
Guide to Cultivating Cantaloupe in Your Garden

Cantaloupe, known for its sweet, juicy flesh and vibrant orange color, is a favorite summer fruit. Whether you're growing it for its delicious flavor or simply for the joy of cultivating something from scratch, cantaloupe can be an incredibly rewarding crop to grow in your garden. This guide will walk you through the essential steps of cultivating cantaloupe, from choosing the right variety to harvesting your fruit.
1. Choosing the Right Variety
Cantaloupe belongs to the Cucurbitaceae family and is closely related to melons like watermelon and honeydew. There are different varieties of cantaloupe, and selecting the right one for your climate and growing space is important. Popular varieties include:
-
Galia: A small, round melon with green flesh and a sweet taste.
-
Cantaloupe (Muskmelon): The classic orange-fleshed melon most commonly found in supermarkets.
-
Sugar Cube: A smaller melon, perfect for limited spaces and offering a high sugar content.
When choosing a variety, make sure it is suitable for your growing zone. Cantaloupes require a warm growing season with temperatures between 70-90°F (21-32°C).
2. Preparing the Soil
Cantaloupes thrive in well-drained, sandy-loam soil that is rich in organic matter. Here’s how to prepare the soil for planting:
-
Location: Choose a sunny spot in your garden where the plants will get at least 8 hours of direct sunlight per day.
-
Soil Preparation: Cantaloupes prefer slightly acidic to neutral soil with a pH of 6.0 to 6.5. Amend your soil with compost or organic matter to improve fertility and drainage.
-
Soil Drainage: Ensure the area is well-drained to prevent root rot. If your soil is clayey or compacted, consider creating raised beds or mounds to improve drainage.
3. Planting Cantaloupe
Cantaloupe is typically grown from seeds. Here’s the process for starting your cantaloupe plants:
-
Timing: Start planting cantaloupe seeds outdoors only when the risk of frost has passed, and the soil temperature is consistently above 70°F (21°C). This usually happens in late spring or early summer.
-
Spacing: Plant cantaloupe seeds 1 inch (2.5 cm) deep and space them about 18-36 inches (45-90 cm) apart, depending on the variety. Leave at least 3 feet (91 cm) between rows to provide plenty of space for vines to spread.
-
Transplanting (Optional): If you’re starting cantaloupe indoors, start seeds 2-3 weeks before the last expected frost and transplant seedlings when the outdoor conditions are ideal for growth.
4. Caring for Cantaloupe Plants
Proper care is key to a successful cantaloupe harvest. Here are some essential tips:
-
Watering: Keep the soil consistently moist but not soggy. Water the plants deeply to encourage strong root growth, particularly during the flowering and fruiting stages. Avoid overhead watering, as wet leaves can promote fungal diseases.
-
Mulching: Apply mulch around the base of the plants to retain moisture, suppress weeds, and maintain an even soil temperature.
-
Fertilization: Use a balanced, slow-release fertilizer rich in phosphorus and potassium to promote strong flowers and fruit development. Avoid excessive nitrogen, as it can lead to vigorous leaf growth at the expense of fruit production.
-
Pruning: Pruning isn’t strictly necessary, but you can pinch back the vines once they have 4-6 leaves to encourage lateral growth and larger fruits. This also helps the plant focus energy on producing fruit.
5. Pollination
Cantaloupe plants produce both male and female flowers. Pollination is crucial for fruit production, and it is typically carried out by bees and other pollinators. If you’re growing cantaloupe in an area with limited pollinator activity, consider hand-pollinating the flowers.
To hand-pollinate:
-
Use a small brush or cotton swab to transfer pollen from the male flowers (which have thin stems) to the female flowers (which have small fruit buds at the base).
6. Harvesting Cantaloupe
Cantaloupes take about 70-90 days to reach maturity, depending on the variety and growing conditions. Here’s how to know when to harvest:
-
Color Change: The skin of the cantaloupe should change from green to a yellow or beige color, depending on the variety.
-
Fragrance: Ripe cantaloupe will emit a sweet, fruity aroma near the stem end.
-
Slip from the Vine: One of the most telling signs of ripeness is when the melon easily slips off the vine with a gentle tug. The stem should be slightly dry, indicating that the melon is fully ripe.
-
Sound: When tapped, a ripe cantaloupe will produce a hollow sound.
7. Storing Cantaloupe
Once harvested, store cantaloupes in a cool, dry place. Uncut cantaloupes can be stored at room temperature for up to a week, allowing the flavor to develop. Once cut, refrigerate the melon and consume it within a few days.
Conclusion
Growing cantaloupe in your garden can be a fun and rewarding experience, especially when you’re able to enjoy the sweet, juicy fruit you’ve cultivated yourself. By choosing the right variety, preparing the soil, ensuring proper care, and watching for the signs of ripeness, you can successfully grow cantaloupe and harvest your own delicious melons.
Happy gardening and enjoy your homegrown cantaloupes!
News in the same category


The husband slapped his wife in front of his friends to show off — but her act of revenge left everyone shocked and speechless

10 Clever Ways to Reuse Lemon Seeds at Home

Unlocking the Secret Health Benefits of Common Mallow: Nature’s Wonder Herb for Wellness

Essential Knowledge for Growing Cassava Successfully

Growing Kale: Planting, Care, and Harvesting Tips

Just 1 Cup Makes Peace Lilies Bloom with So Many Flowers
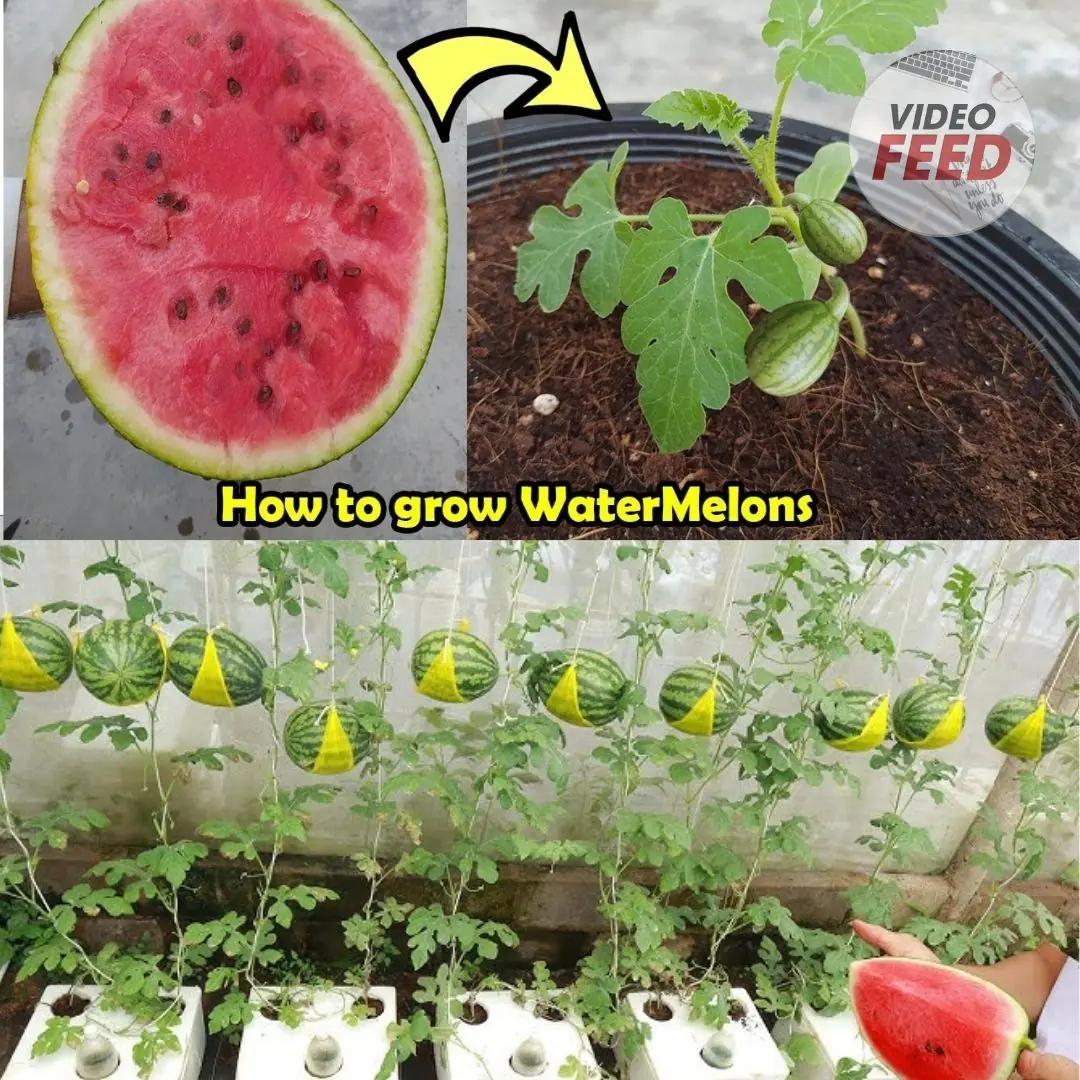
How to Grow Watermelons at Home: A Guide for Small Spaces & Balconies

How to Grow a Banana Tree at Home and Never Buy Bananas Again

Here’s How to Grow Calamansi at Home — No Farm Needed

How to grow tulips indoors – a step-by-step guide to forcing these beautiful bulbs

How to Grow Habanero Peppers in Pots

Grow These 5 Garden Beans This Summer

Why Asians Are Rushing to Grow This “Miracle Tree”: Heals Like Medicine, Sells Like Gold

How to Grow and Care for Dieffenbachia

How to Grow and Care for Phalaenopsis Orchids Indoors

Portulaca in Pots: The Complete Guide to Growing Colorful & Drought-Tolerant Flowers Outdoors

10 Tips for Growing Superb Spring Spinach

How to Make Rose Petal Lemonade – A Refreshing Homemade Drink

How to Grow Carrots at Home in Containers Starting with a Single Carrot
News Post

Squeeze a Few Drops of Lemon Into the Rice Cooker: Why This Simple Trick Is Winning Over Home Cooks
A simple lemon trick may change how your rice tastes and lasts.

A Feminine Touch
he large Neolithic farming community of Çatalhöyük in southern Anatolia has long tantalized archaeologists as a possible example of a matriarchal society.

Don’t Ignore These 10 Common Warning Signs of Neurological Disorders
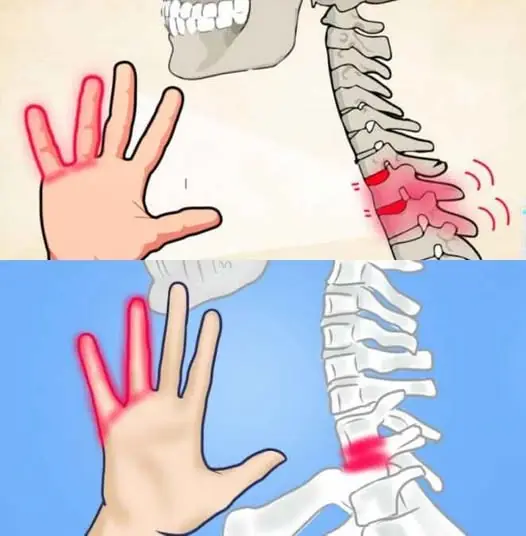
If your HANDS fall asleep it's a clear sign that you have can...
If your HANDS fall asleep it's a clear sign that you have can...

2050 and Beyond: Imagining the Future of Life

The Military Sleep Method That Makes 96% of People Fall Asleep in Just 2 Minutes
The Military Sleep Method That Makes 96% of People Fall Asleep in Just 2 Minutes

A 40-Year-Old Man Diagnosed With End-Stage Li.ver Can.cer: He Ignored a Warning Sign for Three Months
A symptom that seemed harmless turned out to be the body’s first “warning letter.”

The Body Can Sense When Life Is Near Its End — And the First Signs May Appear in the Nose
The Body Can Sense When Life Is Near Its End — And the First Signs May Appear in the Nose

Japanese Business Tycoon: Only One Type of Person Can Truly Become Wealthy — Avoid These Three Things If You Don’t Want to Fail
A Japanese business tycoon has identified three habits commonly seen in people who are destined to fail.

What Raw Garlic Can Do for Your Health May Surprise You
What Raw Garlic Can Do for Your Health May Surprise You

Doctors Warn Parents After 5-Year-Old Dies From Late-Stage Can.cer
Doctors Warn Parents After 5-Year-Old Dies From Late-Stage Cancer

Your hands can reveal li.ver trouble — don’t ignore these shocking signs
Your hands can reveal li.ver trouble — don’t ignore these shocking signs

Sometimes, the strongest protection starts right on your balcony:
Sometimes, the strongest protection starts right on your balcony:

2 Tablespoons of This and You’ll Notice Incredible Results For Your Digestive Problems....
2 Tablespoons of This and You’ll Notice Incredible Results For Your Digestive Problems....
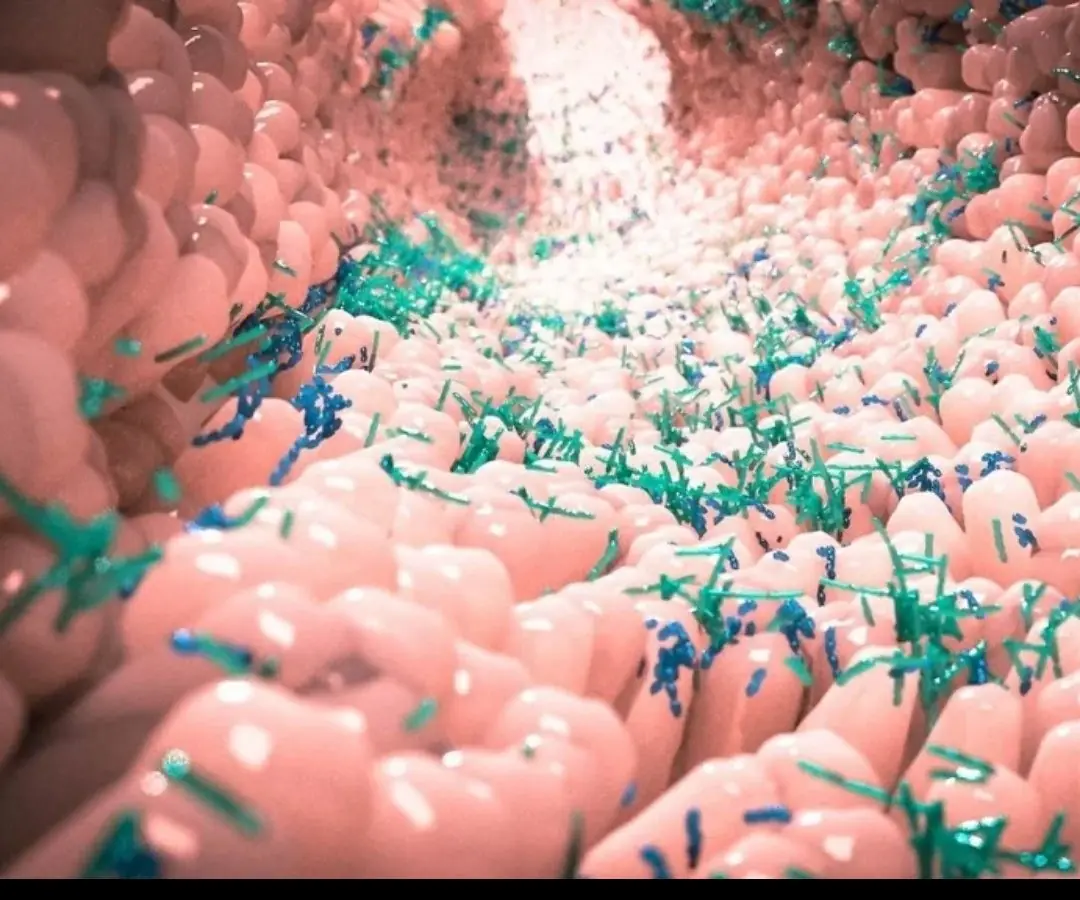
Twin Study Reveals Gut Microbiome's Role in Multiple Sclerosis Development.....
Twin Study Reveals Gut Microbiome's Role in Multiple Sclerosis Development.....

These “Healthy” Vegetables Could Actually Increase Canc:er Risk — Experts Warn to Avoid
These “Healthy” Vegetables Could Actually Increase Canc:er Risk — Experts Warn to Avoid

3 Foot Warning Signs That Could Indicate Serious Internal Organ Issues
3 Foot Warning Signs That Could Indicate Serious Internal Organ Issues

Bathing at the Right Time Could Reduce Stroke Risk — Here’s When
Bathing at the Right Time Could Reduce Stroke Risk — Here’s When
These 8 bathroom signs might seem harmless—but they could point to cancer
These 8 bathroom signs might seem harmless—but they could point to cancer

8 Signs You’re Mentally Exhausted — And Why Ignoring Them Can Cost You More Than You Think
Here are eight warning signs that your mind may be running on empty, and why taking them seriously matters.