One Year Before Death, the Body Often Shows 6 Warning Signs



Conversations about mortality are uncomfortable. Yet from a clinical standpoint, the human body often undergoes progressive physiological decline long before the final stage of life.
It is important to clarify:
There is no universal countdown clock. Not everyone experiences the same pattern. However, in cases involving chronic illness, advanced age, or terminal disease, healthcare professionals frequently observe predictable systemic changes months—sometimes a year—before the end of life.
Below are six commonly observed warning signs associated with late-stage decline. This information is educational, not diagnostic.
1. Persistent and Worsening Fatigue
Fatigue near end of life is not ordinary tiredness.
It is characterized by:
-
Profound lack of energy
-
Increased time spent sleeping
-
Minimal interest in activities
-
Limited responsiveness
As organ systems weaken—especially the heart, lungs, and kidneys—oxygen delivery and metabolic efficiency decline. The body begins conserving energy.
This fatigue is progressive and does not improve with rest.
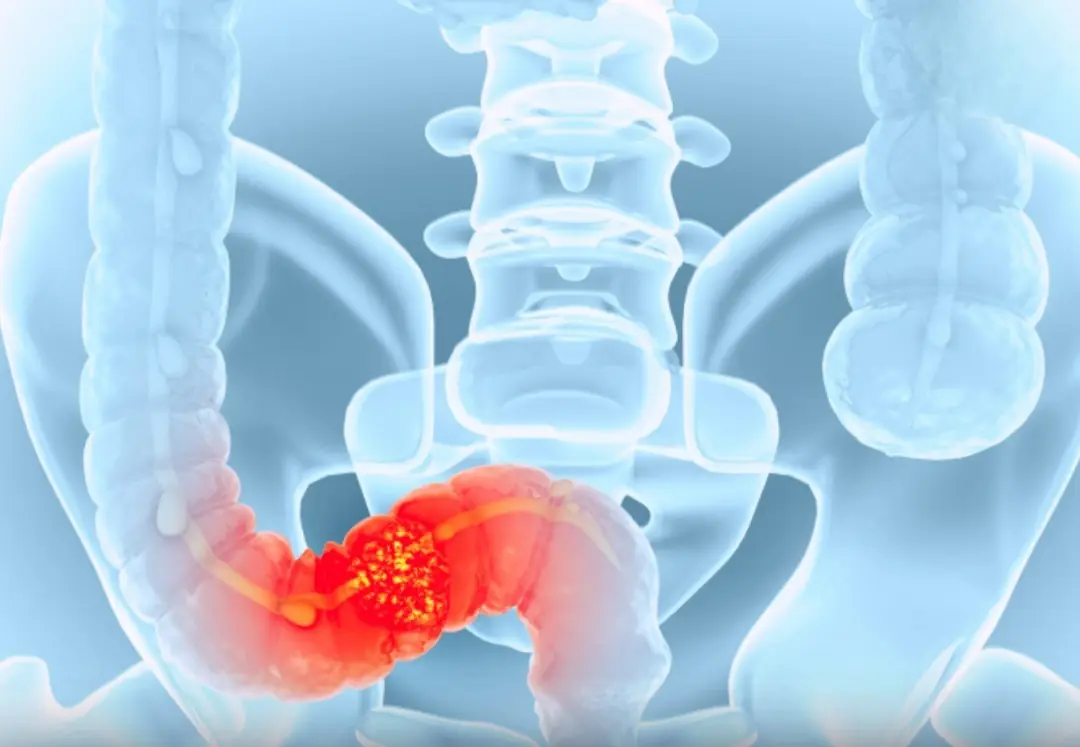
2. Loss of Appetite and Noticeable Weight Decline


Reduced appetite is one of the most consistent late-stage changes.
Why it happens:
-
Slowed metabolism
-
Digestive system slowdown
-
Reduced energy requirements
-
Hormonal shifts
The body gradually requires less fuel. Forced feeding in this stage can sometimes cause discomfort rather than benefit. In palliative medicine, the focus often shifts from caloric intake to comfort.
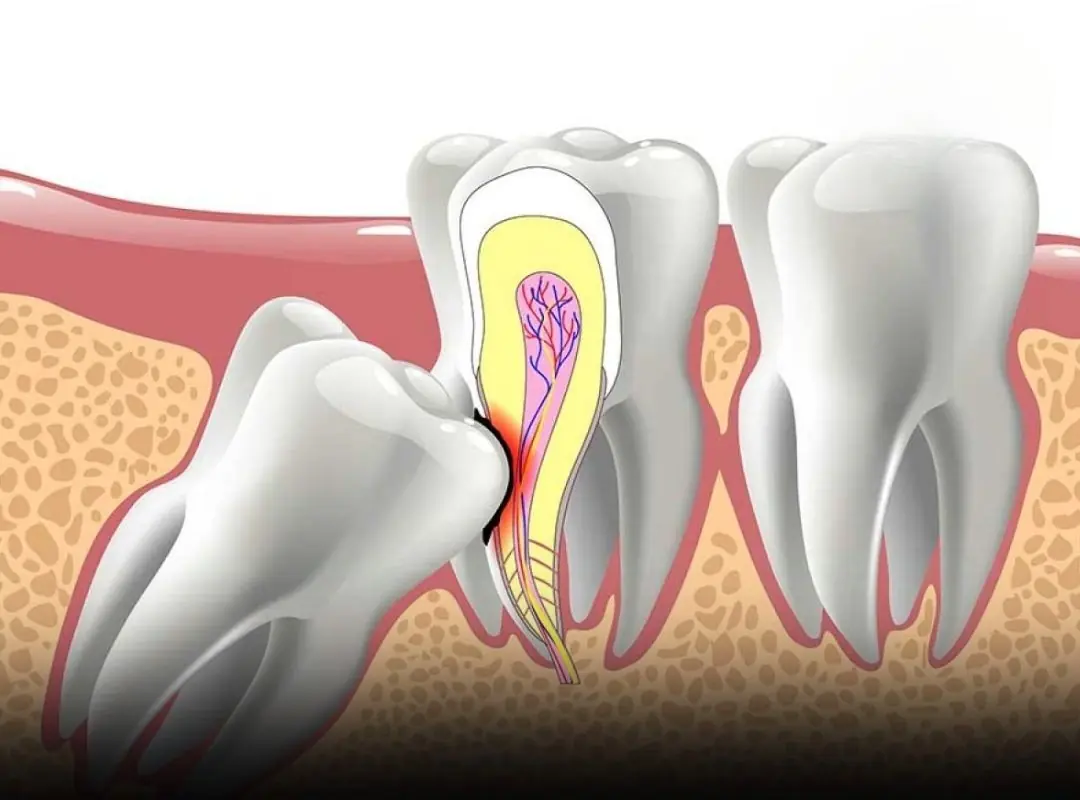
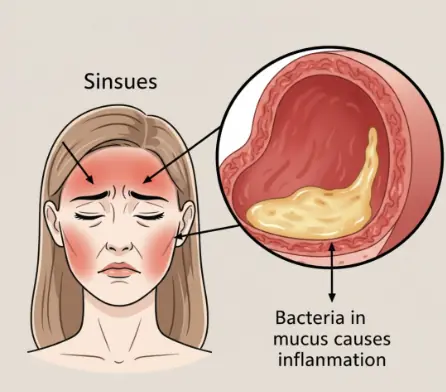
3. Frequent Infections or Delayed Recovery
The immune system weakens over time.
Recurring infections such as:
-
Pneumonia
-
Urinary tract infections
-
Skin infections
may appear closer together and take longer to resolve. Hospitalizations may become more frequent.
In many elderly individuals, infection becomes a major complicating factor in the final year of life.
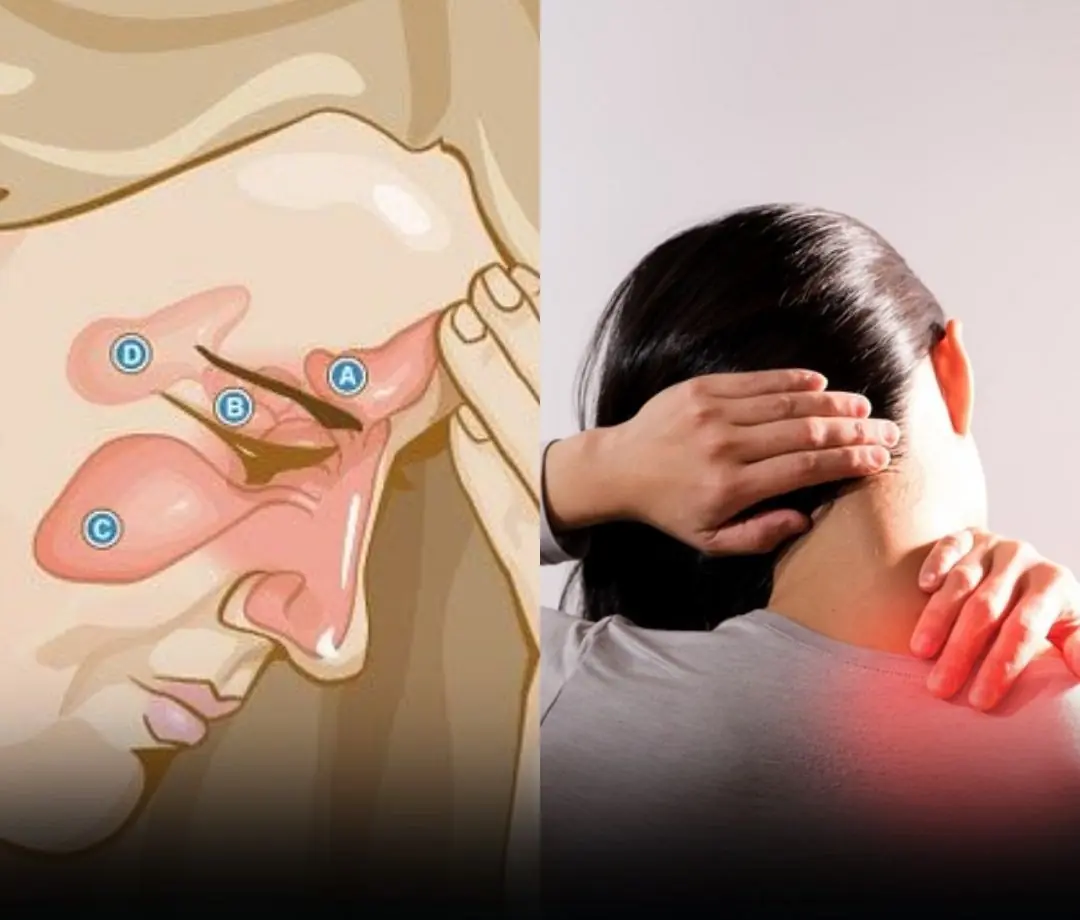
4. Cognitive Changes and Increased Confusion



Mental clarity can fluctuate.
Common signs include:
-
Disorientation
-
Memory lapses
-
Hallucinations
-
Withdrawal
This may result from reduced brain perfusion, medication effects, metabolic imbalance, or neurodegenerative disease progression.
Episodes of delirium are particularly common in advanced illness.
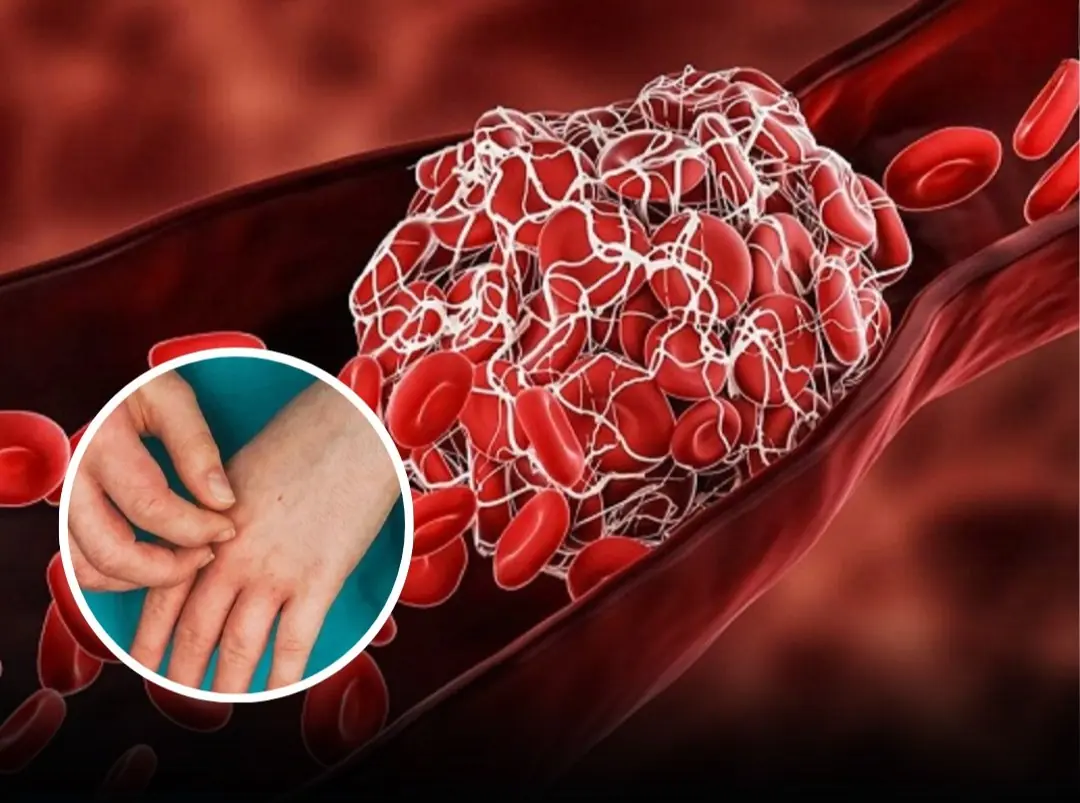
5. Shortness of Breath and Circulatory Changes
Breathing patterns may gradually change months before death.
Indicators include:
-
Increased breathlessness
-
Shallow breathing
-
Reduced tolerance for activity
-
Swelling in extremities
Circulation may weaken, leading to cold hands and feet or visible bruising due to fragile blood vessels and low platelet function.
As cardiac output declines, tissues receive less oxygen.
6. Decreased Social Engagement and Emotional Withdrawal



Many individuals naturally withdraw in their final year.
This can appear as:
-
Reduced conversation
-
Limited interest in visitors
-
Increased reflection
-
Desire for quiet
From a psychological perspective, this withdrawal is not always depression. It can represent a natural transition phase, where the body and mind gradually reduce external engagement.
Important Clarification
These signs do not automatically mean someone will die within a year.
They are more commonly observed in:
-
Advanced cancer
-
End-stage heart failure
-
Severe COPD
-
Late-stage dementia
-
Advanced kidney disease
Prognosis depends heavily on diagnosis, treatment, and overall health status.
Medicine cannot predict exact timelines with precision. Even experienced clinicians rely on functional decline patterns rather than specific dates.
When to Seek Medical Attention
Immediate evaluation is warranted if there are:
-
Sudden severe breathing difficulty
-
Rapid mental status changes
-
Severe unexplained weight loss
-
Persistent uncontrolled pain
-
Repeated infections
Early palliative care consultation can significantly improve quality of life—even when life expectancy is uncertain.
A Compassionate Perspective
The human body does not abruptly shut down. It gradually shifts priorities. Systems slow. Energy narrows. Functions reduce.
Understanding these patterns helps families prepare, plan care appropriately, and focus on comfort rather than crisis.
Open discussion with healthcare providers is not pessimism—it is preparation.
Awareness brings clarity.
Clarity allows dignity.