk/health/article-9288229/Veteran-Britains-leading-cancer-charity-releases-new-book-partners-terminal-diagnosis.html











