Check Your Eyes: 4 Vision Changes That May Be Linked to Diabetes
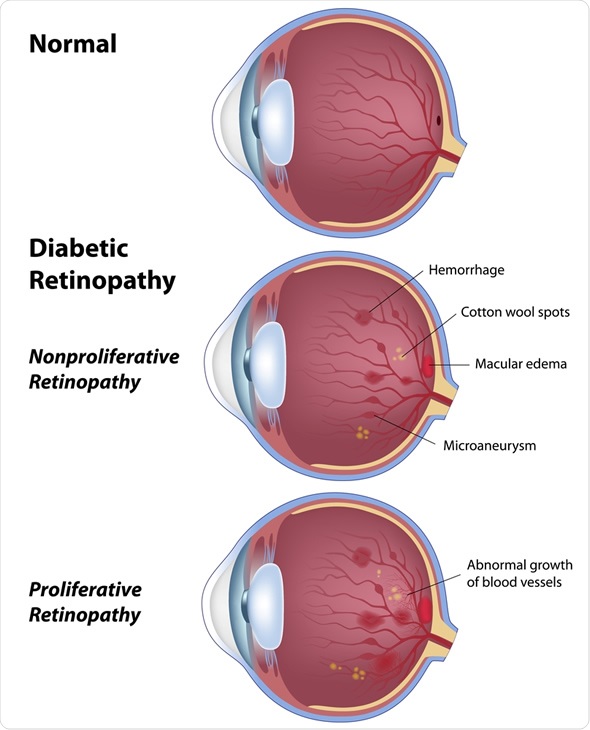
The image suggests that certain eye characteristics could indicate diabetes. While eye changes alone cannot diagnose diabetes, the eyes are one of the first places where long-term high blood sugar can cause visible damage.
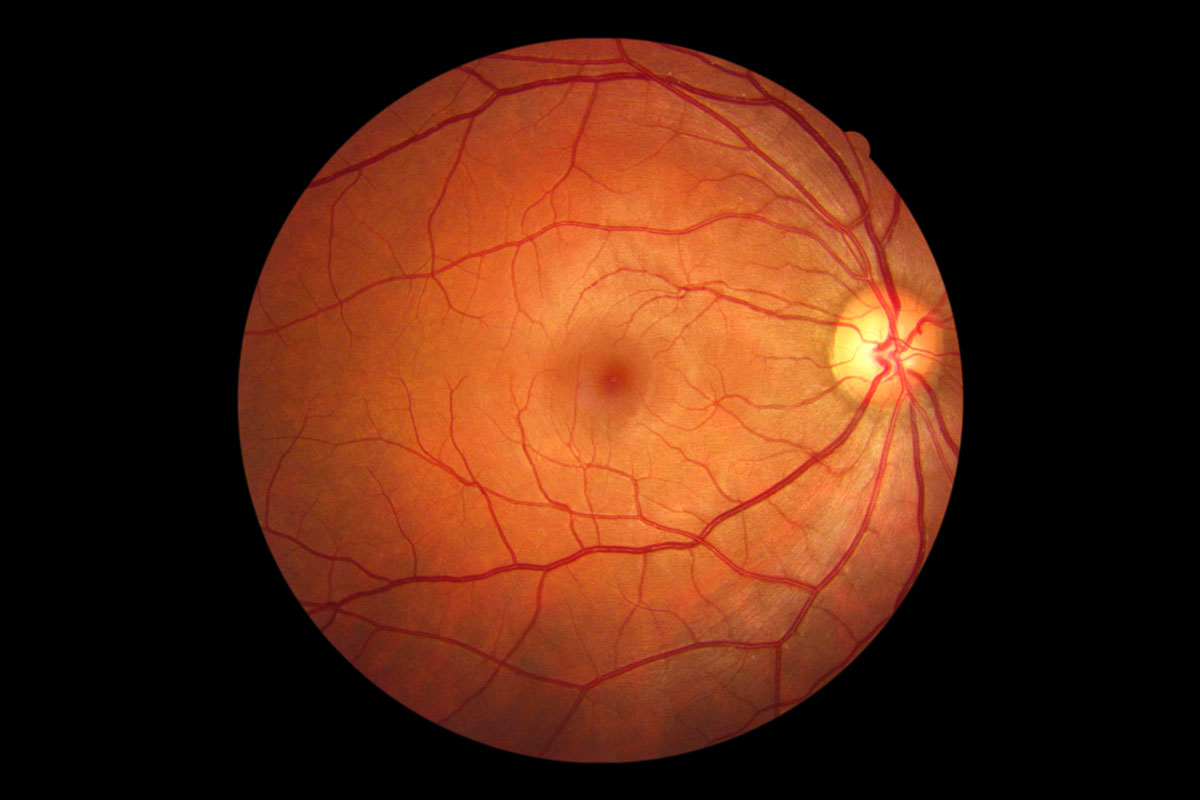
Diabetes affects small blood vessels throughout the body. The retina — the light-sensitive tissue at the back of the eye — contains delicate microvascular networks. When blood sugar remains elevated over time, these vessels can weaken, leak, or become blocked.
This article explains four common eye-related signs associated with diabetes, why they occur, and when medical evaluation is necessary.
1. Blurred or Fluctuating Vision
One of the earliest symptoms linked to uncontrolled blood glucose is temporary blurred vision.
High blood sugar can cause:
-
Swelling in the eye’s lens
-
Changes in fluid balance
-
Altered focusing ability
Vision may appear:
-
Slightly foggy
-
Out of focus
-
Variable throughout the day
Important distinction:
Temporary blur can occur even before permanent damage develops. However, persistent blurred vision should not be ignored.


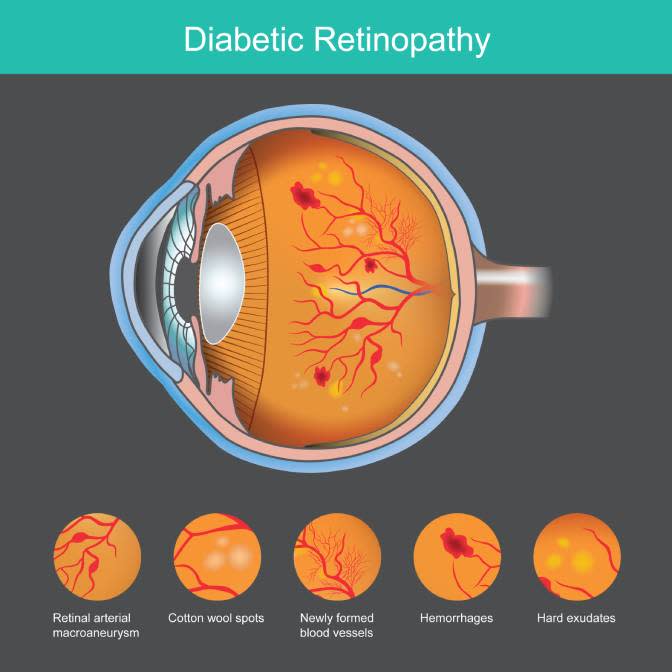
2. Dark Spots or Floaters
Small dark specks or “floating cobwebs” in vision may signal bleeding inside the eye.
In diabetic retinopathy:
-
Damaged retinal vessels leak blood
-
Tiny hemorrhages appear
-
Scar tissue may form
These changes can lead to:
-
Black spots
-
Shadowy areas
-
Sudden vision obstruction (in severe cases)
Sudden increase in floaters requires urgent ophthalmologic evaluation.
3. Difficulty Seeing at Night
Reduced night vision may develop due to retinal damage.
The retina contains photoreceptors responsible for adapting to low-light conditions. Chronic high glucose levels can impair their function.
Symptoms include:
-
Trouble driving at night
-
Slow adjustment from light to dark
-
Increased glare sensitivity
This may progress gradually, making it harder to notice initially.


4. Vision Loss in One Area
Advanced diabetic retinopathy may cause:
-
Partial vision loss
-
Distorted straight lines
-
Dark or empty areas in central vision
This can occur if:
-
New fragile blood vessels grow (proliferative retinopathy)
-
The macula becomes swollen (macular edema)
Macular edema is one of the leading causes of diabetes-related vision impairment.
Immediate specialist care is critical in such cases.
How Diabetes Damages the Eyes
Chronic hyperglycemia leads to:
-
Capillary wall weakening
-
Microaneurysms
-
Leakage of fluid and lipids
-
Abnormal blood vessel growth
Over time, untreated damage may result in permanent vision loss.
Early stages may have no symptoms at all.
Important Clarification
Eye symptoms alone do not confirm diabetes.
Diagnosis requires:
-
Fasting blood glucose testing
-
HbA1c measurement
-
Oral glucose tolerance testing
Some eye symptoms can result from:
-
Aging
-
Hypertension
-
Migraine aura
-
Vitamin deficiencies
-
Retinal tears unrelated to diabetes
Medical testing is essential for accurate diagnosis.
Who Should Be Especially Vigilant?
Higher risk individuals include:
-
Adults over 40
-
Individuals with obesity
-
Family history of diabetes
-
Sedentary lifestyle
-
History of gestational diabetes
-
High blood pressure
Even without symptoms, people with diabetes should receive comprehensive dilated eye exams at least once per year.

Prevention and Protection
The most effective protection strategies include:
-
Maintaining stable blood glucose levels
-
Controlling blood pressure
-
Managing cholesterol
-
Avoiding smoking
-
Scheduling routine eye exams
-
Following prescribed medication plans
Early detection significantly reduces risk of severe vision loss.
When to Seek Immediate Care
Urgent evaluation is needed if:
-
Sudden vision loss occurs
-
A curtain-like shadow appears
-
Flashing lights accompany floaters
-
Eye pain develops
-
Severe headache occurs with vision changes
These symptoms may indicate retinal detachment or advanced bleeding.
The Balanced Perspective
Not every eye change means diabetes. However, diabetes frequently affects the eyes before other symptoms become obvious.
Vision changes are signals — not diagnoses.
Routine screening, metabolic control, and professional evaluation remain the most reliable strategies for protecting eyesight long-term.
If persistent visual symptoms occur, medical testing provides clarity and appropriate treatment options.
Awareness prevents complications.