Can a Husband’s Habits Affect His Wife’s Breast Can.cer Risk?
A viral headline paired with a couple-in-bed illustration warns: “These 2 habits in men could raise their wives’ breast cancer risk.” It’s an attention-grabbing claim—and like many health headlines online, it needs context.
Breast cancer risk is shaped by many factors: genetics, age, hormones, reproductive history, body weight, alcohol use, physical activity, and more. A partner can’t “cause” breast cancer by default. However, shared environments and shared lifestyle routines can influence long-term health. That’s where certain household habits—especially those that increase exposure to toxins or make unhealthy routines feel “normal”—may matter.
Below are two habits that experts commonly flag as potentially harmful in a family setting, along with safer alternatives.
Habit #1: Smoking Around the Home (Secondhand Smoke Exposure)
If a husband smokes indoors, in the car, or near family members, he may expose his partner to secondhand smoke—a mixture of toxic chemicals linked to multiple health harms. While the strongest cancer link is with lung cancer, secondhand smoke also contributes to chronic inflammation and DNA damage, which are processes involved in many diseases.
Why it can matter for women’s health
-
Secondhand smoke may increase overall cancer risk and heart disease risk.
-
It can worsen respiratory issues, reduce sleep quality, and increase stress on the body.
-
Some studies have explored whether secondhand smoke is associated with breast cancer risk, with mixed results—but many health organizations still recommend avoiding exposure because the smoke contains known carcinogens.
What families can do
-
Make the home and car 100% smoke-free.
-
If quitting isn’t immediate, set strict rules: smoke outside, far from windows/doors, and never in shared spaces.
-
Consider cessation support (counseling, nicotine replacement, or physician-guided plans).
The key point: even if the breast cancer connection isn’t as direct as some headlines suggest, reducing secondhand smoke is a clear win for the whole household.
Habit #2: Creating a “High-Risk Lifestyle” at Home (Alcohol + Poor Diet + Sedentary Routine)
Breast cancer risk is strongly influenced by lifestyle—especially alcohol intake and body weight (particularly after menopause). A husband’s habits may raise risk indirectly if they shape the household routine: frequent drinking nights, calorie-heavy meals, late sleeping patterns, and low activity weekends.
Why it can matter
-
Alcohol: Even moderate drinking is linked with higher breast cancer risk. If a partner’s routine normalizes frequent drinking, it may increase the likelihood that the other partner drinks more often too.
-
Weight gain and inactivity: A sedentary lifestyle and long-term weight gain can affect hormones and inflammation—factors associated with breast cancer risk. When couples share meals, schedules, and stress patterns, they often share these risks.
What families can do
-
Choose alcohol-light routines: fewer “drinking default” evenings, more alcohol-free days.
-
Build “couple habits” that protect health: 30-minute walks, weekend sports, home-cooked meals, and consistent sleep times.
-
Make small swaps that stick: replace sugary drinks, add fiber-rich foods, and plan protein/vegetables first.
This isn’t about blaming one person. It’s about recognizing that health behaviors spread through relationships, for better or worse.
What the Viral Headlines Get Wrong
Many posts imply a direct cause-and-effect: “Men do X → Women get breast cancer.” Real life is more complicated. Breast cancer is not usually triggered by one habit alone. Instead, it’s often the result of risk stacking over years: exposure + hormones + lifestyle + genetics + chance.
A better way to interpret the claim is this: a partner’s habits can raise or lower the household’s overall risk environment.
When to Focus on Screening (Not Just Habits)
Lifestyle matters—but screening saves lives. Women should follow local guidelines for:
-
routine clinical checkups
-
mammography schedules based on age and risk
-
earlier screening if there’s a strong family history or genetic risk
If someone notices a new lump, nipple changes, skin dimpling, persistent pain, or unusual discharge, it’s worth seeing a clinician promptly.
News in the same category

Doctors “Reveal” Morning Coffee Causes… What’s the Real Story?

A Stroke Doesn’t Give You a Second Chance: 6 Things You Must Do — and 3 De.adly Mistakes to Avoid

Not all cheap fish is a bargain: six kinds you may want to skip.

If people knew the real risk, they’d think twice before reheating leftover rice.

Some can.cers start quietly. If you spot these eight toilet-time symptoms, don’t delay a doctor visit

These factors can be the cause of c.o.lon ca.ncer that you may not notice in your daily routine

5 Diseases Linked to Dry Mouth and Thirst in the Middle of the Night
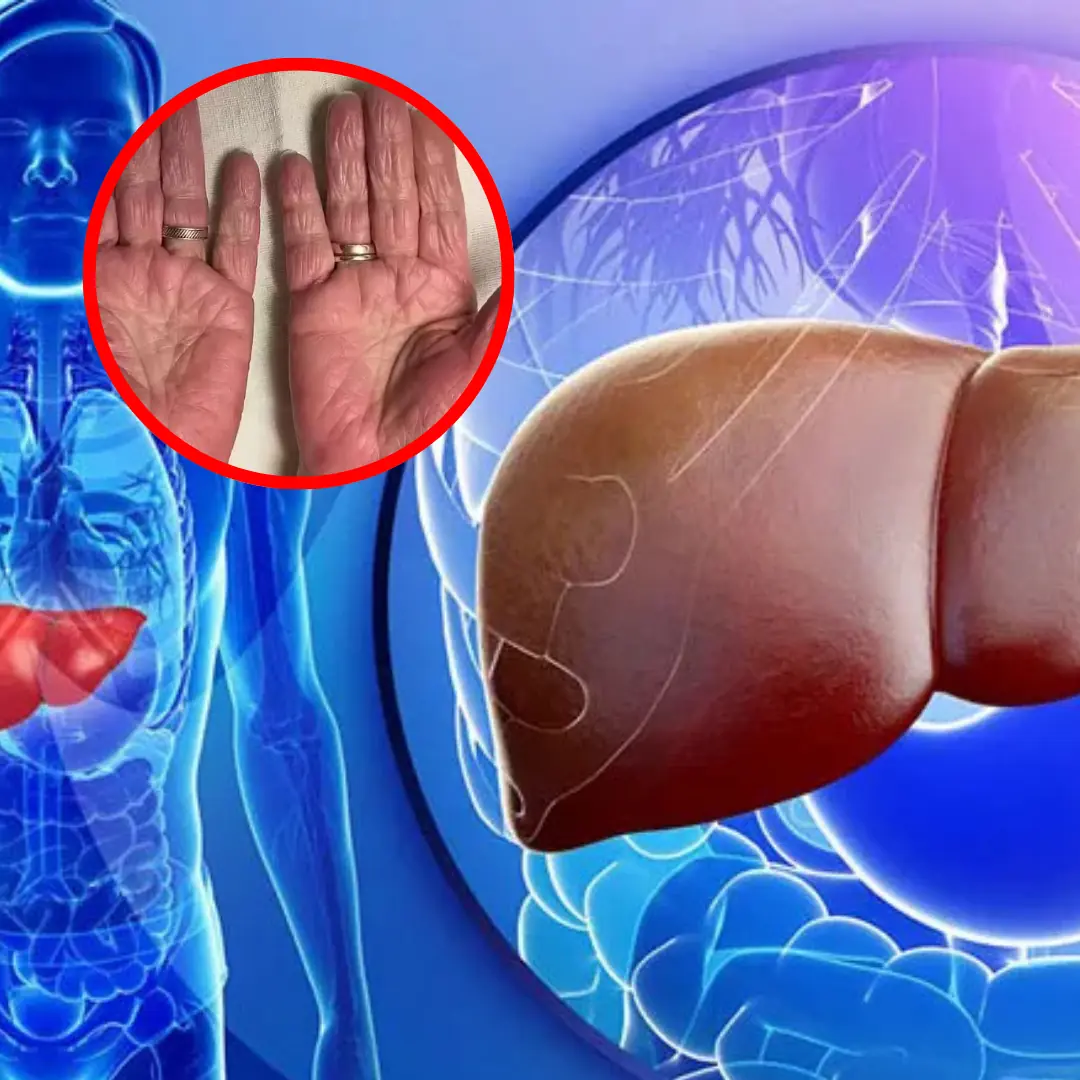
People with liver failure often have 3 characteristics on their hands, if you have 1 you should see a doctor soon
If you notice these 10 symptoms this morning, don't ignore them - you might have diabetes without realizing it

Lymphoma survivors share six symptoms they experienced before diagnosis

“I Warned Her So Many Times”: A 26-Year-Old’s Diagnosis Sparks a Wider Conversation About Women’s Health

Today, my throat feels completely clear — right after this little thing came out. What was it?

Orange Dreamsicle Salad

The Stone Breaker Plant: Nature’s Remedy for Kidney Stones

A Scientific Look at Oregano’s Role in Supporting Wellness
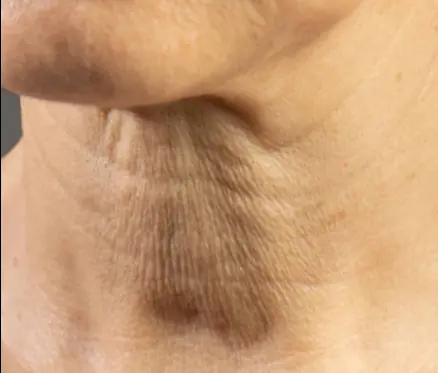
If your neck is starting to sag, don’t ignore it. This is why it happens

“I Di3d for 6 Minutes and Saw the Afterlife — What I Witnessed Still Haunts Me”

If You Have These Two "Dimples" on Your Lower Back, Here's What They Mean
News Post
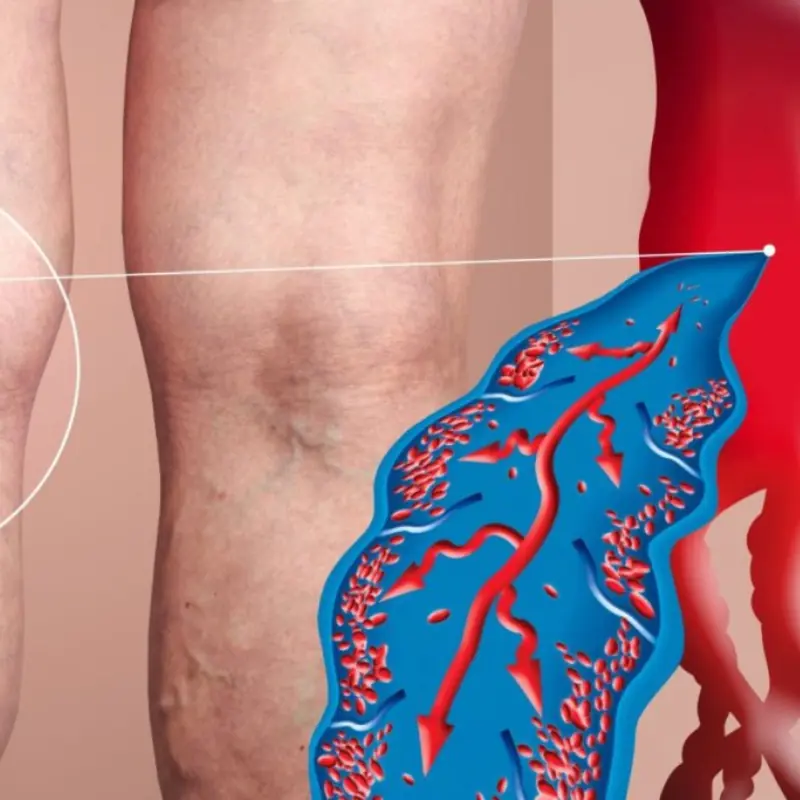
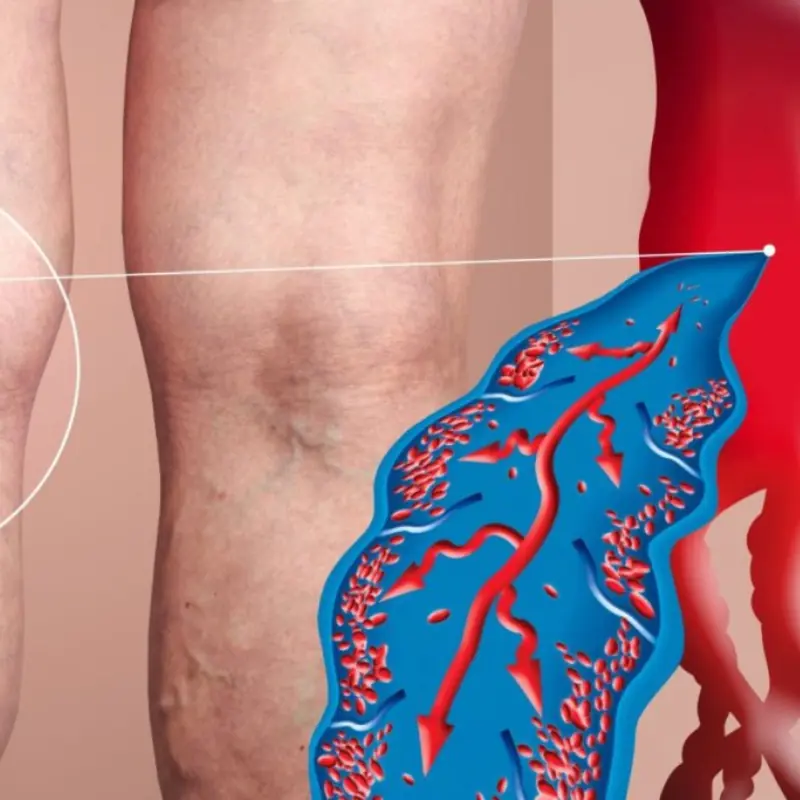
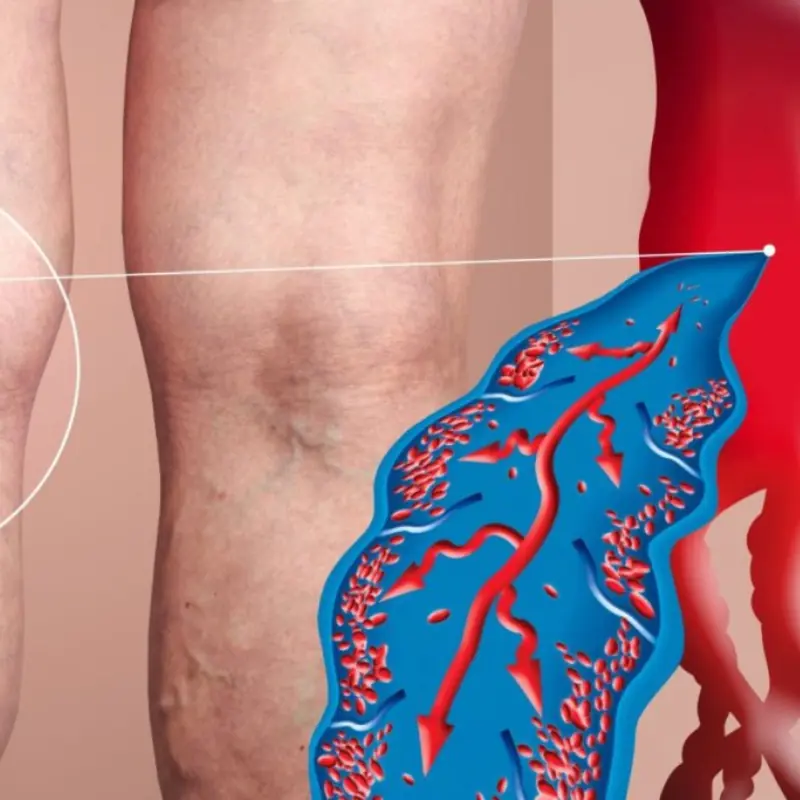
If You Have Poor Circulation, Cold Feet or Varicose Veins, Start Doing these 6 Things

Classic Oven-Roasted Chicken

Doctors “Reveal” Morning Coffee Causes… What’s the Real Story?

Fresh Fruit & Cucumber Salad

A Stroke Doesn’t Give You a Second Chance: 6 Things You Must Do — and 3 De.adly Mistakes to Avoid

Roasted Vegetable Stack

Avocado & Green Vegetable Tower

Pan-Seared Duck Breast

Creamy Peppercorn Steak (Restaurant-Style)

Not all cheap fish is a bargain: six kinds you may want to skip.

If people knew the real risk, they’d think twice before reheating leftover rice.

Some can.cers start quietly. If you spot these eight toilet-time symptoms, don’t delay a doctor visit

These factors can be the cause of c.o.lon ca.ncer that you may not notice in your daily routine

5 Diseases Linked to Dry Mouth and Thirst in the Middle of the Night
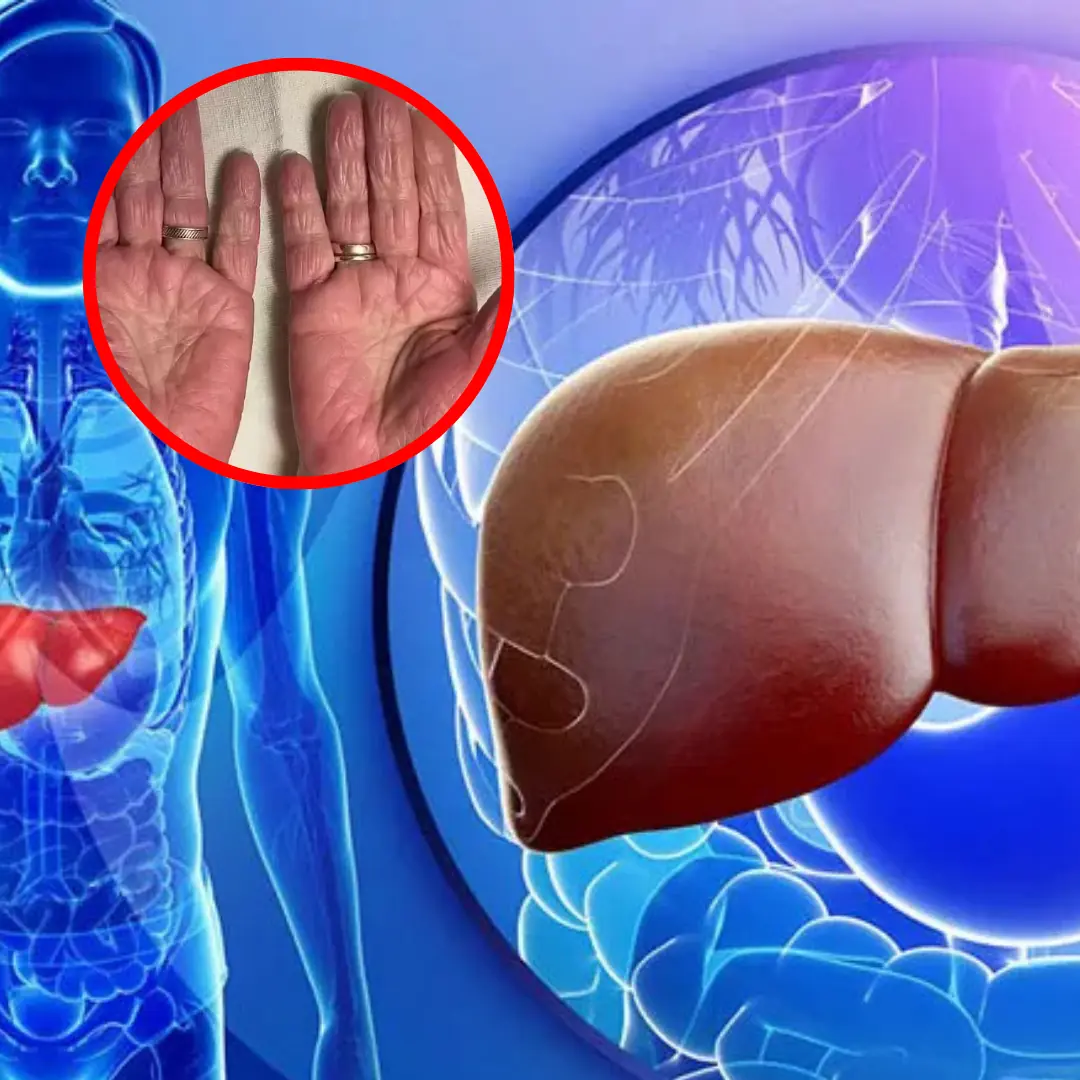
People with liver failure often have 3 characteristics on their hands, if you have 1 you should see a doctor soon

Why Your Phone Works Differently in Europe (And What They’re Not Telling You)
If you notice these 10 symptoms this morning, don't ignore them - you might have diabetes without realizing it

Lymphoma survivors share six symptoms they experienced before diagnosis

“I Warned Her So Many Times”: A 26-Year-Old’s Diagnosis Sparks a Wider Conversation About Women’s Health
