Four Signs a Parent May Be Nearing the Final Stage of Life—and How to Prepare
The image is quiet but heavy: two hands clasped tightly at the bedside, a loved one blurred in the background. It reflects a moment many families recognize—when you start asking not only “How do we help?” but also “What happens next?” The text on the image offers a difficult truth: if your parent shows four signs, they may be approaching the final stage of life. While no checklist can predict an exact timeline, certain changes are common as the body begins to slow down.
This article explains four widely recognized signs seen in many people during advanced illness or frailty, and outlines gentle, practical steps families can take to prepare—without panic, and with compassion.
Sign 1: Rapid decline in eating and drinking
One of the most common changes near the end of life is a marked decrease in appetite and thirst. Your parent may eat only a few bites, refuse favorite foods, or have trouble swallowing. Families often fear their loved one is “starving,” but in many cases the body is naturally conserving energy as organ systems slow.
What to do:
-
Offer small sips, ice chips, or mouth swabs if safe, focusing on comfort rather than calories.
-
Keep lips moist with balm and maintain oral care to reduce dryness.
-
Ask the medical team about swallowing safety and whether thickened liquids are needed.
Sign 2: Increasing sleep and reduced responsiveness
As the body weakens, many people sleep more, speak less, and respond slowly. Your parent may drift in and out of awareness or seem “far away.” This can be emotionally painful for families who want reassurance or final conversations, but it is often part of the natural shutting down process.
What to do:
-
Continue speaking softly—hearing may remain even when responses fade.
-
Create a calm environment: low light, familiar voices, gentle music if comforting.
-
Share important words early: gratitude, love, forgiveness, reassurance.
Sign 3: Changes in breathing patterns
Breathing can shift noticeably in the final stage. You might see irregular breathing, long pauses, rapid shallow breaths, or a pattern that alternates between fast and slow. Some people develop noisy breathing from secretions in the throat (often called a “death rattle”), which can sound distressing even when the person is not suffering.
What to do:
-
Reposition the person slightly on their side, elevate the head, and keep airways comfortable.
-
Ask the care team about medications that may reduce secretions or ease breathlessness.
-
If breathing changes suddenly or seems painful, contact medical support promptly.
Sign 4: Cooling skin, mottling, and circulation changes
When circulation slows, hands and feet may feel cool, and the skin can show mottling—patchy, purplish or bluish areas, often on the legs and feet. Pulse and blood pressure may drop. This is a physical sign that the body is prioritizing core organs and gradually shutting down.
What to do:
-
Use light blankets for warmth (avoid electric heating pads unless advised).
-
Keep the person comfortable with gentle touch and soft clothing.
-
Treat these changes as cues to increase support and presence.
How to prepare: practical steps that help families
Recognizing signs is only part of the story. Preparation can reduce fear and help you protect your parent’s comfort and dignity.
1) Talk to the care team—early and clearly
Ask direct questions:
-
“What changes should we expect next?”
-
“What symptoms mean we should call you right away?”
-
“Is hospice or palliative care appropriate now?”
Hospice and palliative services can provide pain control, nursing support, and guidance for families—often improving comfort and reducing unnecessary hospital trips.
2) Focus on comfort, not force
Near the end of life, the goal often shifts from “fixing” to relieving suffering. Pain, anxiety, nausea, constipation, and shortness of breath can usually be managed. If your parent is no longer eating, it is not always a sign of neglect—it can be a natural progression.
3) Prepare the home and routines
Small changes can make a big difference:
-
Keep essential medications and contact numbers visible.
-
Create a bedside kit: tissues, gloves, wipes, lip balm, water swabs, spare linens.
-
Arrange family shifts so no one caregiver is overwhelmed.
4) Handle key legal and logistical items
If possible, ensure documents are in place: healthcare proxy, advance directive, Do Not Resuscitate (DNR) status if desired, and a list of medications and diagnoses. Discuss preferences about where your parent wants to be—home, hospice facility, or hospital—if choices exist.
5) Take care of yourself, too
Holding a parent’s hand through decline is emotionally and physically demanding. Accept help, rest when you can, and consider grief counseling or support groups. Being present does not mean doing everything alone.
News in the same category

A woman who ate steamed sweet potatoes daily was shocked by her liver test results—what went wrong?
Daily sweet potatoes shocked her liver tests—here’s what may explain it

If you frequently hear ringing in your ears, it could be a warning sign of an underlying health issue.
Persistent ear ringing may signal hidden health problems you shouldn’t ignore
Experts warn: One common mistake is causing mold in spices in most households
Experts reveal the main cause of mold in spices - Most homes are storing them incorrectly

What time should you take a bath to ensure health safety and reduce the r.isk of stro.ke?
What time should you take a bath to ensure health safety and reduce the r.isk of stro.ke?

The health benefits of eating boiled sweet potatoes for breakfast
Eating boiled sweet potatoes for breakfast: The changes you may notice over time
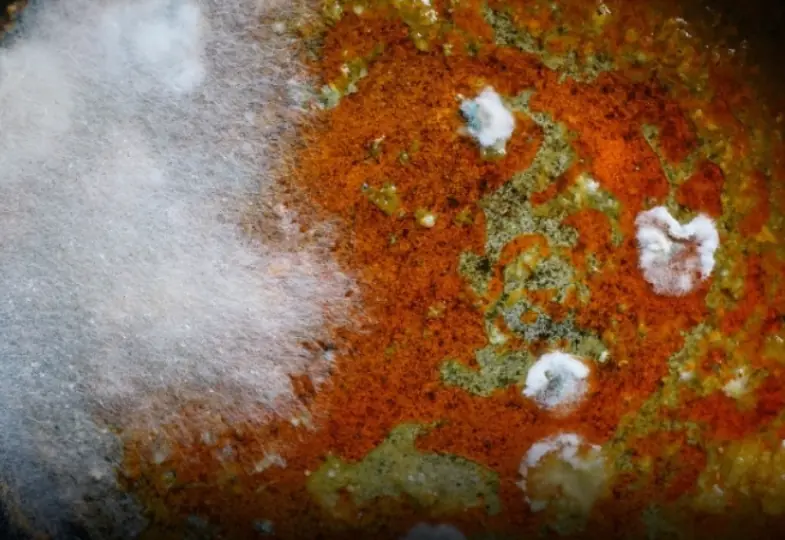
Doctors Say Healthy Kidneys Are Unlikely to Show These 3 Skin Signs
Doctors Say Healthy Kidneys Are Unlikely to Show These 3 Skin Signs

5 warning signs that may indicate advanced liver dis.ease
5 alarming signs your liver could be in serious trouble - Don’t ignore them

The health benefits of sleeping on your left side
Why you should try sleeping on your left side?

A warning sign of stroke can appear up to 90 days before it happens
A warning sign of st.ro.ke can appear up to 90 days before it happens

Beet benefits: What doctors say happens when you eat them?
Health benefits of beets: What doctors say they do to your body?

Experts reveal 5 symptoms of cancer that are easy to ignore but you really shouldn't
Experts reveal 5 symptoms of cancer that are easy to ignore but you really shouldn't

Two itchy areas on the body may be signs of liv.er can.cer, often mistaken for allergies

A woman ate steamed sweet potatoes daily - Her liver test results came as a sh.ock
She ate steamed sweet potatoes every day. Then, the results of her liver tests surprised her

What Really Happens To Your Body When You Eat A Banana Every Day
The Effects of Daily Banana Consumption on the Human Body

5 early warning signs of thyroid can.cer you should know
5 early signs of thyroid can.cer you shouldn’t ignore

20-Year-Old Teacher Dies from Liver Cancer: Doctor Warns That Odor in 3 Body Areas Could Signal a Failing Liver
20-Year-Old Teacher Dies from Liver Cancer: Doctor Warns That Odor in 3 Body Areas Could Signal a Failing Liver

What's Behind the Purple Color in Your Feet? Causes You Shouldn't Ignore

A Family of Four Diagnosed With Liver Can:cer: Experts Identified the Cause the Moment They Entered the Kitchen
News Post
My Kid.neys Were in Dan.ger – Here’s What I Took to Realize the Truth

A woman who ate steamed sweet potatoes daily was shocked by her liver test results—what went wrong?
Daily sweet potatoes shocked her liver tests—here’s what may explain it

If you frequently hear ringing in your ears, it could be a warning sign of an underlying health issue.
Persistent ear ringing may signal hidden health problems you shouldn’t ignore
Experts warn: One common mistake is causing mold in spices in most households
Experts reveal the main cause of mold in spices - Most homes are storing them incorrectly

What time should you take a bath to ensure health safety and reduce the r.isk of stro.ke?
What time should you take a bath to ensure health safety and reduce the r.isk of stro.ke?

Why clove, lemon and onion work so well together for health and home
The combined health and household benefits of clove, lemon and onion

Steak & Shrimp Garlic Bread Boat (Surf and Turf Style)

Creamy Beef & Mushroom Skillet

Berry Choux Cream Cake

The health benefits of eating boiled sweet potatoes for breakfast
Eating boiled sweet potatoes for breakfast: The changes you may notice over time

Sticky Spicy Glazed Meatballs

Red Wine Braised Beef Short Ribs with Creamy Mashed Potatoes

Crispy Spicy Glazed Pork Belly (Asian-Style)

The hidden purpose behind the lines on bath towels
What do the lines on bath towels actually mean?
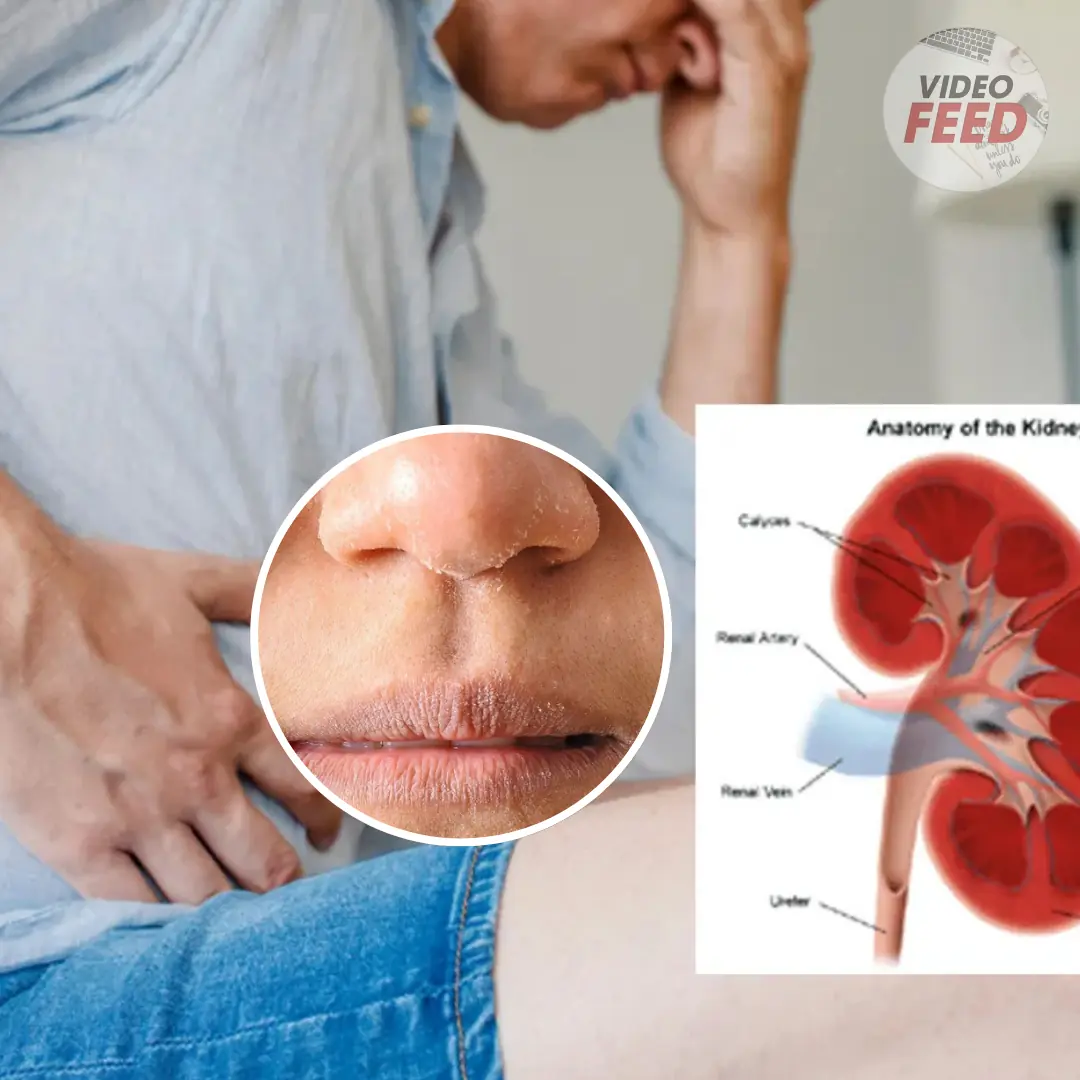
Doctors Say Healthy Kidneys Are Unlikely to Show These 3 Skin Signs
Doctors Say Healthy Kidneys Are Unlikely to Show These 3 Skin Signs

Slow-Braised Beef Shank (Osso Buco–Style)

5 warning signs that may indicate advanced liver dis.ease
5 alarming signs your liver could be in serious trouble - Don’t ignore them

Sticky BBQ Pork Ribs (Tender, Juicy, Fall-Off-The-Bone)

The health benefits of sleeping on your left side
Why you should try sleeping on your left side?