
The Truth About Removing Tartar at Home: What Experts Want You to Know
Home remedies to remove tartar dental
New treatment shrinks d.e.a.dly brain t.u.m.o.r by half – a real breakthrough!

A 62-year-old engineer has seen his deadly brain tumor shrink by half, thanks to a groundbreaking new treatment. Glioblastoma, a type of brain cancer that is both aggressive and often fatal, has always been a huge challenge for doctors and patients. But a new clinical trial is offering hope, showing promising results that could change the way we treat cancer. The engineer, who was given little hope, experienced a significant reduction in his tumor size in just a few weeks. This could be the beginning of a new way to fight one of the toughest cancers.

What is Glioblastoma?
Glioblastoma is the most common and aggressive form of brain cancer in adults. It starts in the glial cells, which support nerve cells, and grows quickly, spreading into nearby brain tissue. This makes it very hard to remove entirely through surgery. Glioblastomas are known for being fast-growing and often come back after treatment. The outlook for patients is poor, with survival rates remaining low even after surgery, radiation, and chemotherapy.
Current Treatment Options
Doctors often try to remove as much of the tumor as possible, but since glioblastomas grow into surrounding brain tissue, complete removal is usually impossible. After surgery, patients typically go through radiation and chemotherapy to kill any remaining cancer cells. However, glioblastomas often return, showing the need for new, more effective treatments. One exciting new approach is a clinical trial at University College London Hospitals NHS Foundation Trust (UCLH). This trial uses targeted radiation therapy directly into the tumor to kill cancer cells without damaging healthy brain tissue.
The Trial and Treatment
The treatment involves a small device called an Ommaya reservoir, implanted under the skin on the scalp. This device connects to the tumor and delivers a radioactive drug directly to the cancer cells. Paul Read, the 62-year-old engineer from Luton, was the first to try this treatment. Diagnosed with glioblastoma in December 2023, Paul underwent surgery, radiation, and chemotherapy, but by July, his tumor had started to grow again. He then joined the trial, which led to a 50% reduction in his tumor size in just a few weeks. Paul was amazed by the results, calling it a “lifeline.” Aside from feeling a little tired, he experienced minimal side effects.
The Expert’s Perspective
Dr. Paul Mulholland, a UCLH oncologist, is optimistic about the trial's potential. He believes this method could change the way brain cancers are treated. Since glioblastomas don’t spread outside the brain, targeting the tumor directly with radiation makes sense. Experts like Dr. Simon Newman, chief scientific officer at The Brain Tumour Charity, also support the trial, seeing it as a step forward in the fight against this challenging cancer.
Looking to the Future
The promising results of the trial are giving hope to patients and doctors alike. Dr. Mulholland plans to increase the radiation dose and combine the treatment with immunotherapy, which trains the body’s immune system to fight cancer. This could improve survival rates and quality of life for glioblastoma patients. If successful, this treatment could lead to new standards of care for this type of cancer, offering hope to many others in the future.
For Paul, the trial has been more than just a treatment—it's been a beacon of hope. He remains positive, even if the treatment doesn’t work for him long-term, believing it could help others. This trial shows the potential of new cancer treatments and represents a step toward better outcomes for people with glioblastoma.
This new treatment approach offers hope not just for Paul, but for all glioblastoma patients. The success of this trial could mark a turning point in how we treat aggressive cancers, and the future looks brighter with the possibility of combining this treatment with immunotherapy. The dedication of doctors, researchers, and patients is bringing us closer to changing the future of cancer care.

Home remedies to remove tartar dental

10 signs that a man shows when he's in love

Managing blood sugar does not have to rely solely on medication or strict dietary deprivation.

Why one simple bedtime habit could quietly save your life
Intelligence alone cannot prevent failure without discipline.
7 reasons why a man gets bored with a woman

Not all cheating looks the same—and some forms feel invisible.

In modern life, the moments before bedtime for many couples often pass in a rush.

One of the most common reasons?

How to Recognize When a Parent Is in the Final Stage of Life and Prepare with Care

Subtle behavioral shifts can reveal deeper relationship secrets.

Bananas are undeniably nutritious.

Why under-stair bathrooms may cost more than you think

11 Important Facts About Sunflower Seeds You Should Know Before Snacking
Most people still don't know what the acronym "WC" used in restrooms stands for

A compliment boosts your mood. A critical comment ruins your day. A delayed reply triggers self-doubt. Sound familiar?

This is a wake-up call for parents who are too quick to push their children into marriage.

People with low emotional intelligence (EQ) often send these four types of messages.

Why you should leave the bathroom light on when staying in a hotel or motel?

Magnesium is an essential mineral in the human body, playing a critical role in over 300 enzymatic processes.

Beer and salt together can help tackle many everyday household issues.
A simple daily drink gaining attention for heart and artery health

Shared daily habit raises health concerns after couple’s diagnosis

Who should avoid ginger? Five conditions that require caution.

5 subtle cancer warning signs experts say you should never ignore

Hidden daily habit leads to serious nasal fungal infection case

A simple dishwashing habit may pose hidden health risks at home.

Sweet Potatoes: A Nutritious Food for Health and Taste




According to Mrs. Wang's account, before being hospitalized, she ate a bowl of bitter gourd soup.


Home remedies to remove tartar dental
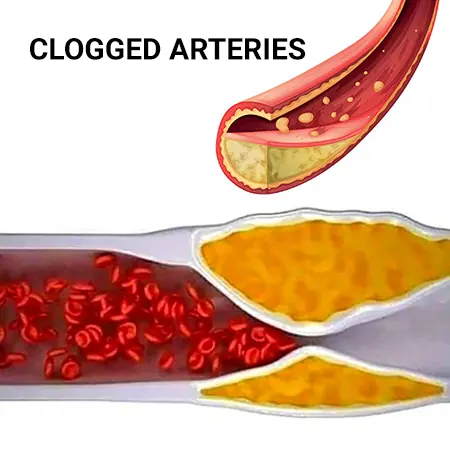
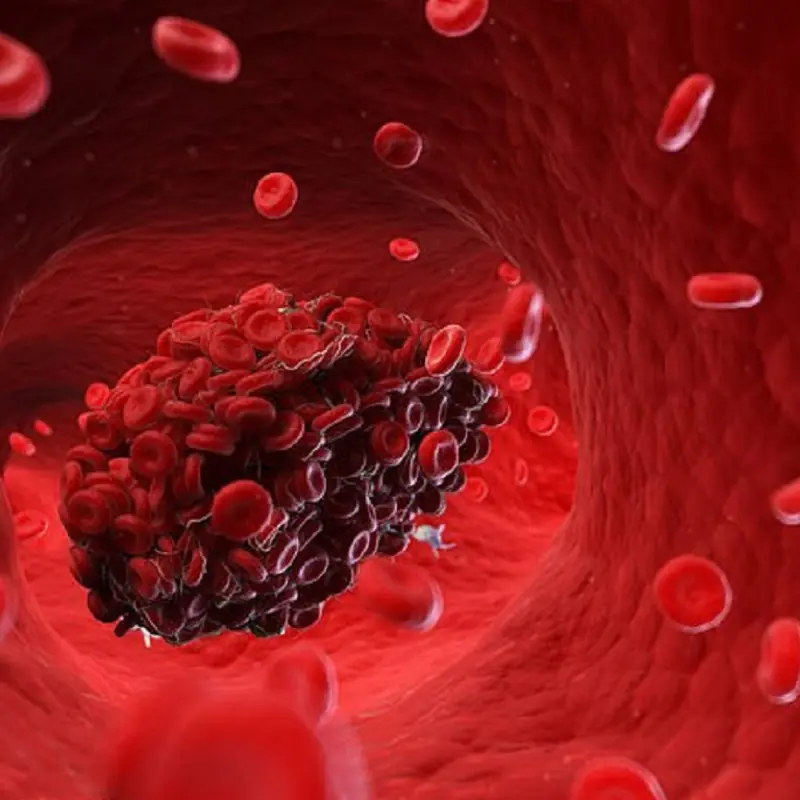
Clogged arteries rarely happen overnight. Instead, they develop slowly as fat, cholesterol, and other substances build up inside blood vessels, a process known as atherosclerosis.

10 signs that a man shows when he's in love

I was ashamed of my mom’s old car until the night it saved my dad

I almost sold my late father’s house to a stranger — until my son asked me one question that changed everything

The empty chair at the table said more than words ever could

We pretended everything was fine until it wasn’t