
Relax 2025-02-11 17:54:35
Girls will understand

Answer: it is a toothbrush.
News in the same category

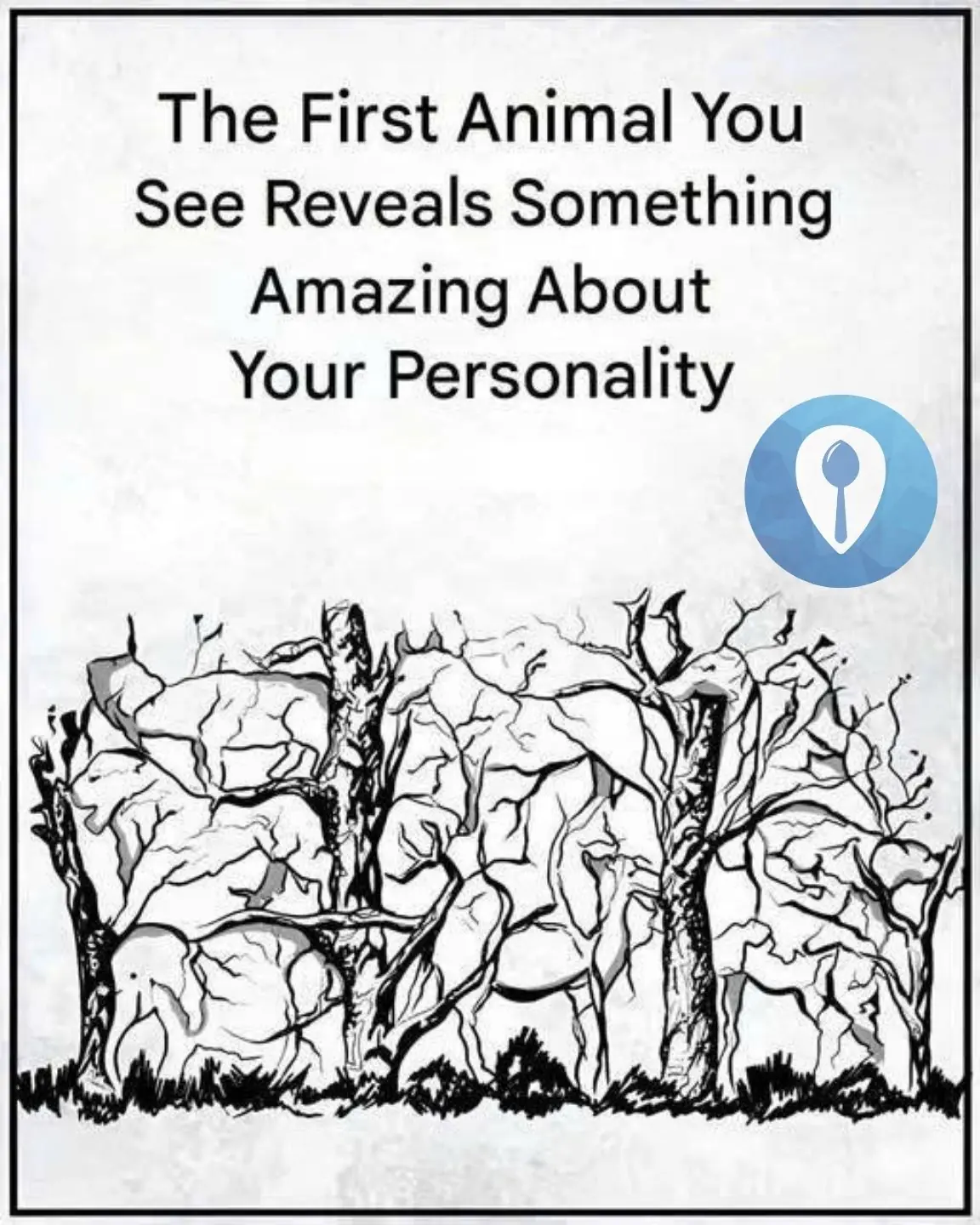
The First Animal You See Reveals Something Amazing About Your Personality

Traveling and saw a strange animal, hint: not a pig

What's strange in this photo?
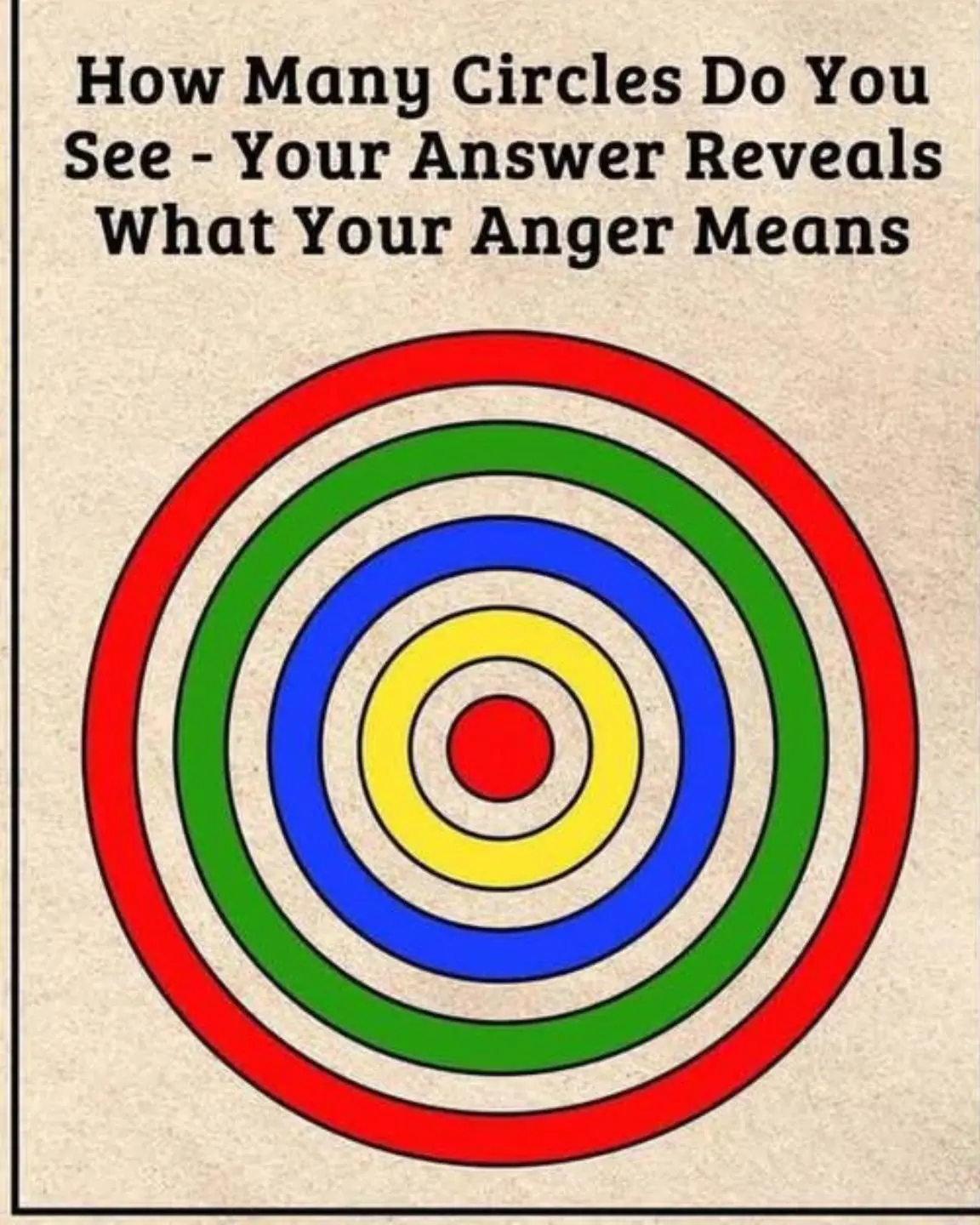
How many circles do you see?
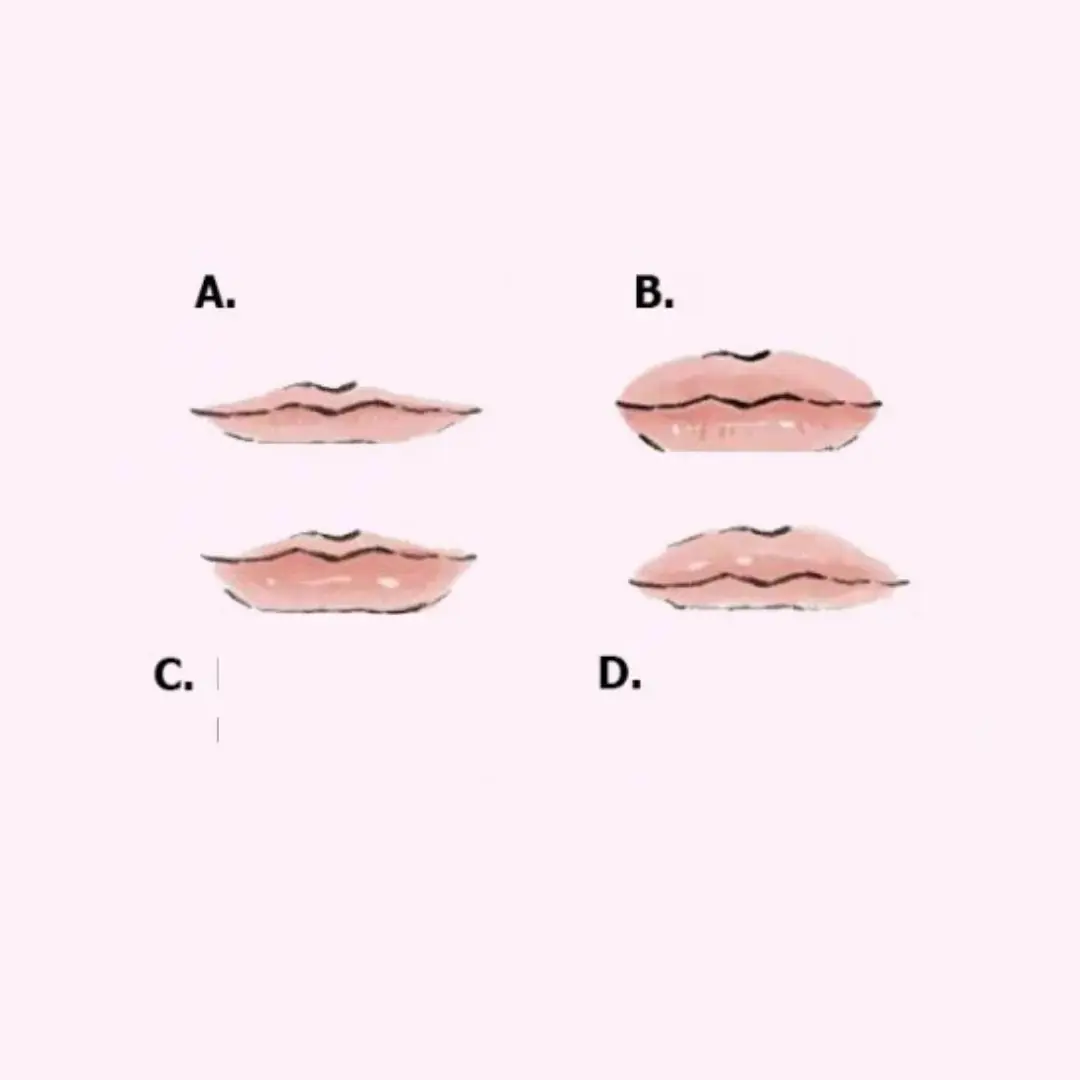
Look at the thickness of your lips, predict your rich or poor fate: Which type are you?
For those who don't know.
This is the correct way to move it.
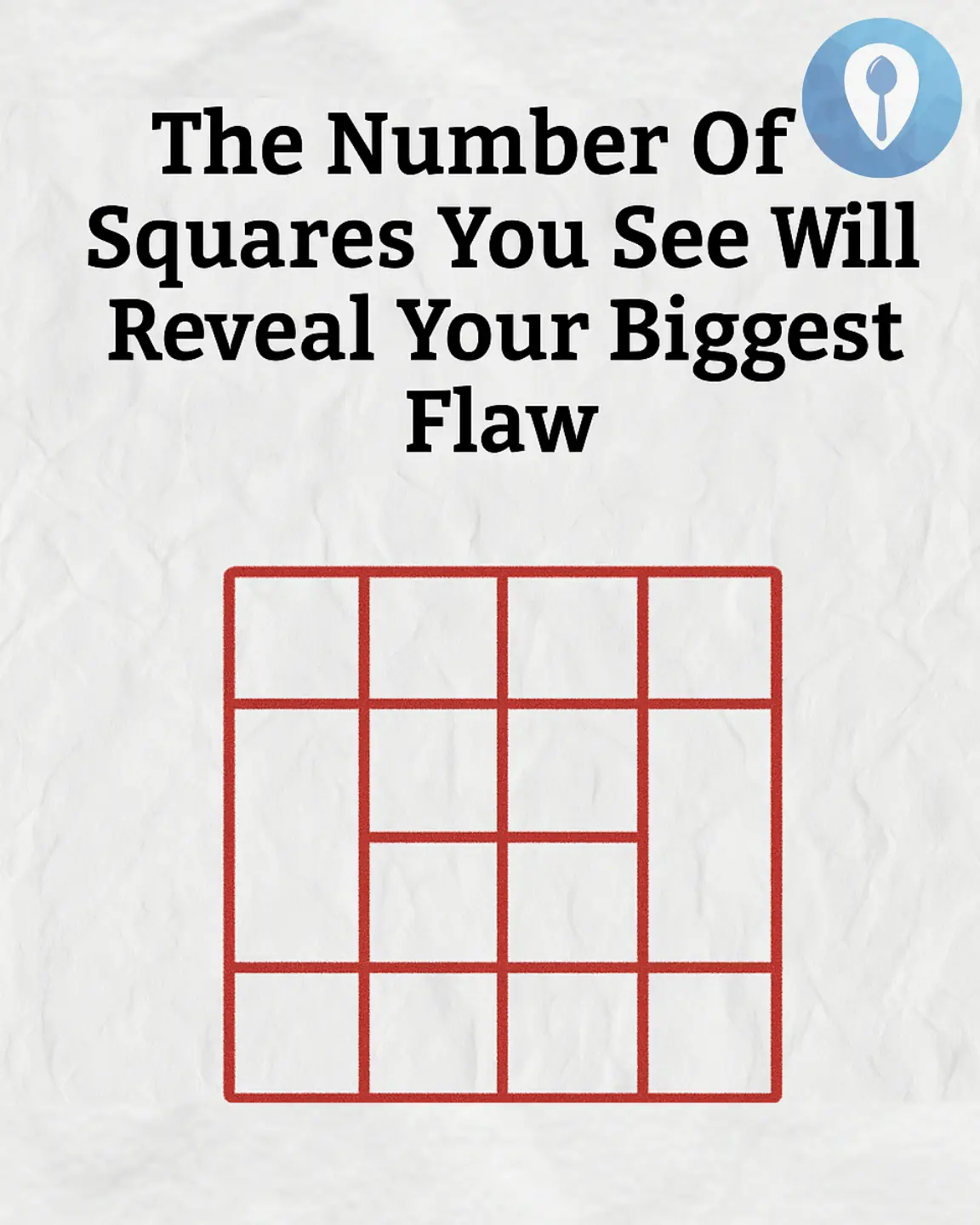
The Number of Squares You See Will Reveal Your Biggest Flaw?

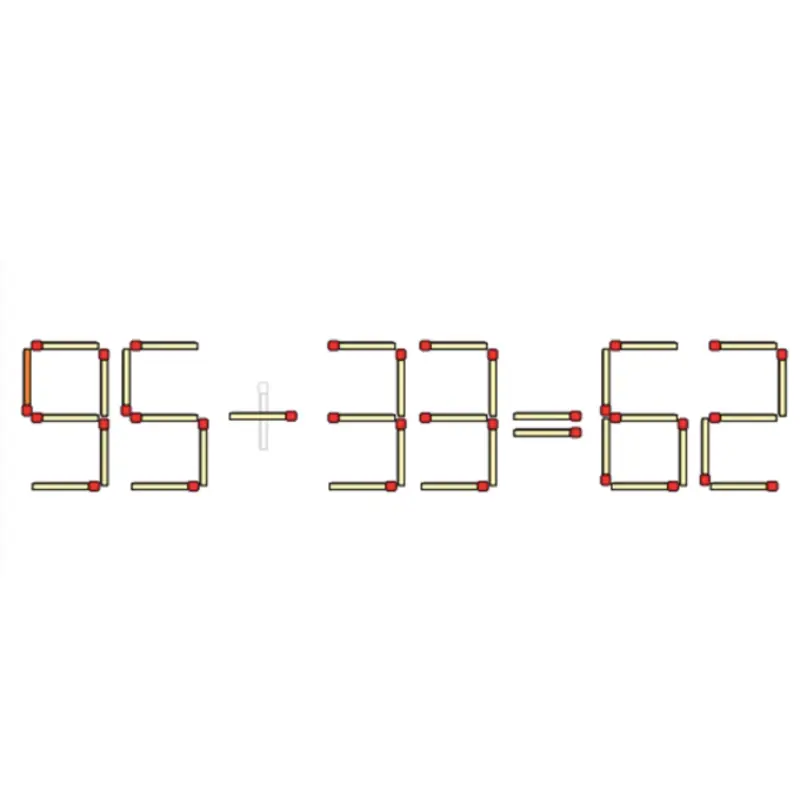
A Logic Puzzle That Stumped Many — Can You Solve It?

What is she so curious about 🤔

Find the 4 Hidden Faces in the Image
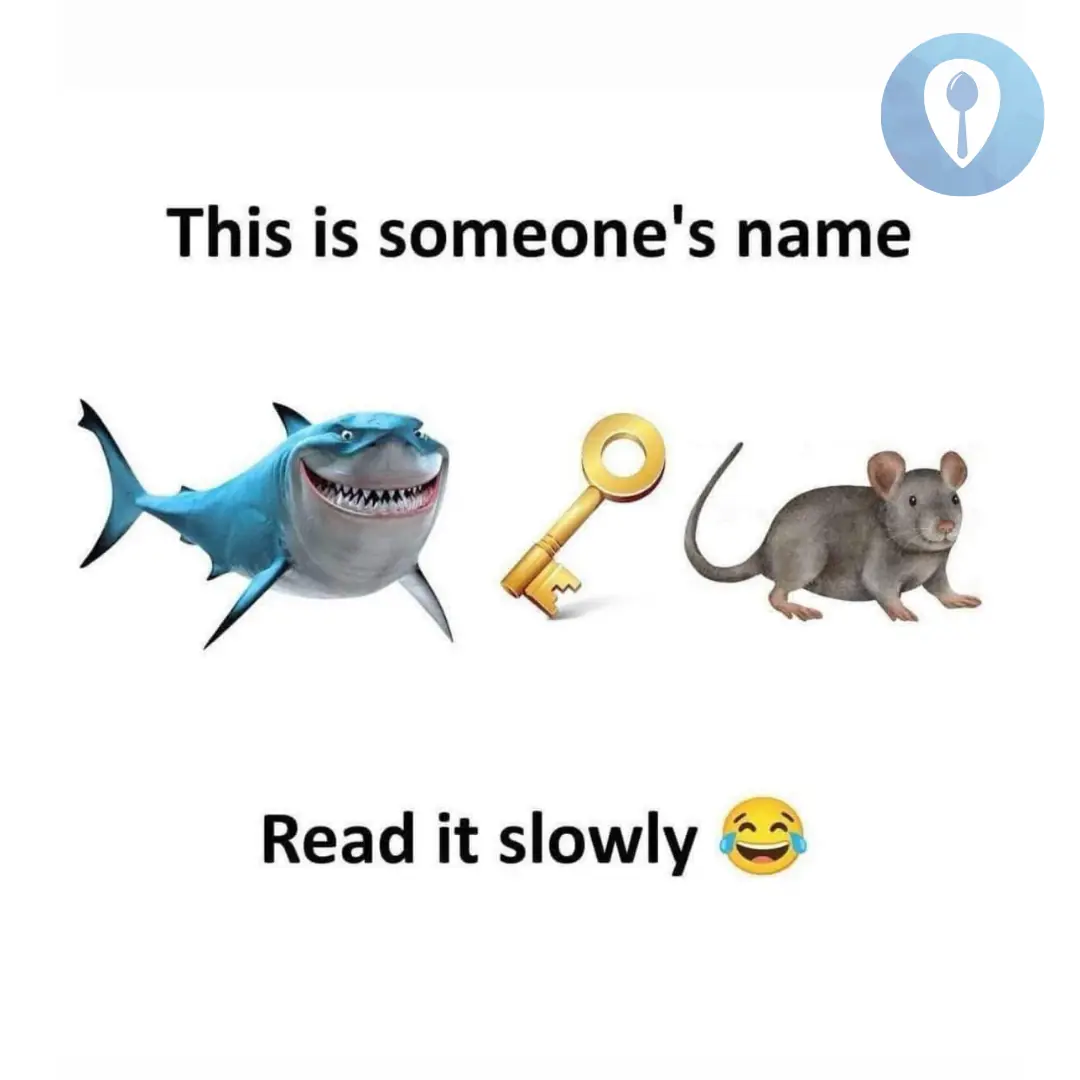
This is someone's name

Open the Right Doors to Win a Car
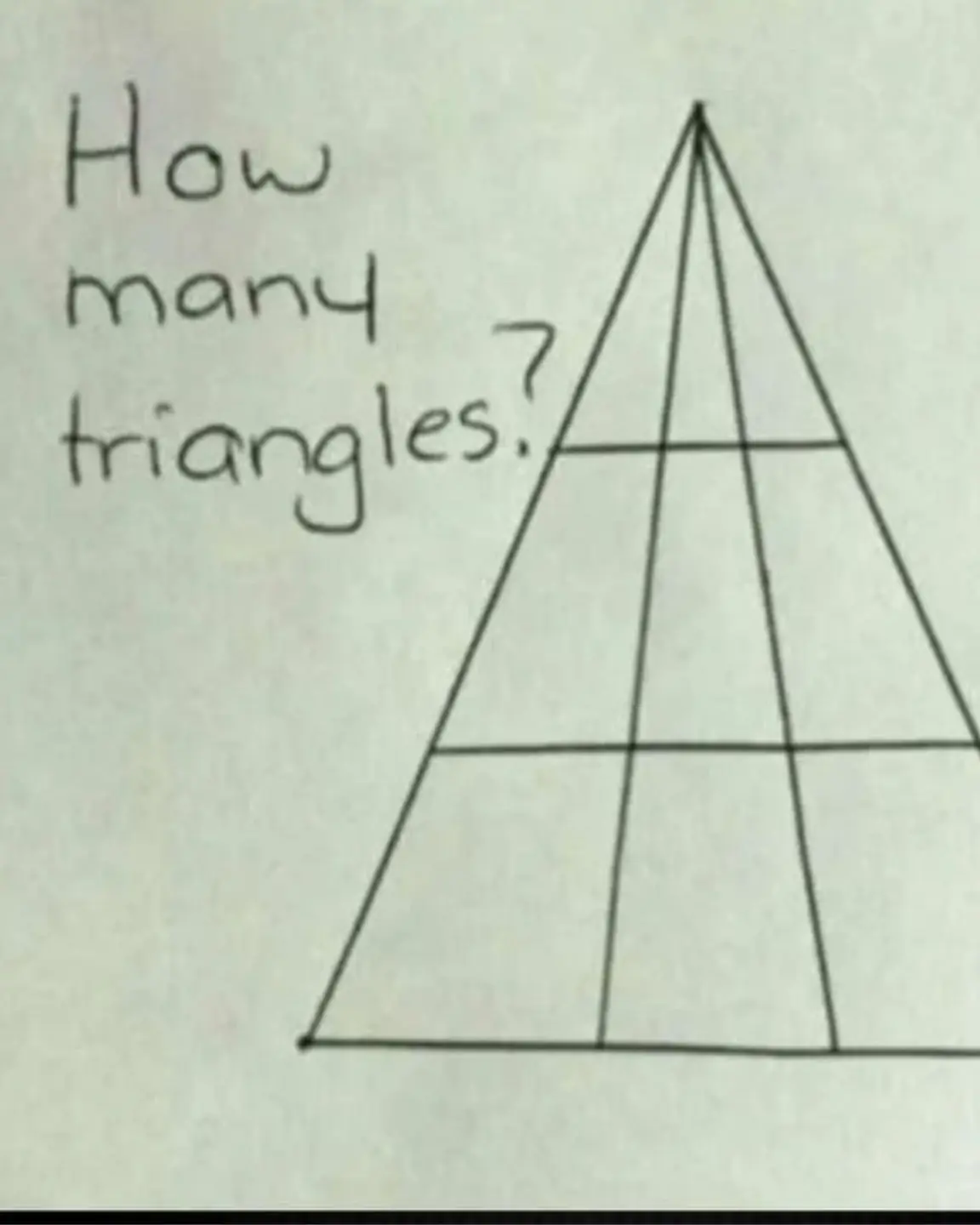
How many triangles?
Only Those Who Know Traffic Laws Can Spot the Mistake in This Image
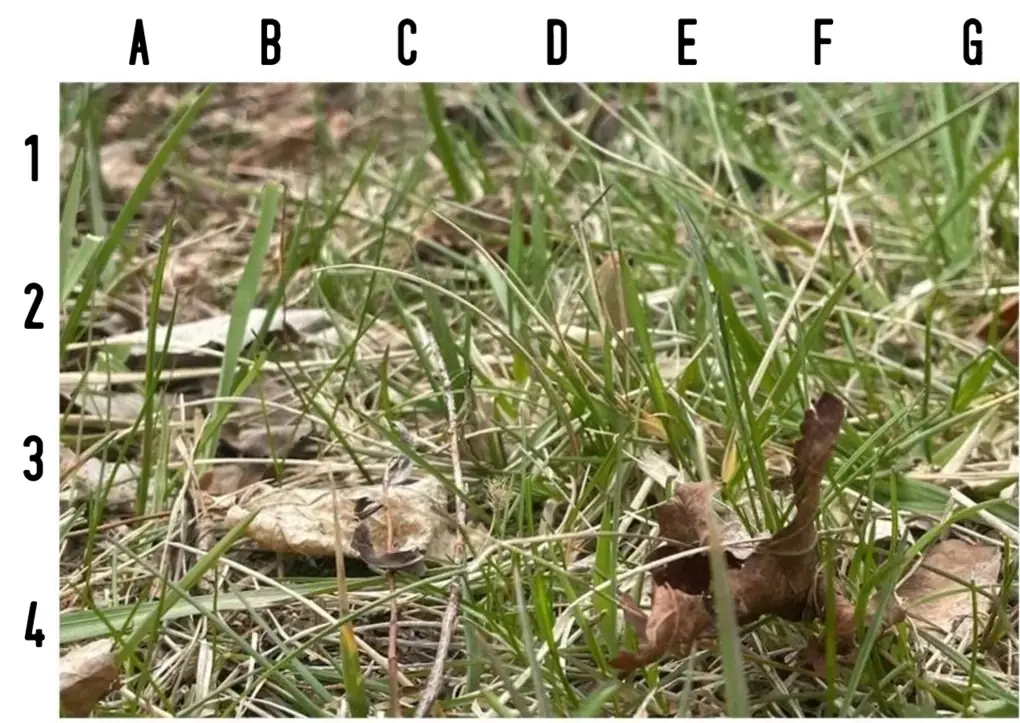
80% of people can't spot the snake within 5 seconds — can you?

Why Are So Many People Alarmed After Seeing This Photo?

Why Are Turn Signal Lights Yellow Instead of Green or Red?

Where are the 3 hidden faces?
News Post

Why do flight attendants like to bring a banana on the plane?
Facts 09/05/2025 10:41

What are the symptoms of no.seble.eds and when should you see a doctor?
Health 09/05/2025 10:40

Here's What Eating Blueberries Every Day Does to Your Body, Says a Registered Dietitian
Facts 09/05/2025 10:18

No matter how delicious they are, don't eat these 5 parts of the pig or you'll get si.ck
Tips 09/05/2025 09:57

5 common foods that ha.rm your li.ver
Health 09/05/2025 09:52

Tips to fix food that is too spicy when cooking
Tips 09/05/2025 09:46

Adding only water when cooking rice is a big mistake. I will share with you the secret that hotels use
Tips 09/05/2025 09:41

Cardinal Robert Francis Prevost elected as 267th pope, takes name Leo XIV
News 09/05/2025 08:45

Take These 5 Items Out of Your Fridge Now One Day They Could Actually "Explode"
Facts 08/05/2025 22:58

This type of leaf contains calcium
Tips 08/05/2025 22:41

Is it right to close the door tightly when using the air conditioner
Tips 08/05/2025 22:38

How to chase away a bunch of rats with just a handful of rice, without using toxic baits
Tips 08/05/2025 22:24

5 Eye Symptoms That May Signal Your Li.ver Is Crying for Help – Women, Don’t Ignore These if You Want to Stay Healthy Every Day
Health 08/05/2025 17:26

Tips to keep your flowers fresh
Tips 08/05/2025 14:58

Tips to make rice more delicious that not everyone knows
Tips 08/05/2025 10:28

8 Plants You Should Never Grow Indoors—and What You Should Plant Instead
Tips 08/05/2025 10:23

How to pick a sweet and juicy cantaloupe melon
Tips 08/05/2025 10:17

Before the divorce, my husband cooked my favorite fish dish, I was not moved but burst into tears because of 3 bitter truths
Facts 08/05/2025 09:58
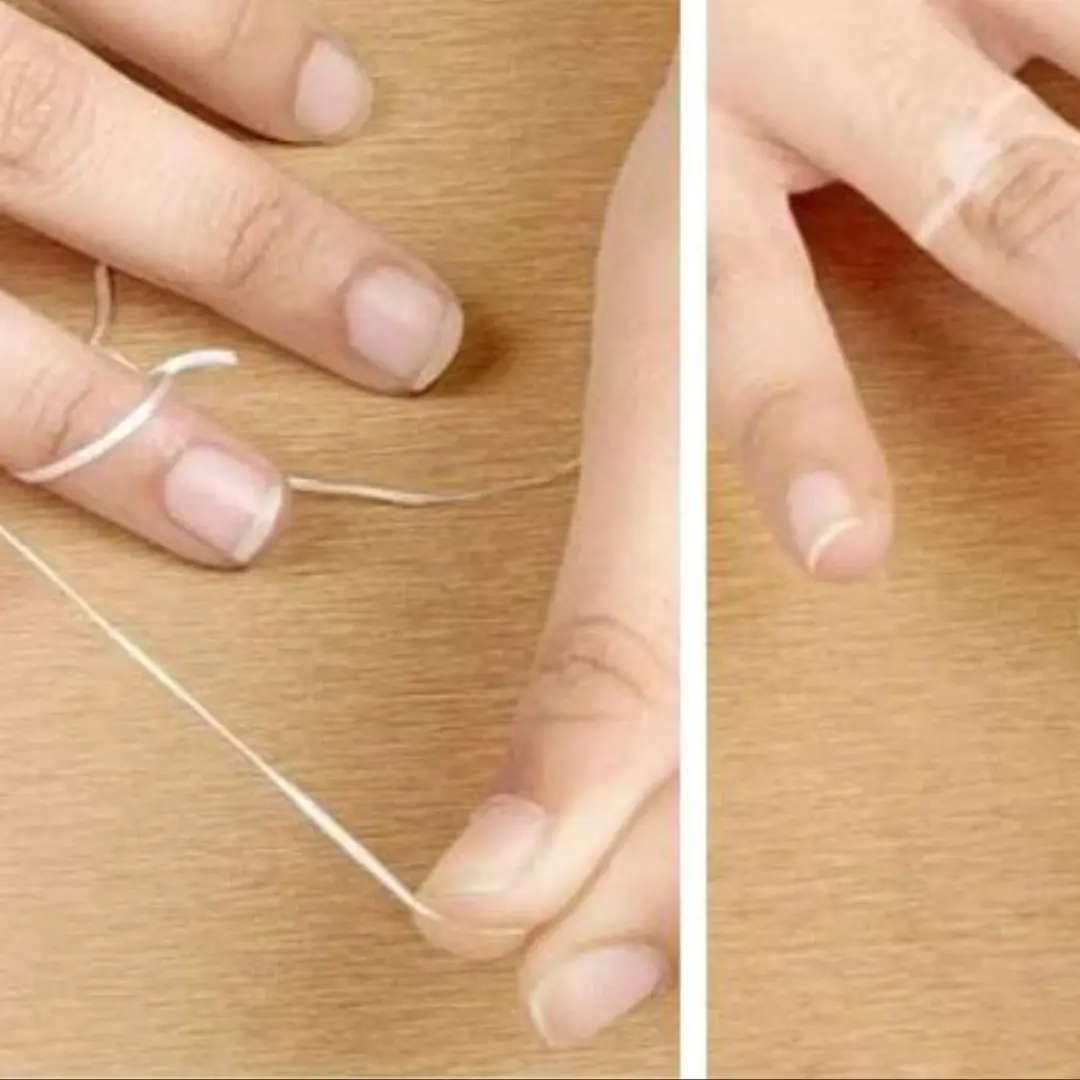
How to remove a tight ring on your hand easily without lube
Tips 08/05/2025 09:48

Everyone thinks that getting bitten by mosquitoes is due to blood type or body odor, but experts say: "Because you have this in your body."
Facts 08/05/2025 09:40