
A Sincere Warning: Always Wear Gloves When Doing These 7 Things—Or Risk Har.ming Your Health

A Sincere Warning: Always Wear Gloves When Doing These 7 Things—Or Risk Har.ming Your Health
Don't let a moment of inconvenience lead to long-term damage. Wearing gloves isn’t just about pampering your hands—it’s about protecting your health.
Some people scoff: “Why wear gloves for something so small? That’s over the top!” Others know they should, but skip it out of laziness.
But the truth is, wearing gloves before certain tasks does more than keep your hands clean—it can prevent serious health risks. Here are 7 situations where gloves aren’t optional—they’re essential.
1. Handling Seafood
A friend once cleaned fish barehanded and got pricked by a bone. At first, it seemed minor. By evening, her finger was swollen and she had a high fever.
Doctors later diagnosed her with a flesh-eating bacteria infection—fast-acting and potentially deadly. Not just fish—shrimp shells can also pierce skin, and if you already have a cut, the bacteria from seafood can easily enter and cause serious harm.
Always wear gloves when handling seafood. If you do get pricked, wash immediately, apply alcohol to disinfect, and seek medical attention if swelling or fever occurs.
2. Using Cleaning Chemicals
People often use bleach, alcohol, or other disinfectants barehanded. At first, I thought my peeling skin was just dryness—but no lotion helped. Turns out, harsh cleaners had damaged my skin barrier.
Even though these substances kill bacteria, they also degrade your skin's defenses. Prolonged exposure leads to faster aging, cracked skin, and sensitivity.
3. Touching Receipts or Tickets
Receipts, delivery slips, and movie tickets may look harmless, but they contain Bisphenol A (BPA)—a toxic chemical.
BPA is especially dangerous for pregnant women and children. Studies have shown that BPA levels on receipts can exceed safety limits by over 700 times. Worse yet, it only takes five seconds of contact for BPA to absorb into your skin, potentially harming your nervous and endocrine systems. Gloves are a smart precaution.
4. Refilling Printer Ink
No matter how careful I am, printer ink always ends up on my hands. It's hard to wash off and sometimes stays for days.
Ink contains dyes, carbon powder, and solvents that can cause rashes, allergic reactions, or even dermatitis. Colored inks may have heavy metals. Next time, wear gloves—don’t let the ink sink in.
5. Doing Housework
Wearing gloves while cleaning isn’t “extra”—it’s smart. Strong cleaners like toilet bowl gel or glass spray can erode your skin’s protective layer.
Without gloves, frequent exposure can lead to peeling, cracks, and long-term skin sensitivity, even eczema. Trust me, it’s not worth the regret later.
6. Gardening or Planting
Gardening may look relaxing, but it’s rough on your hands. When I planted succulents with bare hands, dirt got stuck deep in my nails and skin. My hands looked rough and aged overnight.
Soil, fertilizer, and thorns can scratch or irritate the skin. Gloves keep your hands soft and safe.
7. DIY or Home Repairs
I once painted a wall and glued tiles barehanded to save money. The paint stained my skin so badly I had to use harsh solvents to remove it—leaving my hands dry and burning for days.
If you forget gloves, try rubbing olive oil or baby oil on your hands before washing—it’s gentler than chemicals. But better yet: just wear gloves from the start.
Bottom line:
It’s not about being picky—it’s about prevention. Gloves may seem like a small detail, but they can save you from infections, skin damage, and serious health issues. Protect your hands—they do more for you than you think.
News in the same category


5 diseases that can cause stomach pain after eating - What your body may be trying to tell you?

30 Powerful Benefits of Sessile Joyweed (Alternanthera sessilis): A Traditional Plant with Remarkable Potential

Doctors warn: 6 types of food that can promote can.cer growth that people are unaware of
Why shouldn't you set the air conditioner to 26°C at night?

Are feet an "early warning sign" of cervical can:cer? Don't ignore these 4 situations
This is why some people always keep a lemon with them - it may help in unexpected situations

Don’t Ignore These 5 Symptoms at Night That Could Be Linked to Can.cer
Canadian Researchers Discover New Evidence That Vitamin D Shuts Down Cancer Cells
Warning: 6 vegetables that naturally contain to.xins

Lines on your nails could be a hidden health warning: What your body may be telling you?

20 Early Red Flags Your Body Uses to Warn You About Cancer

Why You Should Avoid Using Wet Wipes For Intimate Hygiene: An Expert Sheds Light

Eat 4 foods on an empty stomach in the morning to help clean the intestines, improve digestion, and prevent can.cer

Why should you stop eating tilapia right now? What you need to know before your next meal?
Noticing brown spots in your eyes? These causes may surprise you — and the solutions are simple

This is Why You Always Wake Up in the MIDDLE of the Night
Mini Stroke in People Over 40

Tiny White Pimples on Your Face? Here’s What Causes Them—and How to Get Rid of Them
News Post

Stir-Fried Glass Noodles with Shrimp

Grilled Chicken Rice Bowl with Corn

10 symptoms of dia.betes that may show up in your feet

5 diseases that can cause stomach pain after eating - What your body may be trying to tell you?

Loaded Cheesy Bacon Fries

Cheesy Stuffed Beef Buns (Baked Meat & Cheese Rolls)

30 Powerful Benefits of Sessile Joyweed (Alternanthera sessilis): A Traditional Plant with Remarkable Potential

Doctors warn: 6 types of food that can promote can.cer growth that people are unaware of
Why shouldn't you set the air conditioner to 26°C at night?

9 out of 10 people store onions incorrectly: Here's why you shouldn't keep them in the fridge

Smart travel tip: Why you should toss a water bottle under your hotel bed?
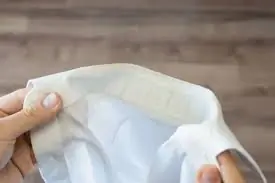
Don't throw away your yellowed white shirts - try this soaking method to make them bright and as good as new

Are feet an "early warning sign" of cervical can:cer? Don't ignore these 4 situations

Different Green Juices to Reduce Be.lly Fat
This is why some people always keep a lemon with them - it may help in unexpected situations

Classic Baked Lasagna

Don’t Ignore These 5 Symptoms at Night That Could Be Linked to Can.cer
Canadian Researchers Discover New Evidence That Vitamin D Shuts Down Cancer Cells
Warning: 6 vegetables that naturally contain to.xins
