
Onions: A Common Ingredient – Should You Eat Them Raw or Cooked?
Onions: A Common Ingredient – Should You Eat Them Raw or Cooked?
Onions are a staple ingredient in many kitchens worldwide, adding flavor and depth to countless dishes. However, a common debate arises: Is it better to eat onions raw or cooked? Both options offer unique benefits and drawbacks, so let’s explore the differences.

Benefits of Eating Raw Onions
Raw onions are packed with vitamins, minerals, and antioxidants that offer numerous health benefits. Here’s why you might want to eat them raw:
- Rich in Antioxidants – Raw onions contain quercetin, a powerful antioxidant that helps reduce inflammation and boost immunity.
- Good for Heart Health – Eating raw onions may help lower blood pressure and cholesterol levels, reducing the risk of heart disease.
- Supports Digestion – Onions are a great source of prebiotics, which promote gut health by feeding beneficial bacteria in the digestive system.
- May Reduce Blood Sugar Levels – Some studies suggest that raw onions help improve insulin function, benefiting people with diabetes.
Drawbacks of Eating Raw Onions
Despite their benefits, raw onions aren’t for everyone:
- Strong taste and smell – Their pungent odor can cause bad breath.
- Can cause digestive discomfort – Some people experience bloating or gas when consuming raw onions.
- Can irritate sensitive stomachs – Those with acid reflux or irritable bowel syndrome (IBS) may find raw onions too harsh.
Benefits of Eating Cooked Onions
Cooking onions changes their flavor, texture, and nutritional composition. Here’s why some prefer them cooked:
- Milder taste – Cooking reduces the sharpness, making onions sweeter and more palatable.
- Easier to digest – Heat breaks down some of the compounds that can cause bloating and discomfort.
- Still rich in nutrients – While cooking may reduce vitamin C levels, onions retain many important antioxidants and beneficial sulfur compounds that support health.
Drawbacks of Eating Cooked Onions
- Reduced antioxidant levels – Some heat-sensitive nutrients and compounds are lost during cooking.
- Less prebiotic content – Cooking lowers the fiber content that benefits gut health.
So, Which Is Better?
The answer depends on your preference and health needs. If you want maximum nutrients and antioxidants, raw onions are the best choice. However, if you prefer a milder taste and easier digestion, cooked onions are a great alternative.
For the best of both worlds, include both raw and cooked onions in your diet! Use raw onions in salads and sandwiches, while adding cooked onions to soups, stir-fries, and roasted dishes. No matter how you enjoy them, onions are a flavorful and healthy addition to any meal.
News in the same category

Mix White Salt With Fabric Softener: A Simple Household Trick That Saves Money and Solves Multiple Problems

Installing an Air Conditioner: Avoid These 4 Locations to Protect Your Family’s Health

Don’t Throw Away Rice-Washing Water: 5 Surprisingly Useful Kitchen Benefits

Why should garlic be placed at the head of the bed when sleeping at night?

Cook rice better just this

Remove this from your room immediately!! Lung can.cer!

Why Should Couples Over 50 Consider Sleeping in Separate Beds? Those Who’ve Experienced It Share 3 Key Benefits
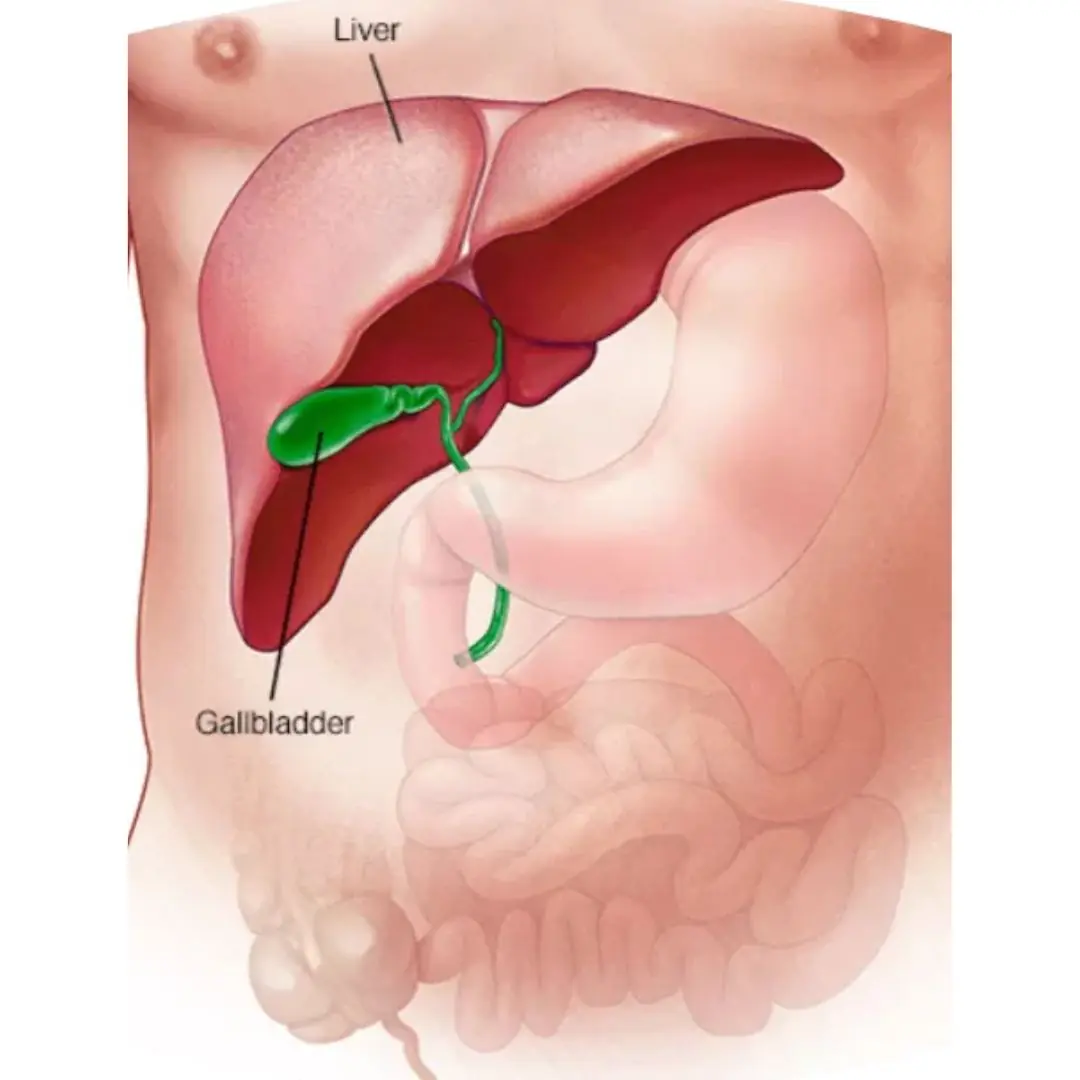
Gallbladder removal: what happens next and 3 risks to watch for

Why do Japanese people wear socks to sleep regardless of winter or summer?

Man develops 'pork worms' in his brain after years doing this specific cooking habit
People with calcium deficiency often experience these 7 signs. Check now to see if you have them

Should you keep the bathroom door open or shut when it’s not in use? Surprisingly, many people get this wrong.

Grapefruit Is Healthy and Generally Safe, but These 4 Groups Should Avoid It

Revealed: The 10 Most Toxic Foods in the World — Some Are Shockingly Familiar

3 Effective Ways to Prevent Snakes From Entering Your Home
A Simple, Safe Way to Repel Rats Using Only Rice

The reason dogs always behave this way is because

The Vegetable Once Reserved for Emperors — Now Found in Everyday Gardens

The Overlooked Plant Said to Support Health in Many Ways
News Post

Many people cook rice every day—but still get it wrong: 4 simple tips for tastier rice and better digestion

Two vegetables considered “natural remedies” for headaches—eat them and sleep soundly through the night

The 4 earliest warning signs the body sends as a “cry for help” for cerv.ical can.cer—sadly, many women overlook them
More and more people are developing kid.ney failure. U.S. experts warn: Eating too much of these 4 foods is especially harmful to the kid.neys and should be limited immediately

4 Foods to Eat on an Empty Stomach in the Morning That May Support Digestion and Long-Term Health

Just follow these 4 steps and pork will always turn out tender, juicy, and never tough

Yellow Tongue: A Small Sign That May Signal Serious Health Problems

Pharmacist shares major wa:rning sign in heels of foot that could be symptom of serious condition

5 Common Drinking-Water Mistakes That Can Damage Your Liver and Kidneys

Cancer May Be Silent at First: 8 Warning Signs You Should Never Ignore When Using the Toilet
Mix White Salt With Fabric Softener: A Simple Household Trick That Saves Money and Solves Multiple Problems
Breakthrough: Scientists discover a way to turn can.cer cells back into normal cells

Installing an Air Conditioner: Avoid These 4 Locations to Protect Your Family’s Health

American Nutrition Experts Praise Avocados as a Top Heart-Healthy Fruit

Seafood Bisque with Crab, Shrimp, and Lobster

Why Your Throat Feels Mucusy: The Real Reasons Behind That Sticky Sensation
Does Reheating Rice Cause Cancer? What You Should Really Know
Losing Both Kidneys Before 30: A Wake-Up Call About Kidney Health
An Overlooked Flower That Supports Liver and Kidney Health
