
4 Useful Items You Should Place Under Your Bed
4 Smart Things to Store Under Your Bed

4 Smart Things to Store Under Your Bed

What Lemon Water Can Do for Your Body: 17 Benefits Worth Knowing

Flight Attendants Reveal Why They Sit on Their Hands Before Takeoff

A Simple Trick to Deal with Peeling Walls and Mold Stains Without Professional Help

A Simple Trick Before Steaming Sweet Potatoes That Chefs Often Use
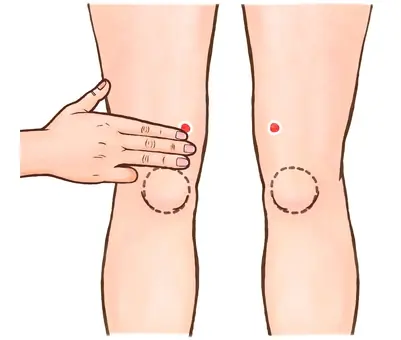
Two Pressure Points Behind Your Knees You Should Know

When Should You Avoid Bananas? 2 Situations to Know

7 Incredible Benefits of Kakadu Plum for Your Health

No matter how expensive they are, you should never eat these foods after they have been left overnight. Don’t gamble with your health!

The Real Advantages of Starting Your Day with Coffee

12 Health Benefits of Starting Your Day with Banana and Avocado for 30 Days

You can grow 8 types of snake-repelling plants 👇👇👇

The Surprising Reason Kni.ves Sometimes Have a Small Hole

According to a recent study published in The British Journal of Nutrition (UK), eating about 100g of watercress per day can prevent breast cancer and many other cancers.

Do your best to be the parent your children deserve

The Ideal Battery Percentage to Charge Your Phone for Longer Lifespan

Which Is Better When Buying Garlic: White or Purple Skin?

Worried About Snakes Around Your Home? Here Are 5 Plants People Often Grow to Help Keep Them Away

A 50-Year-Old Man Died After Eating Leftovers From the Fridge: 5 Foods You Should Never Keep Overnight
Waking Up With a Headache? Here Are the Signs That May Point to Stroke Risk