
Growing Tomato Plant From Tomato Slice Time Lapse

Tomatoes are one of the most popular and rewarding plants to grow at home. While most gardeners start from seeds or seedlings, did you know you can actually grow a tomato plant directly from a slice of tomato? This simple and fascinating method is not only fun but also a great way to understand plant growth from start to finish.
In this article, we’ll explore the step-by-step process of growing a tomato plant from a slice of tomato, highlighting what you can expect to see in a time-lapse journey from seed to sprout and beyond.
Why Grow Tomatoes from a Slice?
Using a tomato slice to grow plants is an easy and natural way to propagate tomatoes without buying seeds. Each slice contains seeds and pulp rich in nutrients, which provide the perfect environment for germination and early growth. This method is perfect for beginners, kids, or anyone interested in watching plants grow quickly and visually.
Step-by-Step Guide
Step 1: Choose a Ripe Tomato
Select a fresh, ripe tomato with fully developed seeds. The better the tomato, the higher the chances of successful germination.
Step 2: Prepare the Tomato Slice
Cut a thin slice of tomato, about 1/4 inch thick, making sure the seeds are visible. The slice should include the seed gel around the seeds to aid germination.
Step 3: Place on Growing Medium
Place the tomato slice on moist soil or a paper towel inside a shallow container. Ensure the soil is well-draining and kept consistently moist but not waterlogged.
Step 4: Provide Proper Conditions
Cover the container with a clear plastic lid or plastic wrap to maintain humidity. Place it in a warm, sunny spot or under a grow light to encourage sprouting.
Step 5: Watch the Time-Lapse Growth
Over the next several days to weeks, you will observe seeds germinating, tiny roots developing, and shoots emerging from the tomato slice. A time-lapse video of this process beautifully captures the dynamic growth and transformation from slice to seedling.
Step 6: Transplant Seedlings
Once the seedlings grow several true leaves and become sturdy enough, carefully transplant them into individual pots or your garden. Continue to provide water, sunlight, and nutrients for healthy growth.
What You’ll See in a Time-Lapse Video
-
Seed Germination: Seeds swell and crack open as roots begin to emerge.
-
Shoot Emergence: Tiny green shoots break through the soil surface.
-
Leaf Development: First leaves (cotyledons) appear, followed by true leaves.
-
Growth Acceleration: Stems grow taller, and more leaves develop, showing the plant’s vigor.
Watching this process in fast motion reveals the incredible life cycle of plants and is a wonderful educational tool.
Benefits of Growing from a Tomato Slice
-
Easy and Cost-effective: No need to buy seeds or seedlings.
-
Educational: Great for kids and beginners to learn about plant biology.
-
Sustainable: Recycles food scraps and reduces waste.
-
Rewarding: Experience the joy of growing plants from everyday kitchen scraps.
Final Tips
-
Keep the soil moist but avoid overwatering to prevent rot.
-
Provide plenty of light to support healthy growth.
-
Be patient - germination can take from a few days to a couple of weeks.
-
Once transplanted, care for your plants with regular watering and fertilization.
Growing tomato plants from a tomato slice is a fascinating and simple way to connect with nature and enjoy fresh, homegrown tomatoes. Whether you document the journey with time-lapse photography or simply watch them grow day by day, it’s an experience full of wonder and satisfaction.
Happy gardening!
News in the same category


The husband slapped his wife in front of his friends to show off — but her act of revenge left everyone shocked and speechless

10 Clever Ways to Reuse Lemon Seeds at Home

Unlocking the Secret Health Benefits of Common Mallow: Nature’s Wonder Herb for Wellness

Essential Knowledge for Growing Cassava Successfully

Growing Kale: Planting, Care, and Harvesting Tips

Just 1 Cup Makes Peace Lilies Bloom with So Many Flowers
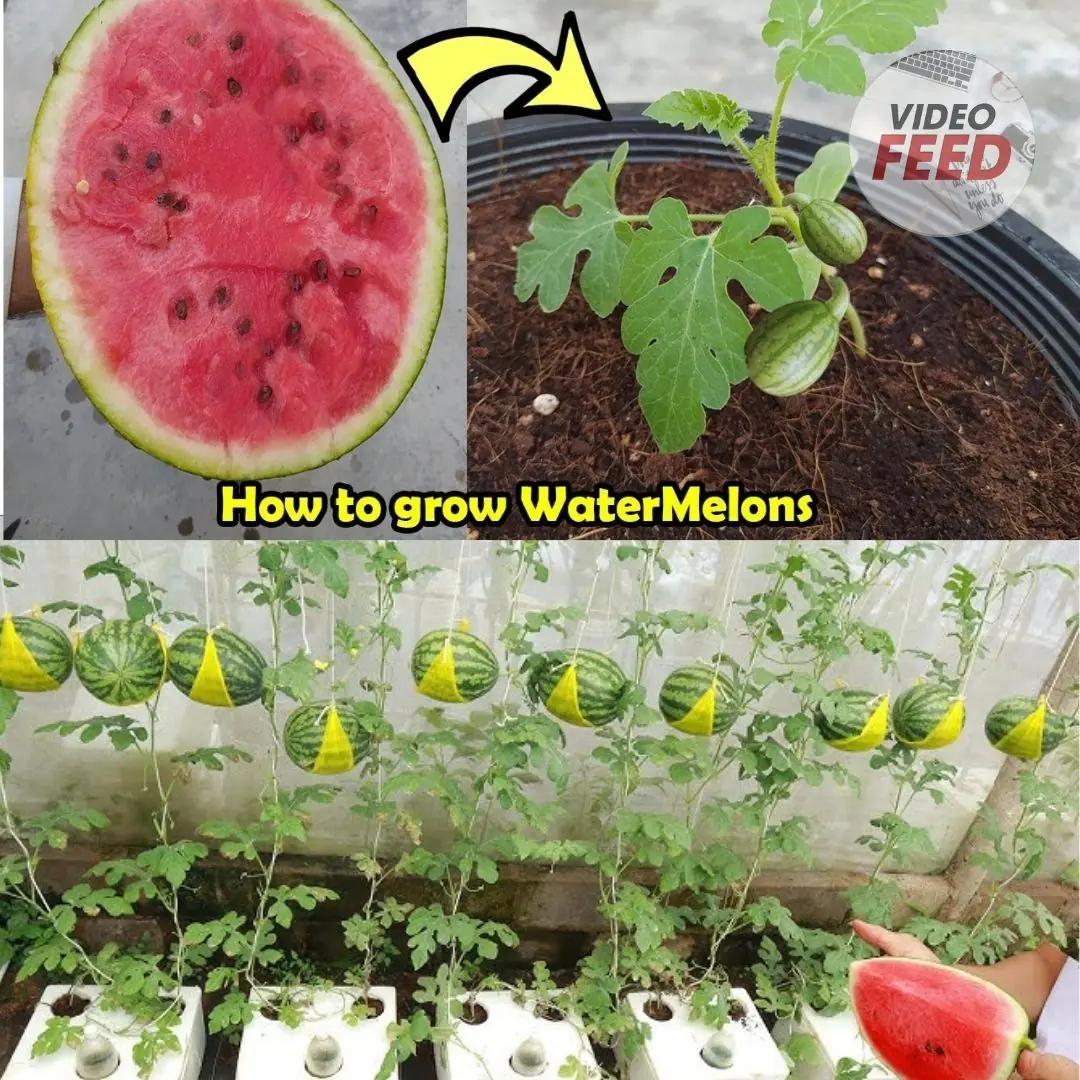
How to Grow Watermelons at Home: A Guide for Small Spaces & Balconies

How to Grow a Banana Tree at Home and Never Buy Bananas Again

Here’s How to Grow Calamansi at Home — No Farm Needed

How to grow tulips indoors – a step-by-step guide to forcing these beautiful bulbs

How to Grow Habanero Peppers in Pots

Grow These 5 Garden Beans This Summer

Why Asians Are Rushing to Grow This “Miracle Tree”: Heals Like Medicine, Sells Like Gold

How to Grow and Care for Dieffenbachia

How to Grow and Care for Phalaenopsis Orchids Indoors

Portulaca in Pots: The Complete Guide to Growing Colorful & Drought-Tolerant Flowers Outdoors

10 Tips for Growing Superb Spring Spinach

How to Make Rose Petal Lemonade – A Refreshing Homemade Drink

How to Grow Carrots at Home in Containers Starting with a Single Carrot
News Post

If you drink lemon water every morning, this is what happens to your body

I truly am bothered by these!

Stanford researchers identified a specific circuit within the amygdala

Searching for Truth in Bones: The Mysterious Relics of Mary Magdalene

Coconut–Pineapple Chili Island Ja
This One Superfood Could Tackle Major Health Issues—Here’s What You Need To Know
If Cancer Is Developing in the Body, These 3 Nighttime Signs Often Appear — But Many People Ignore Them

36-Year-Old Teacher Dies From Diabetes Doctors Say Was Triggered By Everyday Foods

Husbands With These 2 Bad Habits May Put Their Wives at Higher Risk of Breast Cancer - Stop Them Now Before They Harm The Whole Family

Discover Love in the Little Things: Everyday Connections

The Vegetable Known as a “Bedroom Superfood”: Beneficial for Both Men and Women
Your Appendix May Be in Trouble: 4 Warning Signs
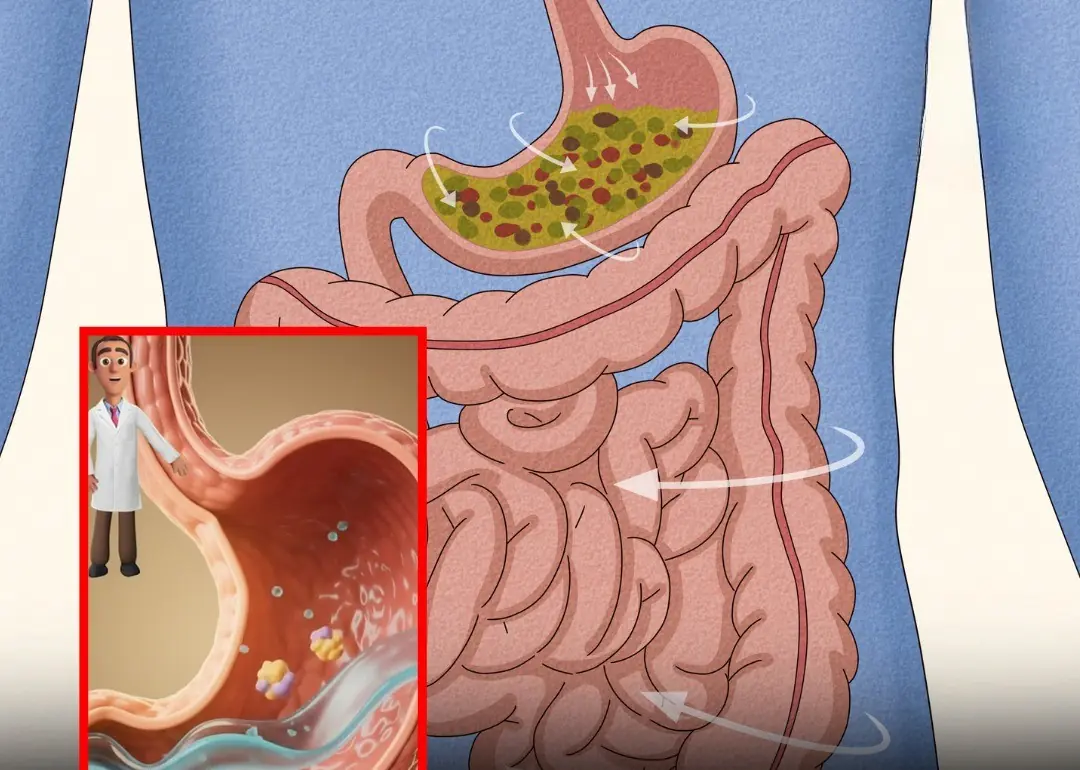
Tips to Stop Stomach Growling

Your Thyroid Is Begging You to Stop Eating These 6 Foods Immediately!

Feng Shui masters say these 4 apartment floors bring wealth and stability — are you living on one of them?
These 4 morning symptoms may be the earliest warning of lung cancer — don’t overlook them

Doctors rarely explain it, but constant phlegm often comes down to 4 overlooked causes...
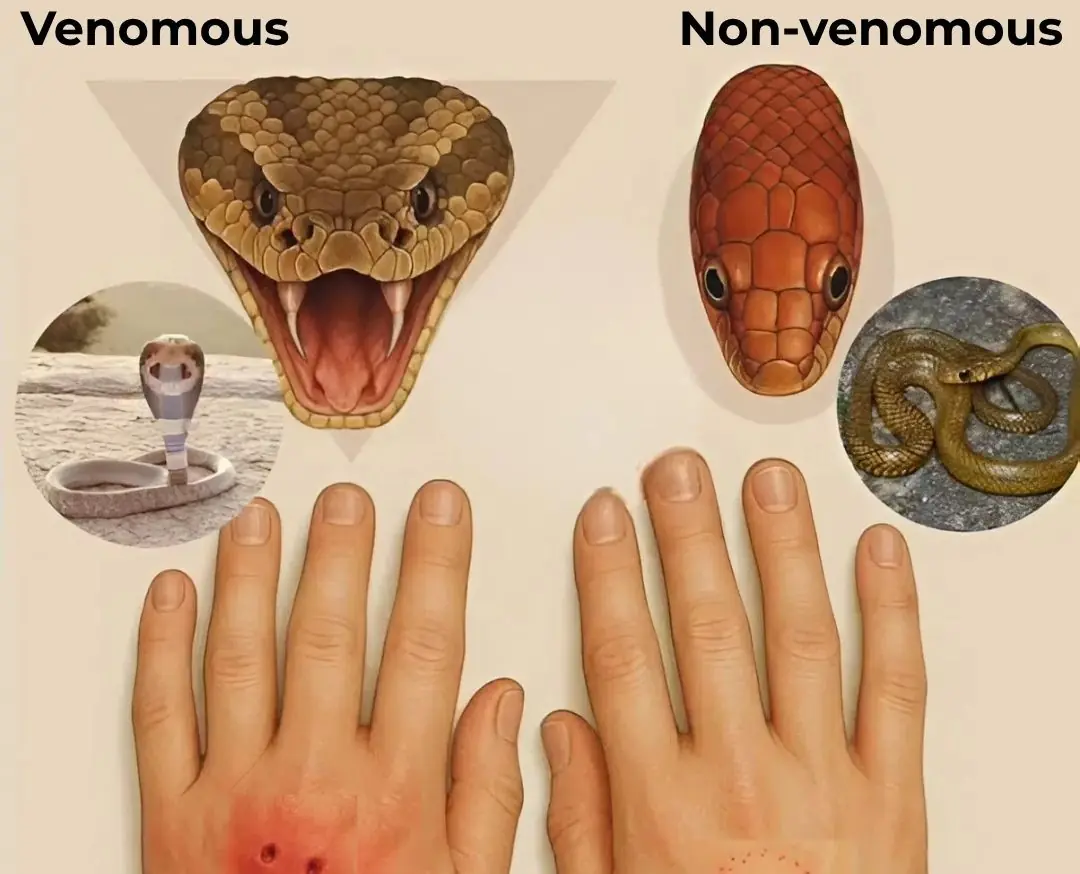
Snake bi.te - don't panic, do the following
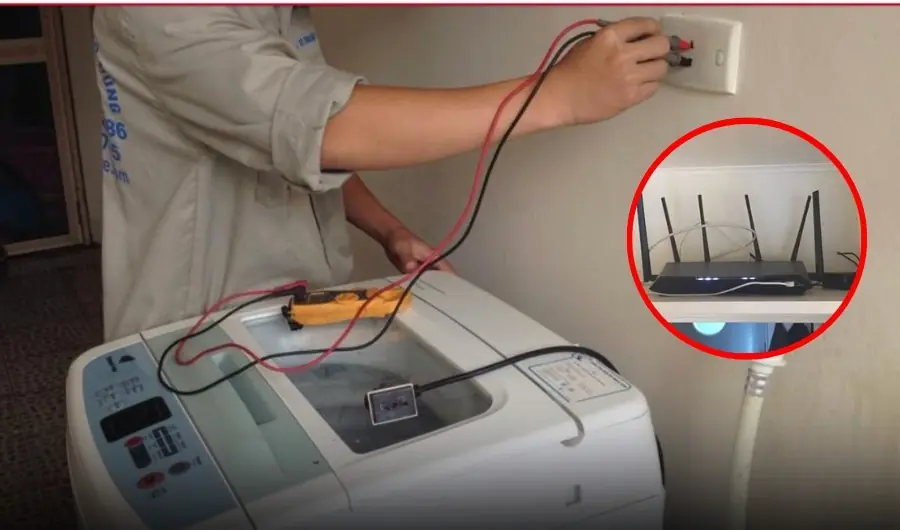
7 household items you should NEVER unplug. Number 3 shocks everyone
