What Causes “Black Thorn” Disease? Understanding the Real Medical Condition Behind Dark Skin Patches
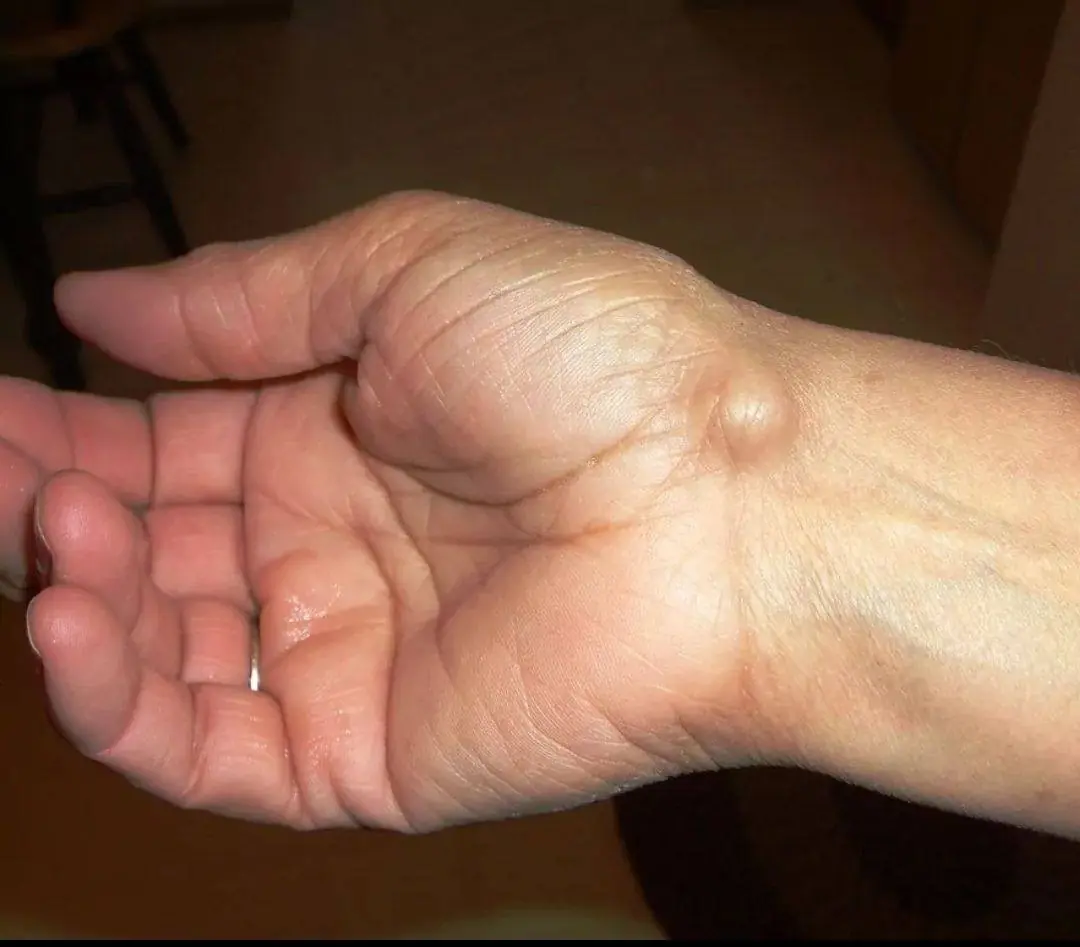
The term “black thorn disease” is not a recognized medical diagnosis. It is often used online to describe a skin condition characterized by dark, thickened patches, typically found around the neck, armpits, groin, or other body folds.
The actual medical term for this condition is acanthosis nigricans.
This article explains what acanthosis nigricans is, what causes it, who is at risk, and when medical evaluation is necessary.
What Is Acanthosis Nigricans?
Acanthosis nigricans is a skin condition marked by:
-
Darkened skin (brown to grayish-black)
-
Thickened, velvety texture
-
Symmetrical appearance
-
Commonly located in skin folds
It most frequently appears on:
-
Back of the neck
-
Armpits
-
Groin
-
Elbows
-
Knees
It is not contagious and is not an infection.



Primary Cause: Insulin Resistance
The most common underlying cause is insulin resistance.
When the body becomes resistant to insulin:
-
The pancreas produces more insulin.
-
Excess insulin stimulates skin cells.
-
Skin cells multiply more rapidly.
-
Pigmentation increases.
This leads to the characteristic thickened, darkened patches.
Insulin resistance is strongly associated with:
-
Type 2 diabetes
-
Prediabetes
-
Obesity
-
Polycystic ovary syndrome (PCOS)
In many cases, the skin change appears before diabetes is diagnosed.
Other Possible Causes
While insulin resistance is the most frequent cause, other factors may contribute:
1. Hormonal Disorders
-
PCOS
-
Thyroid dysfunction
-
Cushing’s syndrome
2. Medications
-
Corticosteroids
-
Oral contraceptives
-
Growth hormone therapy
3. Genetic Factors
Some individuals inherit a predisposition.
4. Rarely: Internal Malignancy
In very rare cases, sudden severe acanthosis nigricans in adults may be linked to underlying cancers (most commonly gastrointestinal). This form usually progresses rapidly and may involve unusual locations like palms or mucous membranes.



How Is It Diagnosed?
Diagnosis is primarily clinical — based on appearance.
Doctors may order:
-
Fasting blood glucose
-
HbA1c test
-
Insulin levels
-
Lipid profile
-
Thyroid function tests
The goal is not just treating the skin, but identifying the metabolic cause.
Can It Be Treated?
The skin condition improves when the underlying cause is addressed.
1. Weight Reduction
Even modest weight loss improves insulin sensitivity.
2. Blood Sugar Control
Managing prediabetes or diabetes may reduce progression.
3. Medication Adjustment
If caused by drugs, modifying therapy may help.
4. Topical Treatments
Creams containing:
-
Retinoids
-
Salicylic acid
-
Urea
These may improve texture but do not fix the root cause.



Important Clarifications
-
It is not caused by poor hygiene.
-
Scrubbing aggressively does not remove it.
-
It is not a fungal infection.
-
It is not contagious.
Many individuals mistakenly treat it as a cosmetic problem only. However, it is often a visible marker of internal metabolic imbalance.
When to Seek Medical Advice
Medical evaluation is recommended if:
-
The patches appear suddenly
-
They spread quickly
-
They occur in someone without obesity
-
They are accompanied by unexplained weight loss
-
There are additional symptoms like fatigue or excessive thirst
Early evaluation helps detect underlying metabolic conditions before complications develop.
The Bigger Picture
Acanthosis nigricans is best understood as a warning sign, not just a skin issue.
It often signals:
-
Insulin resistance
-
Prediabetes
-
Early metabolic syndrome
Addressing lifestyle factors — diet, physical activity, sleep — plays a major role in prevention and management.
The skin can reflect internal health.
If dark, thickened patches appear in body folds, professional medical assessment provides clarity and appropriate guidance.
Awareness leads to early action — and early action prevents long-term complications.