
Warning signs: Persistent itching and small bumps on your skin may signal a hidden problem

Surprising Causes of Hives Revealed — What May Be Triggering Your Skin Reaction
Hives (urticaria) are red, itchy welts that can appear suddenly on the skin. While allergies are a well-known cause, doctors say many cases of hives are triggered by less obvious factors. Here are some scientifically recognized but often overlooked causes of hives, along with what you can do about them.
1. Sudden Temperature Changes
Why it happens:
Rapid changes in temperature—such as stepping into a hot shower, exposure to cold air, or sweating during exercise—can trigger physical urticaria, including cold urticaria or heat-induced urticaria. These conditions occur when temperature changes stimulate mast cells in the skin to release histamine.
What you can do:
Avoid sudden exposure to extreme heat or cold. Gradually acclimate your body to temperature changes and wear appropriate protective clothing.
2. Tight Clothing or Skin Friction
Why it happens:
Pressure or repeated friction from tight waistbands, bras, or backpack straps can cause dermatographism (also called “skin writing”), a common form of physical hives where raised welts appear after minor skin irritation.
What you can do:
Choose loose-fitting, breathable fabrics and reduce prolonged pressure on sensitive areas.
3. Sunlight Exposure
Why it happens:
Some people develop solar urticaria, a rare condition in which exposure to sunlight causes itchy, red welts within minutes.
What you can do:
Use broad-spectrum sunscreen, wear protective clothing, and limit sun exposure during peak hours.
4. Exercise or Sweating
Why it happens:
Exercise, sweating, or emotional stress can raise body temperature and trigger cholinergic urticaria, characterized by small, itchy hives.
What you can do:
Exercise in cooler environments, stay hydrated, and wear moisture-wicking clothing.
5. Certain Foods (Without a True Allergy)
Why it happens:
Even without a diagnosed food allergy, some foods may worsen hives by increasing histamine levels or releasing histamine in the body. Common triggers include:
-
Histamine-rich foods (aged cheese, fermented foods, alcohol, processed meats)
-
Food additives (preservatives like sulfites, artificial colors, MSG)
What you can do:
Keep a food diary to identify patterns and consider an elimination diet under medical guidance.
6. Infections — Even Mild Ones
Why it happens:
Viral or bacterial infections (such as colds, urinary tract infections, or dental infections) can stimulate the immune system and trigger hives, especially in children.
What you can do:
Treat underlying infections promptly. If hives recur frequently with infections, consult a doctor.
7. Contact With Water (Rare)
Why it happens:
A very rare condition called aquagenic urticaria causes hives after contact with water, regardless of temperature. The exact mechanism remains unclear.
What you can do:
Consult a dermatologist for diagnosis and treatment. Avoid harsh soaps and use gentle skincare products.
8. Hormonal Changes
Why it happens:
Hormonal fluctuations—during menstruation, pregnancy, or menopause—may influence immune responses and worsen hives in some women.
What you can do:
Track symptoms alongside hormonal changes and discuss persistent issues with a healthcare provider.
9. Unexpected Medication Triggers
Why it happens:
Certain medications can provoke hives even without a classic allergic reaction. Common examples include:
-
Aspirin and other NSAIDs
-
Blood pressure medications (such as ACE inhibitors)
-
Some herbal supplements
What you can do:
Review all medications with your doctor. Stop or switch medications only under medical supervision.
10. Hidden Environmental Irritants
Why it happens:
Fragrances, detergents, cleaning products, pollen, and dust mites can irritate sensitive skin and contribute to hives.
What you can do:
Use fragrance-free, hypoallergenic products and rinse clothes thoroughly after washing.
11. Autoimmune Conditions

Why it happens:
Chronic hives lasting longer than six weeks may be linked to autoimmune disorders, where the immune system mistakenly activates skin mast cells.
What you can do:
Seek evaluation from a dermatologist or allergist. Blood tests may be recommended.
Conclusion
Hives are not always caused by allergies alone. Temperature changes, friction, sunlight, infections, hormones, medications, and even water can all play a role. Identifying your personal triggers is key to managing symptoms effectively. If hives persist, recur frequently, or last longer than six weeks, professional medical evaluation is essential.
News in the same category


If Your Parent Shows These 3 Signs, They May Be Nearing the End of Life. Prepare Yourself for What’s to Come

Can you eat leftover rice safely? Here’s what nutrition experts say

For those who are in the habit of poking the leg out of the bed sheet when sleeping
Health Warning: 4 Types of Electric Kettles You Should Stop Using Immediately

This type of "poiso,nous sandal" can cause early puberty in children, but many parents still buy it for their children to wear!

With this leaf in hand, you don't have to worry about diarrhea or health problems will improve

Don’t Drink Water Immediately After Waking Up: Doctors Reveal 5 Important Things to Do First

A 106-Year-Old Woman Reveals a Zero-Cost Secret to Longevity — And It’s Not Exercise or Dieting

Why Are My Veins Suddenly Bulging and Visible?

Just follow these 4 steps and pork will always turn out tender, juicy, and never tough
Mix White Salt With Fabric Softener: A Simple Household Trick That Saves Money and Solves Multiple Problems

Installing an Air Conditioner: Avoid These 4 Locations to Protect Your Family’s Health

Don’t Throw Away Rice-Washing Water: 5 Surprisingly Useful Kitchen Benefits

Why should garlic be placed at the head of the bed when sleeping at night?

Cook rice better just this

Remove this from your room immediately!! Lung can.cer!

Why Should Couples Over 50 Consider Sleeping in Separate Beds? Those Who’ve Experienced It Share 3 Key Benefits
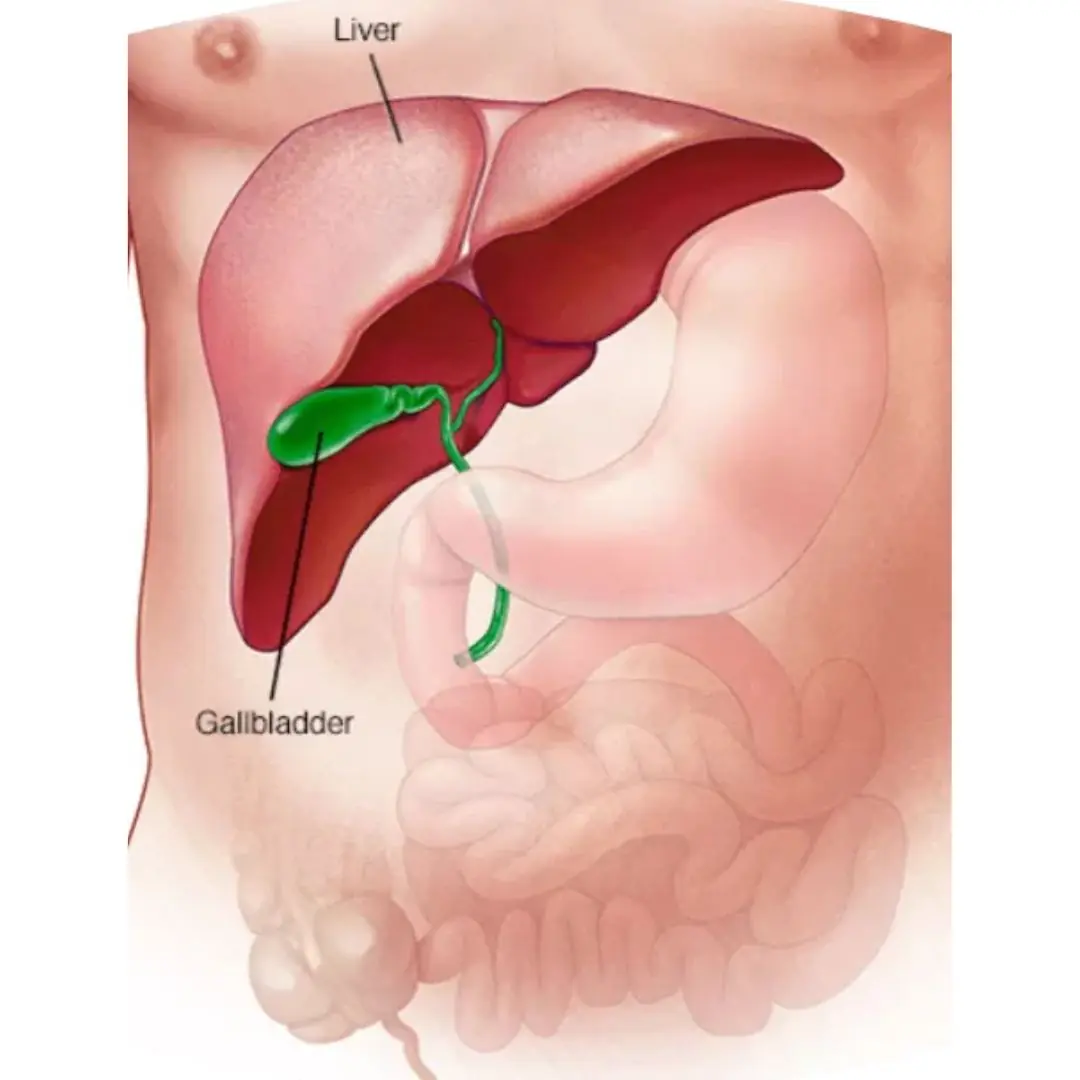
Gallbladder removal: what happens next and 3 risks to watch for
News Post

10+ Warning Signs You're Eating Too Much Sugar

Why you should never pour household wastewater into the toilet?

When coffee becomes too much: 7 warning signs your body is asking you to stop

If Your Parent Shows These 3 Signs, They May Be Nearing the End of Life. Prepare Yourself for What’s to Come

The ring you pick will reveal your truest trait

Can you eat leftover rice safely? Here’s what nutrition experts say
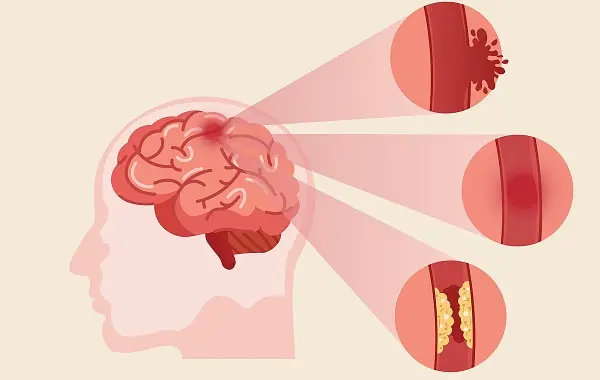
Br.ain aneu.rysm: Warning signs, emergency symptoms and How to reduce your risk
The right way to clean your refrigerator’s rubber door seal

Numb hands: Is it normal or a sign of a deeper problem?

5 Potential Risks of Eating Avocados You Should Know

Drinking Coffee at the Right Time May Support Heart Health, Experts Say
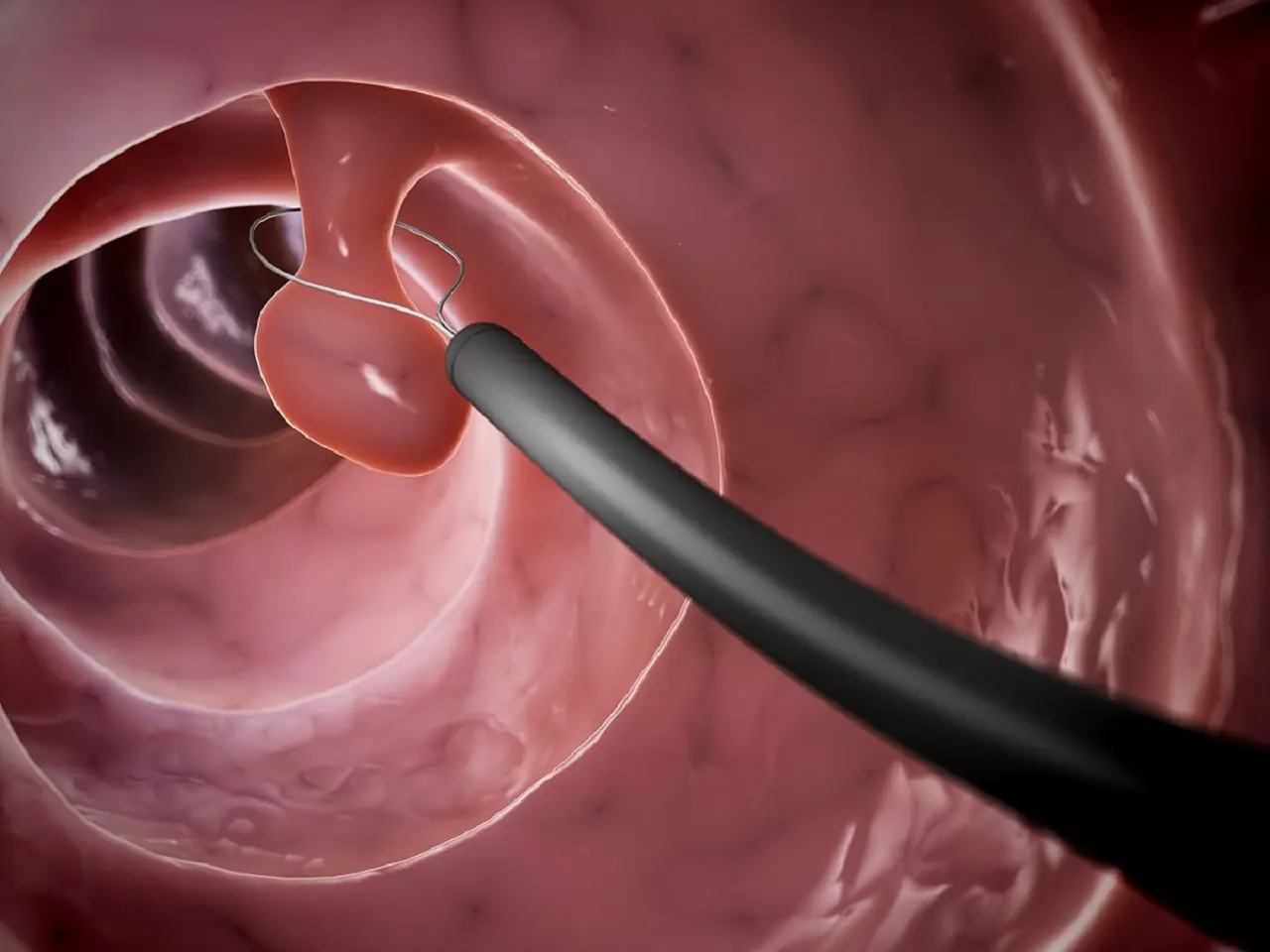
Early detection of colon polyps: The key to effective cancer prevention

For those who are in the habit of poking the leg out of the bed sheet when sleeping

Warning Signs That Cancer Is Growing in Your Body
Health Warning: 4 Types of Electric Kettles You Should Stop Using Immediately

The Back of Your Hand May Reveal Longevity Secrets: 4 Signs Everyone Should Check

More Than 90% of iPhone Users Don’t Know the Purpose of the Tiny Hole Next to the Camera

Doctors recommend a vegetable that supports the heart, fights aging, has 7x more calcium than bone broth, and is easy to find at the market.
