Follow this tip and your fish will stay fresh without losing its nutrients
1. Defrosting with salt water
Find a larger basin, pour a spoonful of salt into it and add enough water to cover the fish. Then add the salt and stir well until the salt is completely dissolved, then soak the frozen fish in it.
The defrosting effect of salt is very good, if the snow line is frozen, using salt to defrost is very practical, this method can also be applied to defrosting fish. Wait about 15 minutes and then we proceed to examine the condition of the fish, the fish has defrosted and does not affect the quality and taste of the fish.
2. Defrosting with white vinegar
Similarly, prepare a large pot, then pour in an appropriate amount of white vinegar, the amount of white vinegar should not be too much, otherwise the fish will be sour. After adding it, stir well and add the frozen fish.
This method may not be as fast as defrosting in salt water but is also very good, after about 20 minutes the fish will be soft.
3. Defrosting with a microwave
This method is very convenient to defrost, everyone can try it. Take the fish out of the refrigerator and put it in the microwave, it must be at a low temperature, first leave it for 3 minutes, after it is cooked, take it out and observe the state, if not, it is okay, turn it for another 1 or 2 minutes until it is completely defrosted.
Whether it is defrosting fish or defrosting pork, you can try this method, it defrosts quickly and does not affect the taste. Many people only use water to soak, even boiled water, this is not recommended.
News in the same category


To get rid of cockroaches, you can use several natural ingredients commonly found at home.

Sprinkle One Spoonful of This When Frying Fish: Perfect Golden Crisp, Even Cooking, and No More Sticking to the Pan

Added Too Much Salt While Cooking? Don’t Add Water — Use This Ingredient to Balance the Flavor

A little-known secret to keeping ginger fresh and delicious

How to fix a leaking refrigerator: Simple solutions and tips to extend its lifespan
When washing clothes, don't just put in detergent. Let me teach you a little trick

Oranges Are in Season, but Doctors Warn: Never Eat Oranges With These Three Types of Foods

Put an empty plastic bottle in the washing machine — the person who invented this hack must have sky-high IQ

This Surprising Hack Could Save You Thousands
Warm Water Each Morning Can Be a ‘Healing Tonic’—But It Turns into ‘Toxic Water’ If You Drink It in These 3 Harmful Ways

5 Surprising Changes That Happen to Your Body When You Drink Warm Lemon Water Every Morning

Snakes are very afraid of the smell of these 3 plants

When bitt.en by a snake, you should do these things first
There is a “secret button” on your washing machine — pressing it once can cut your electricity bill by 62%

The Phone’s Volume Buttons Have 6 Hidden Functions — Extremely Practical! Not Knowing Them Is Truly a Waste!

Amazing functions that many people don’t know about

3 fast and reliable methods to defrost fish safely and keep it ready for perfect cooking

7 powerful scents that repel snakes and keep your home safe

Put them in your home and mice will run away
News Post

There Is a Small Part Inside Your Washing Machine Open It Once a Month to Keep the Drum Clean and Your Clothes Smelling Fresh

Here’s Exactly What Happens to Your Body When You Eat Garlic Every Day

What happens to people who regularly eat sweet potatoes for breakfast over a long period of time?
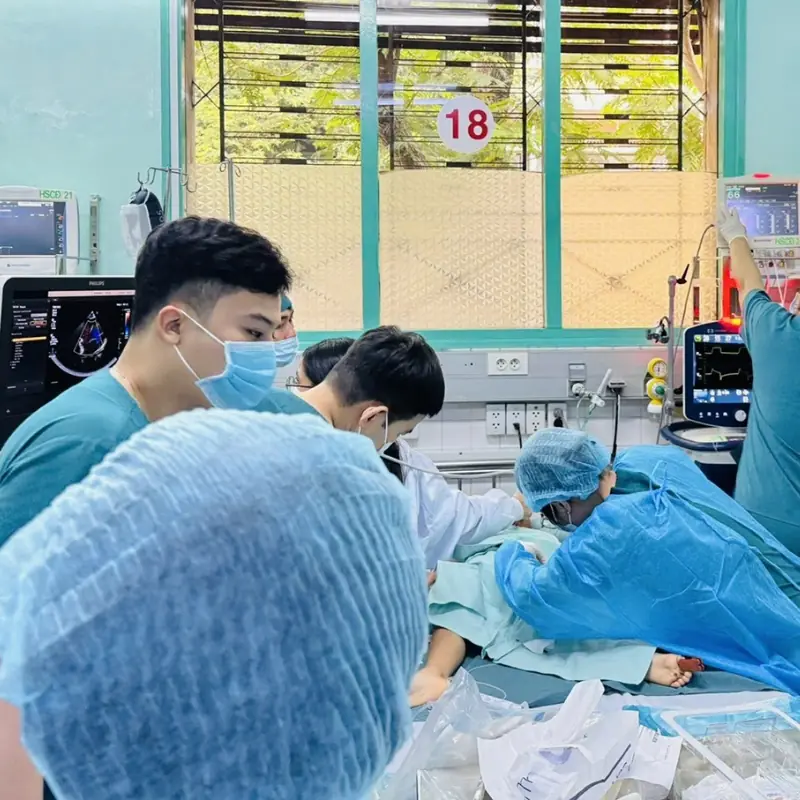
A De.a.dly Disease That Can K.i.ll Within Hours: Fatigue and Shortness of Breath in Children Should Never Be Ignored
A Shocking Family Revelation: From Rejection to Inheritance

One Month Before a Heart Attack, Your Feet May Warn You With These 6 Signs

Simple tips to deal with clogged pipes at home

Don’t Throw Away Rice-Washing Water: Discover Its Surprising Uses That Can Help You Save a Fortune

Shoulder discomfort may warn of liver can.cer in its early stages

If you have these two holes in your back, it means…

To get rid of cockroaches, you can use several natural ingredients commonly found at home.

4 Skin Symptoms That Could Be Warning Signs of Liver Disease 👇

What Happens to Your Body When You Eat 6 Roasted Garlic Cloves Every Day

A snowy roadside favor that reshaped my family’s future

Buttery Salmon & Roasted Veggie Bowl

Drink Coffee This Way to Extend Lifespan and Stay Younger, Experts Say

Guys, I need your attention for a moment

Bl.o.od Ca.n.cer: 10 Subtle Symptoms You Shouldn’t Ignore

If You Notice This Change in Your Feet, Your Fat:ty Liver May Be Beyond Repair