Dr. Bill Frist 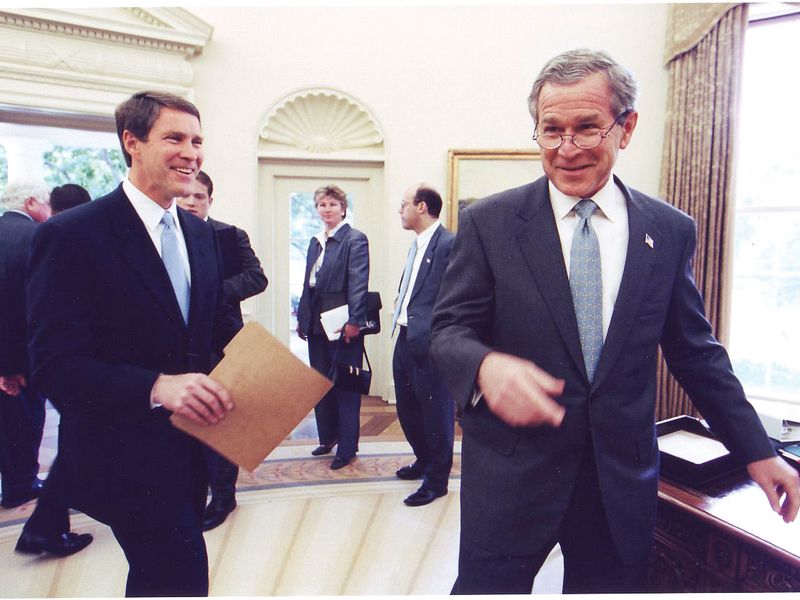
Dr. Bill Frist, a heart and lung transplant surgeon, served as a U.S. senator from Tennessee from 1995 to 2007, including serving as Senate majority leader from 2003 to 2007. Here he’s pictured during a meeting with President George W. Bush.
When we look back on 2020, undoubtedly a definitive period in our history, perhaps one of our greatest lessons will be the near-miraculous power of partnerships and collaboration.
When we harnessed the greatest scientific minds of the world from both academia and companies and paired them with the financial backing and influence of the most powerful governments, we advanced light-years ahead in vaccine research, viral treatments and diagnostics.
Of course this is not the first time we’ve seen partnerships yield success. Indeed, I believe collaboration and cross-pollination have proven central to moving our healthcare system forward. Let me give three examples.
PEPFAR The first is the epochal program that former President George W. Bush considers among his most impactful legacies, but one that is little known to the typical American.
PEPFAR, the President’s Emergency Plan for AIDS Relief, was enacted in 2003. I was then Senate Majority Leader and had provided on-the-ground medical care of patients with AIDS in sub-Saharan Africa.
I worked with President Bush’s team to write the bill and get it across the finish line, and then the magic happened. At the time of passage, AIDS was killing 3 million people each year globally and had escalated to a global pandemic. Eighteen years later, PEPFAR has saved over 20 million lives, allowed 2.8 million babies to be born HIV-free, and trained 290,000 health workers.
The U.S. began by engaging with 14 nations (the total is now over 50) that were debilitated by the virus. Over time, lives and society were restored.
Public-private partnerships were part of the strategy, and central to results. As Jeffrey Sturchio and Gary Cohen wrote in their 2012 Health Affairs piece, engaging the private sector to further the mission of addressing the global AIDS pandemic was written into the bill.
For instance, PEPFAR’s Supply Chain Management System partnered with a network of private sector companies—led by shipping and logistics provider UPS—as well as academic and not-for-profit organizations to tackle the herculean task of delivering antiretroviral medications and related supplies to remote parts of sub-Saharan Africa.
The parallels are striking as today, even in the U.S., we see the challenges in distributing a vaccine with stringent cold-storage requirements. Imagine planning logistics for areas where electricity, refrigeration and running water may not be easily accessible. It was to overcome barriers like this that PEPFAR drew on private sector experience. In time, infrastructure was built, supply chain management systems were put in place, and antiretroviral treatments were dispersed by the thousands, then millions.
As another study of PEPFAR’s effectiveness noted, “As of the end of 2010, there were 6.6 million people who initiated antiretroviral treatments in low- and middle-income countries, compared with only 400,000 in 2003.” Today, over 17 million have received lifesaving therapy. And many of those same procurement processes, disease surveillance systems and public health foundations laid in PEPFAR have been critical to developing nations as they tackle COVID-19 today.
With the support of PEPFAR and its partners, these nations began to prosper. The U.S. benefited as well from improved trade, improved diplomatic relations, reduced threats in foreign nations that could be destabilized by terrorism, and improved perceptions of the U.S. throughout the world.
With PEPFAR’s backing, new partnerships continue to form, such as the Go Further Partnership with Merck, which began in 2018 and aims to reduce new cervical cancer cases by 95% among the estimated 7.1 million women living with HIV who reside in the partnership’s 12 African countries. As of September 2020, the Go Further Partnership has supported over 1.5 million cervical cancer screenings.
Medicare Advantage A second example that really resonates for me is Medicare’s partnership with the private sector through Medicare Advantage. We overhauled MA in Congress in 2003, at the time a tiny program known as Medicare+Choice.
We took a number of steps to incentivize private insurers’ participation, which had been declining. I vividly remember my late-night, one-on-one, planning and negotiating meetings with the late Sen. Edward Kennedy, who, despite his concerns with the bill, worked tirelessly with me and my staff to make it better for patients.
While more generous reimbursement rates were needed initially to bring insurers to the table, the cost of the average Medicare Advantage patient is nearly on par (or below depending on the analysis) with the traditional Medicare patient. Even better, we’ve seen Medicare Advantage foster innovation and flexibility for seniors’ care to address substantial health problems further upstream—getting to the non-medical social determinants of health.
When Brad Smith and I were working to bring community-based palliative care into the home through Aspire Health, it was through Advantage plans that we were first able to expand access to this widely needed but underutilized new form of care for those with serious chronic illness.
I’ve also seen Advantage plans allow some of our nation’s brightest healthcare entrepreneurs—like Ed and Todd Park at Devoted Health and Rushika Fernandopulle at Iora Health—bring their own innovative care models into being.
Today, 39% of all Medicare beneficiaries—24.1 million people out of 62 million Medicare beneficiaries overall—are enrolled in Advantage plans, with projections it will cover 51% of beneficiaries by 2030.
I am convinced the Medicare Advantage program will continue to be on the forefront of bringing the best, most modern healthcare delivery models to seniors now and in the future. That’s what effective partnerships can accomplish.
Creativity in Tennessee Finally, I turn to my home state of Tennessee, which has been a national leader in harnessing the best of private sector innovation to provide quality care to our Medicaid population. Tennessee was the first state to transfer all of its Medicaid beneficiaries to managed-care organizations, which we did in 1994. I had been chair of the Tennessee Medicaid Task Force, comprised of representative public and private sector individuals, which laid the groundwork in 1993.
Through a Section 1115 waiver, we were able to add unique flexibility to our Medicaid program and try cutting-edge ideas without constantly having to seek federal approval, which can take months or years. Indeed, we were out front in integrating physical and behavioral health services, implementing a more coordinated approach to caring for Medicare/Medicaid dual-eligible patients, and providing cost-effective alternatives to care that often focused on social determinants like home-delivered meals and making home modifications to improve safety.
Of course, this transition was not without its challenges and setbacks in the early years of the program, and that is why it’s so important that government provide the necessary incentives and guardrails to induce both investment and creativity and ensure patient quality and safety, and do our fiduciary duty to taxpayers. According to a 2020 Pew Charitable Trusts study, from 2000 to 2017 TennCare (our state’s Medicaid program) outperformed all other states in limiting the growth of the state budget share going to support Medicaid. And annual member surveys for TennCare show a member satisfaction rate of 94%, resting above 90% for more than a decade.
When government invites the energy, inventiveness and the access to capital of the private sector, giving it the structure to address issues of equity and market failures and provide needed solutions, we can solve some of our nation’s, and the world’s, most pressing and often seemingly insurmountable problems.
Our healthcare system today is in need of comprehensive overhaul, and a blunt, single-bullet fix like government-run healthcare will not be the solution. We are at our best when we bring new partners, new people, and new ideas to the table. I know we will continue to bring down barriers in the years to come to foster collaboration across governments, academia, private industry and not-for-profits, in all sectors of our economy.
Source link : https://www.modernhealthcare.com/opinion-editorial/transformative-power-public-private-partnerships











