
What Raw Garlic Can Do for Your Health May Surprise You
What Raw Garlic Can Do for Your Health May Surprise You
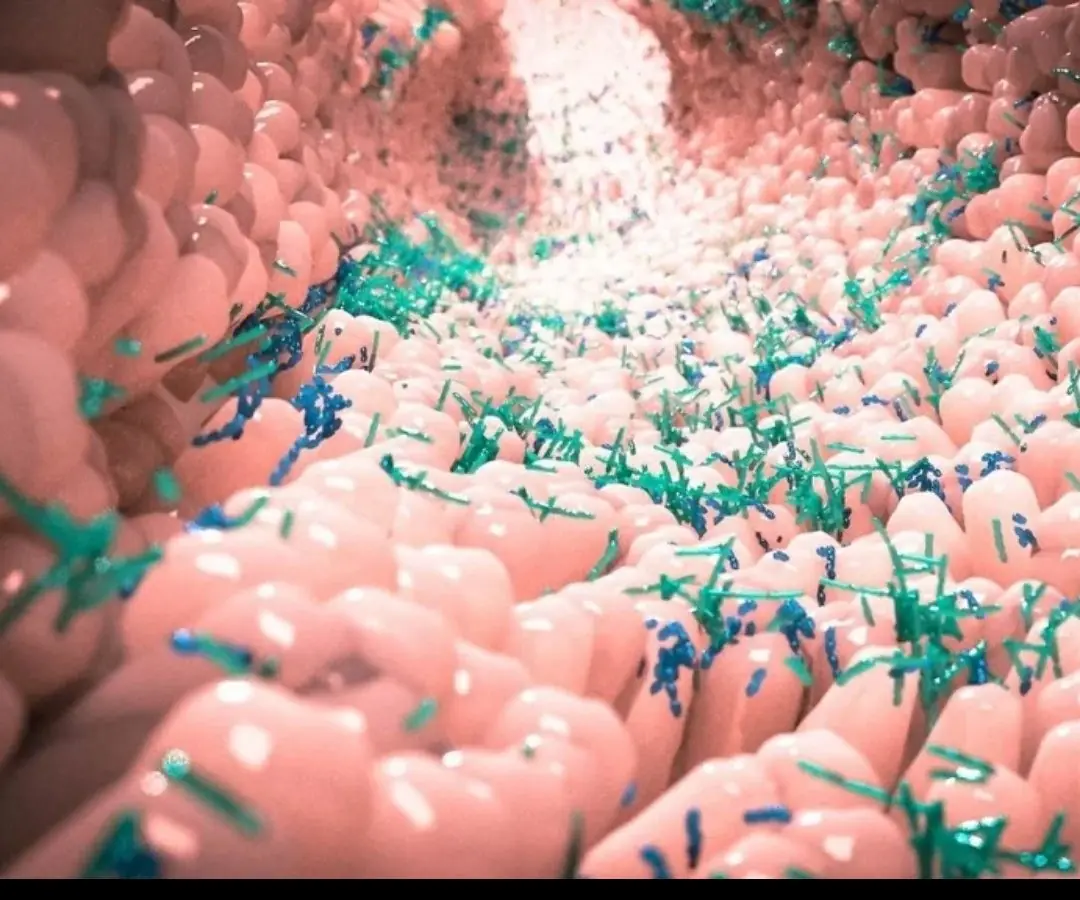
The gut is no longer just about digestion.
In recent years, science has been slowly pulling back the curtain on a hidden world inside the body—one that may influence the brain, the immune system, and even the development of serious neurological diseases.
A recent twin study has added powerful evidence to a growing idea:
the gut microbiome may play a critical role in the development of Multiple Sclerosis (MS).
This isn’t hype.
It’s a shift in how disease is understood.

Identical twins share the same DNA.
If genetics were the only cause of MS, both twins would almost always develop the disease.
But that’s not what researchers see.
In many twin pairs, one twin develops MS while the other remains healthy. This gap has pushed scientists to look beyond genes—and straight into the environment inside the body.
The gut microbiome became a prime suspect.
The gut microbiome is a massive ecosystem of trillions of microorganisms—bacteria, viruses, fungi—living inside the digestive tract.
These microbes:
Help digest food
Train the immune system
Influence inflammation
Communicate with the brain through the gut–brain axis
In other words, they are not passive passengers.
They actively shape how the body responds to threats—including its own tissues.
Researchers compared the gut bacteria of twins where:
One twin had MS
The other did not
The results were striking.
The microbiome composition was noticeably different, despite identical genetics and similar upbringing. Certain bacterial species were more abundant in the twin with MS, while protective bacteria were reduced.
This suggests that microbial imbalance—also called dysbiosis—may help trigger immune dysfunction that contributes to MS.
Not cause it alone.
But push the system in the wrong direction.
Multiple Sclerosis is an autoimmune disease.
The immune system mistakenly attacks the protective covering of nerve fibers in the brain and spinal cord.
So where does the gut come in?
Research suggests gut bacteria can:
Activate immune cells that promote inflammation
Suppress regulatory immune cells that normally prevent autoimmunity
Increase gut permeability (“leaky gut”), allowing inflammatory molecules into circulation
Once immune balance is disrupted, the nervous system becomes vulnerable.
The gut doesn’t start MS—but it may help decide whether the switch gets flipped.
For decades, MS research focused heavily on:
Genetics
Brain lesions
Immune-suppressing drugs
The microbiome adds a new layer—one that is dynamic and potentially modifiable.
Unlike genes, gut bacteria can change through:
Diet
Antibiotic exposure
Stress
Infections
Lifestyle habits
That opens doors science couldn’t open before.
Not that simple.
MS is complex.
There is no single cause, no magic probiotic, no guaranteed prevention strategy.
But the study strongly suggests that:
The microbiome may influence disease risk
It may affect disease severity
It could become a future treatment target
Some early research is already exploring:
Personalized probiotics
Diet-based microbiome modulation
Fecal microbiota transplantation (still experimental)
This is early-stage science—but it’s moving fast.
The twin study highlights something crucial:
Genes load the gun.
Environment pulls the trigger.
And the gut microbiome sits right at the intersection of both.
Two people can share DNA, family, childhood, even meals—and still develop radically different immune responses over time.
Tiny microbial differences may accumulate quietly for years before disease appears.
This study doesn’t rewrite MS overnight—but it changes the direction of the conversation.
Future research is likely to focus on:
Identifying harmful vs protective bacterial patterns
Understanding how gut changes interact with immune cells
Developing therapies that support immune balance rather than suppress it blindly
Instead of only treating symptoms, science may move closer to modifying underlying drivers of disease progression.
This research does not mean:
Gut bacteria alone cause MS
Diet cures MS
Supplements replace medical treatment
MS remains a serious neurological condition requiring professional care.
But it does mean that the body is more interconnected than once believed—and that the gut may be a powerful player in neurological health.
The twin study delivers a clear message:
Multiple Sclerosis is not just a brain disease.
It’s an immune disease.
And the immune system listens closely to the gut.
Understanding that connection may be one of the most important steps toward better prevention strategies, more personalized treatments, and a deeper understanding of why MS affects some people—and not others.
Sometimes, the key to the brain
starts much lower than expected.

What Raw Garlic Can Do for Your Health May Surprise You

Doctors Warn Parents After 5-Year-Old Dies From Late-Stage Cancer

Your hands can reveal li.ver trouble — don’t ignore these shocking signs

Sometimes, the strongest protection starts right on your balcony:

2 Tablespoons of This and You’ll Notice Incredible Results For Your Digestive Problems....

These “Healthy” Vegetables Could Actually Increase Canc:er Risk — Experts Warn to Avoid

3 Foot Warning Signs That Could Indicate Serious Internal Organ Issues

Bathing at the Right Time Could Reduce Stroke Risk — Here’s When
These 8 bathroom signs might seem harmless—but they could point to cancer

What Happens to Your Body If You Eat Sweet Potatoes for Breakfast Every Day?

Broccoli is healthy, but doctors say it may cause issues for some people.

Vegetables are among the most beneficial foods for heart health due to their high fiber content, low sodium levels, and rich nutrient profile.

3 husband behaviors that may increase the risk of cer.vical can.cer in wives

Why Do Women Cross Their Legs When Sitting? The Psychology, Culture, and Comfort Behind a Common Habit

10 warning signs of pancreatic can.cer you shouldn’t overlook

Fatty liver disease is often called a “silent condition” because it can progress for years without obvious symptoms.

Boiling Water the Wrong Way?

The parents of a 10-year-old girl who sadly died by suicide have talked about the changes they noticed in her prior to her death.

The Body Can Sense When Life Is Near Its End — And the First Signs May Appear in the Nose

A Japanese business tycoon has identified three habits commonly seen in people who are destined to fail.

What Raw Garlic Can Do for Your Health May Surprise You

Doctors Warn Parents After 5-Year-Old Dies From Late-Stage Cancer

Your hands can reveal li.ver trouble — don’t ignore these shocking signs

Sometimes, the strongest protection starts right on your balcony:

2 Tablespoons of This and You’ll Notice Incredible Results For Your Digestive Problems....

These “Healthy” Vegetables Could Actually Increase Canc:er Risk — Experts Warn to Avoid

3 Foot Warning Signs That Could Indicate Serious Internal Organ Issues

Bathing at the Right Time Could Reduce Stroke Risk — Here’s When
These 8 bathroom signs might seem harmless—but they could point to cancer

Here are eight warning signs that your mind may be running on empty, and why taking them seriously matters.

What Happens to Your Body If You Eat Sweet Potatoes for Breakfast Every Day?

Popular beliefs link certain body traits to health, youth, and vitality.

Broccoli is healthy, but doctors say it may cause issues for some people.

Vegetables are among the most beneficial foods for heart health due to their high fiber content, low sodium levels, and rich nutrient profile.

3 husband behaviors that may increase the risk of cer.vical can.cer in wives
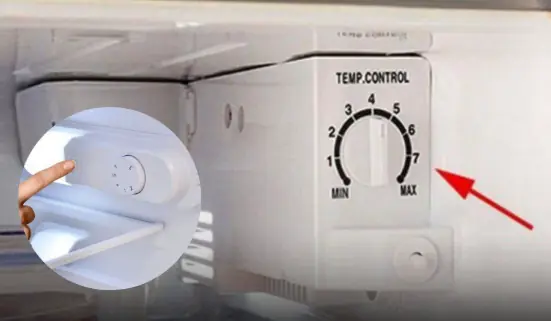
A Small Button in Your Refrigerator Can Save You a Lot on Electricity Bills – Many People Don’t Know This

Why Do Women Cross Their Legs When Sitting? The Psychology, Culture, and Comfort Behind a Common Habit