
Subtle Heart Attack Symptom Many Women Miss Without Realizing
Heart disease in women can often emerge silently, yet the subtle warning signs are usually there. However, they just do not always appear in the dramatic way that many people imagine. A story recently shared by a hospital worker on Reddit described a colleague who came in with jaw and neck pain that shifted into chest discomfort. Soon after arriving at the emergency desk, she collapsed and went into cardiac arrest. The team resuscitated her, placed stents, and she survived. The experience haunted the poster, who admitted they never knew jaw and neck pain could signal a heart attack in women.
In this article, we will learn more about that story and then find out what research has to say. We will explore the early signs of heart attack in women, especially those that do not match the familiar picture of crushing chest pain. We will also learn why jaw and neck pain matter, why women so often have subtle symptoms, and how delays in care increase risk. Ultimately, the goal is simple. Women should recognize heart attack symptoms in women early enough to act and protect their hearts.
The Reddit story that exposed a subtle warning sign

The original Reddit thread came from a biomedical and pathology student working in a hospital. They described an ordinary admin staff member who walked into the emergency department because of jaw and neck pain that soon crept into her chest. Within minutes she collapsed in front of the triage desk and went into cardiac arrest. Staff performed CPR, moved quickly, and she lived long enough to receive stents and begin recovering. The poster wrote, “I genuinely didn’t know that jaw/neck pain is a common warning sign for heart attack in women.” That single line captured how even people in medical settings can overlook early signs in women.
Many readers felt a similar jolt of recognition when they read the thread. Clinicians and nurses filled the comments with examples of these subtle danger signs. Some described women who blamed exhaustion on long work hours, and nausea on a simple stomach bug. Others recalled patients who had back or neck pain for days before finally seeking help because breathing became difficult. The discussion showed how personal stories can shift public awareness and make statistics about heart disease in women feel real.
Why heart attack symptoms in women often look different

Most people still picture a man clutching his chest and falling to the floor. In daily life, heart attack symptoms in women frequently unfold in a quieter, more drawn out way. Many women describe discomfort that appears gradually and seems manageable at first. Health agencies report that millions of women live with some form of heart disease and that it causes about 1 in 5 female deaths. Those numbers underline how vital it is for women to understand how their symptoms can differ from men’s.
Cardiology experts have repeatedly shown that women are more likely to describe shortness of breath, nausea, vomiting, or back and jaw pain. Chest discomfort, when present, may feel milder or less focused. Patient education materials from major heart organizations list pain or discomfort in one or both arms, the back, neck, jaw, or stomach as key warning signs. These sensations do not always feel obviously cardiac. They can be vague, shifting, or intermittent. That makes it easy to blame them on muscle strain, anxiety, or indigestion, which quietly delays urgent care
How jaw and neck pain connect back to the heart

Jaw and neck pain can seem far removed from the heart, yet the connection lies in shared nerve pathways. When blood flow to part of the heart muscle drops, nerves in the chest send distress signals. The brain sometimes misinterprets these signals and experiences pain in distant areas. This phenomenon, called referred pain, explains why some people feel discomfort in the left arm, upper back, throat, or jaw instead of the chest. Women often describe this pain as heaviness, pressure, or tightness, not as sharp stabbing pain.
Major heart centers note that a heart attack can cause pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth, or upper belly. Research on craniofacial pain has found that pain in the head or face can be triggered by reduced blood flow to the heart. In a subset of patients, craniofacial pain was even the only warning sign during ischemia. These findings show why new, unexplained jaw or neck pain, especially in someone with risk factors, deserves careful attention. It should not simply be written off as stress or a minor pulled muscle.
What studies reveal about early warning signs in women

Researchers have worked for years to understand early, or prodromal, heart attack symptoms in women. One landmark study led by Jean McSweeney surveyed hundreds of women who had experienced a heart attack. Almost all of them remembered at least one warning symptom during the month before the event. Many never realized those sensations were related to their hearts. The most common early complaints included unusual fatigue, sleep disturbance, and shortness of breath. Classic chest discomfort appeared far less often during that early phase.
Later summaries of McSweeney’s work note that many women did not have chest pain even during the actual heart attack. Others reported discomfort in the arms, back, jaw, or shoulders, along with anxiety and restless sleep. This pattern paints a picture of heart disease in women that unfolds gradually, with symptoms that feel scattered. A woman might feel deeply tired, sleep poorly, and notice odd pains, yet still see herself as basically healthy. Without clear information, she has little reason to link those changes to a developing heart attack.
The risk of having no chest pain during a heart attack

One key reason heart attack symptoms in women are missed is the absence of chest pain. A large registry study led by John Canto examined more than 1 million patients with heart attacks. The researchers found that women were more likely than men to arrive at the hospital without chest pain. Those patients without chest discomfort had significantly higher in-hospital death rates. The numbers revealed a hidden danger. When symptoms do not match expectations, everyone hesitates longer.
Further work from Canto’s group and others showed that younger women without chest pain face a particular risk. Some analyses concluded that women not only arrive with less typical symptoms, but also suffer higher in-hospital mortality compared with men. Cardiologists have warned that women’s complaints may be taken less seriously when they do not include clear chest pain. A woman with jaw pain, fatigue, and breathlessness may be triaged more slowly or sent for non-urgent tests. Those lost minutes can close the window for treatments that protect the heart muscle and improve survival.
Why women often delay seeking help

Studies also show that many women delay calling emergency services, even when symptoms are concerning. In interviews with heart attack survivors, women often describe misreading early warning signs. They connect fatigue to busy schedules or indigestion to a heavy meal. A qualitative study from Iran found that participants were largely unaware that their early symptoms were related to heart disease. They viewed their discomfort as minor, temporary, and not urgent.
Systematic reviews of prodromal symptoms in women echo these themes across different countries. Women frequently experience fatigue, sleep disturbance, anxiety, and unexplained pain in the weeks leading up to an acute coronary event. Yet they often underestimate the threat. Many feel reluctant to “make a fuss” or disrupt family routines. Others delay because of responsibilities at home or work. These social and cultural pressures help explain why women often arrive at the hospital later, when heart damage is already extensive, and options are more limited.
Sorting heart attack symptoms from heartburn or anxiety

Distinguishing everyday discomfort from a true emergency is challenging for anyone. Many women living with heart disease also have reflux, musculoskeletal pain, panic symptoms, or anemia. Each of these conditions can cause chest tightness, throat discomfort, or breathlessness. That overlap can blur the picture and create doubt. However, cardiology guidelines generally advise that new, unexplained, or rapidly worsening symptoms should be treated as cardiac until proven otherwise, especially when risk factors are present.
Educational materials from major heart organizations urge people to look at patterns, not single sensations. Symptoms are more worrisome when they appear suddenly, intensify over minutes, or spread from the chest into nearby areas like the arm, back, neck, or jaw. Many experts advise calling emergency services rather than driving yourself if you suspect a heart attack. Paramedics can begin treatment on the way and alert the hospital before arrival. It is always safer to have a worrying episode checked and find nothing serious than to wait at home while a heart attack evolves.
Protecting yourself from heart disease in women

Recognizing trouble matters, yet prevention remains just as important. Public health agencies estimate that tens of millions of women live with some form of heart disease. It continues to cause about 1 in 5 female deaths in countries like the United States. Cardiologists describe heart disease as the leading killer of women and stress that it is not a condition limited to older men. Younger and middle aged women, especially those with risk factors, also face significant danger.
The encouraging news is that many major risk factors can improve over time. Smoking, high blood pressure, elevated cholesterol, diabetes, excess body weight, and low physical activity all increase the likelihood of a heart attack. Large reviews show that quitting smoking, treating blood pressure, managing blood sugar, and moving regularly each week can lower risk. Doctors also recommend routine checks of blood pressure and cholesterol, since both can rise silently. Lifestyle changes and medication, when needed, make the heart more resilient. Prevention cannot erase all risk, yet it often makes future events less severe and more survivable.
When to act immediately and how to advocate for care

Experts in emergency cardiology keep returning to one core message. Time to treatment is one of the strongest predictors of survival during a heart attack. Heart organizations remind people that heart disease still tops the list of causes of death, even as treatments improve. This is why clinicians continue to use the phrase “time is muscle.” Every minute of delay allows more heart tissue to suffer from poor blood flow.
If you or someone nearby has sudden chest discomfort, pressure, or pain that lasts more than a few minutes, urgent action is needed. The same applies if there is unexplained pain in the arm, back, neck, jaw, or upper belly, especially when combined with breathlessness, sweating, or nausea. Calling emergency services is safer than driving, because trained teams can start care immediately. When you arrive at the hospital, clear language can help. Saying “I am worried this could be my heart” signals to staff that cardiac causes need to be ruled out quickly, even if symptoms seem atypical.
A final word: listen to the subtle signals

The story that began on Reddit shows how small symptoms can hide major danger. A woman with jaw and neck pain walked into the emergency department on her own. Soon afterward, she collapsed and needed resuscitation. The original poster admitted, “I genuinely didn’t know that jaw/neck pain is a common warning sign for heart attack in women.” Their shock revealed a gap in public understanding. Many readers likely realized they shared that same blind spot.
Work by researchers like Jean McSweeney, John Canto, and Mariano Kreiner shows a consistent pattern. Women often experience unexplained fatigue, disturbed sleep, and spreading pain in the arms, back, or jaw before a heart attack. They are also more likely than men to arrive without chest pain, which increases the risk of misdiagnosis and poorer outcomes. If you notice new, unusual, or escalating discomfort in these areas, especially when you have known risk factors, it is wise to get checked. Listening to those quiet signals does not mean living in fear. It simply means giving your heart the same careful attention you would offer to someone you love.
News in the same category


Oxford research finds a drink that helps “ward off” colon can.cer

Doctor shares what it means if you always need to poo immediately after you eat (it isn’t just IBS)

Suddenly something feels stuck in your throat - then a small lump comes out. What is it?

Leaf of life – The healing plant growing in your backyard

6 Gentle Drinks for People with Insomnia - Plus Simple Habits That Help You Sleep Better Naturally
The link between ovarian can.cer and breast can.cer

Men Who Neglect This Crucial Practice Face 45% Higher Risk of Prostate Cancer

Warning: Pain in These 3 Spots Might Be a Sign of Lung Ca.ncer

Your Legs Could Be Sending a Pancreatic Cancer Warning — 4 Signs to Watch

20-Year-Old Teacher Dies of Liver Can.cer Doctors Say Unusual Odors in 3 Areas May Be a Warning Sign of Li.ver Failure

Sweet Potatoes Aren’t Always “Healthy” the Way You Think — Here’s Why

5 Dan.gerous Times You Should Avoid Showering - For the Sake of Your Health

Amazing Health Benefits of Chicken Feet You Should Know

Sweet potato lovers should read this article - it will change your life Knowing this now is not too late!

The Hidden Power of Orange Peels: A Forgotten Treasure You Shouldn’t Throw Away

The Food That Rejuvenates Skin from the Inside: One Bowl Is Better Than 10 Face Masks

5 early can.cer symptoms experts say are commonly ignored

Why Horse Chestnut Is So Effective for Swollen Legs
News Post

One week of coconut water on an empty stomach: A simple habit with big rewards

Oxford research finds a drink that helps “ward off” colon can.cer

Doctor shares what it means if you always need to poo immediately after you eat (it isn’t just IBS)

Suddenly something feels stuck in your throat - then a small lump comes out. What is it?

Leaf of life – The healing plant growing in your backyard

6 Gentle Drinks for People with Insomnia - Plus Simple Habits That Help You Sleep Better Naturally

The Cultural Meaning of Ankle Bracelets You May Not Know
The link between ovarian can.cer and breast can.cer

Strawberry Swiss Roll Cake (Strawberry Cream Roll)
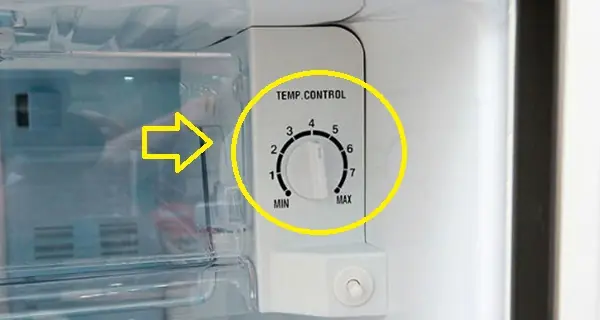
This small fridge button can significantly cut your electricity bill

Doctors Explain What Happens When You Eat Bananas Every Single Day

Men Who Neglect This Crucial Practice Face 45% Higher Risk of Prostate Cancer

Strawberry Crunch Cheesecake Cones

Crispy Fried Ice Cream with Strawberries & Chocolate Sauce

Warning: Pain in These 3 Spots Might Be a Sign of Lung Ca.ncer

Your Legs Could Be Sending a Pancreatic Cancer Warning — 4 Signs to Watch

20-Year-Old Teacher Dies of Liver Can.cer Doctors Say Unusual Odors in 3 Areas May Be a Warning Sign of Li.ver Failure

Sweet Potatoes Aren’t Always “Healthy” the Way You Think — Here’s Why
