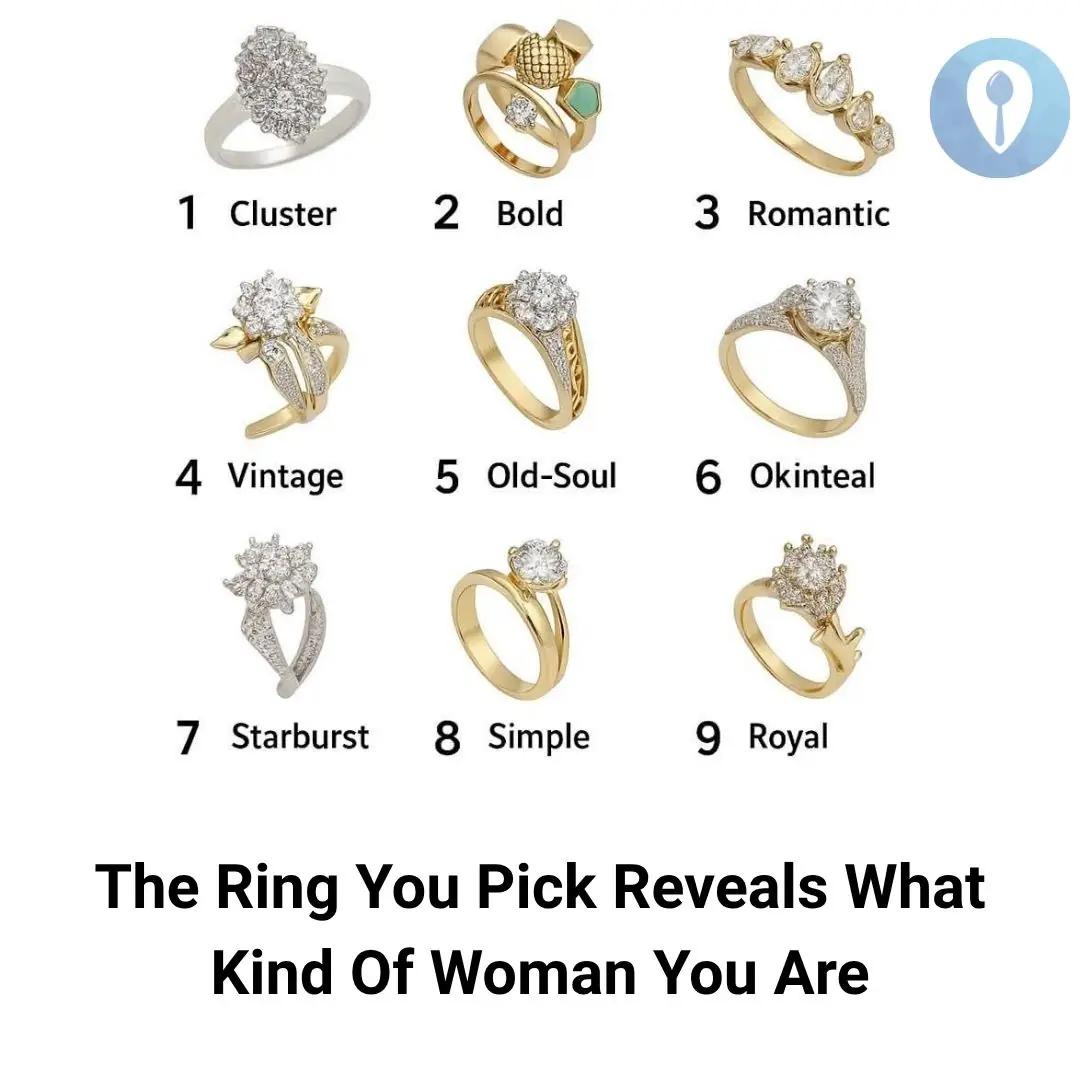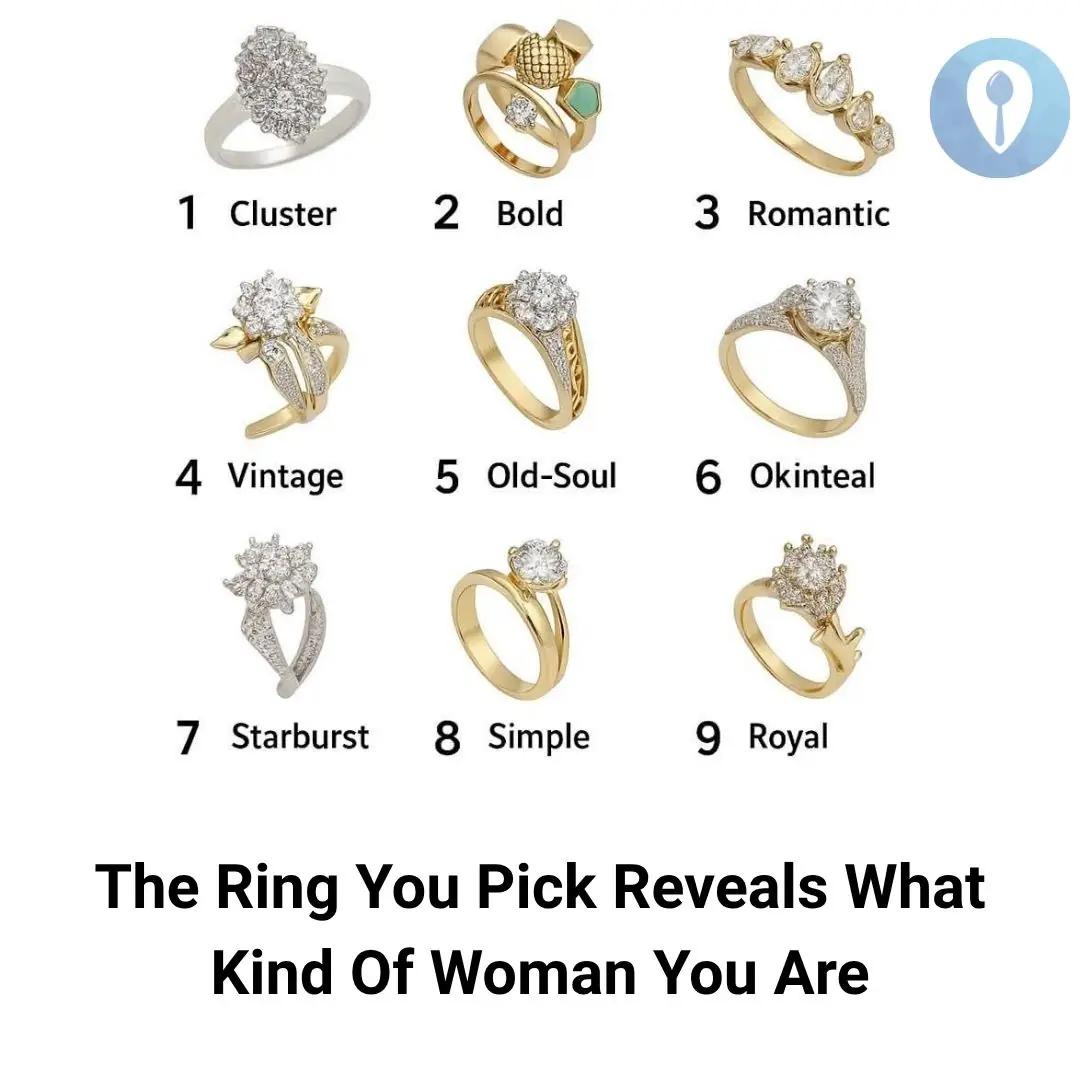
Pick a Ring and Discover What It Says About the Woman You Are
Relax 05/11/2025 12:02

Answer: This is a toad fan. The reason it is called a toad fan is because the fan body consists of 2 pieces of plastic placed together, covering the copper core, making the fan look like a toad. The base is made of wrought iron, quite sturdy.